
Observation on therapeutic effect of stereotactic soft channel puncture and drainage on hypertensive cerebral hemorrhage
Introduction
Hypertensive cerebral hemorrhage is a disease with high incidence, high mortality, large amount of bleeding and high disability rate. More than 40% of stroke patients are caused by hypertensive cerebral hemorrhage (1,2). Recent studies showed that the incidence of male is higher than that of female, and it mostly occurs in patients aged 50–60 years, but in recent years, the disease tends to occur in young patients (3). For the treatment of hypertensive intracerebral hemorrhage, the main treatment principle is to clear the hematoma as soon as possible, reduce the intracranial pressure, and improve the prognosis of patients (4). Although conservative treatment of clinical drugs can clear the hematoma to a certain extent, but the absorption of efficacy is slow. Conventional craniotomy can clear the hematoma in a short time, but it has a high risk of surgery and more postoperative complications (5-7). At present, with the improvement of medical technology, minimally invasive medicine has been rapidly developed and applied. Many hospitals have adopted stereotactic soft channel puncture and drainage to treat hypertensive cerebral hemorrhage, and achieved satisfactory results, effectively improving the treatment rate and quality of life of hypertensive cerebral hemorrhage patients (8-10). In our hospital, 60 patients with hypertensive cerebral hemorrhage from September, 2014 to September, 2019 were treated with stereotactic soft channel puncture and drainage, and the report is as follows.
Methods
General information
Sixty patients with hypertensive cerebral hemorrhage admitted to our hospital from September 2014 to September 2019 were selected for study and randomly divided into study group (n=30) and routine group (n=30) according to admission number. Institutional review board approval with consent waiver was obtained for this retrospective study. In the routine group, the ratio of male to female was 20:10. The upper limit of age was 65 years old and the lower limit of age was 48 years old, the average was 57.19±3.65 years old. There were 13 cases of basal ganglia hemorrhage, 7 cases of thalamus hemorrhage, 5 cases of lobar hemorrhage, 5 cases of cerebellum hemorrhage, and the average amount of hemorrhage was 46.13±10.73 mL. In the observation group, the ratio of male to female was 19:11. The upper limit of age was 64 years old, the lower limit of age was 50 years old, and the average was 57.18±3.69 years old. There were 14 cases of basal ganglia hemorrhage, 8 cases of thalamus hemorrhage, 4 cases of lobar hemorrhage, 4 cases of cerebellum hemorrhage, and the average amount of hemorrhage was 46.09±11.06 mL. There was no statistical difference between the two groups in terms of the gender, age, bleeding site and average bleeding volume, which was worth studying (P>0.05).
Research acceptance and exclusion principles
Acceptance principle: (I) the study obtained the consent of the hospital ethics committee and the patient’s family members, and the patient’s family members signed the relevant informed consent with the hospital voluntarily, (II) all patients were diagnosed as hypertensive cerebral hemorrhage by CT, (III) the patient has a history of hypertension, (IV) in accordance with the indications of stereotactic soft channel puncture and drainage, (V) follow up for half a year.
Exclusion principle: (I) Incomplete information, (II) patients with abnormal coagulation, (III) brain herniation, (IV) brain stem failure, (V) other causes of cerebral hemorrhage, (VI) patients with severe organ (heart, kidney, liver, etc.) dysfunction, (VII) operation contraindications.
Therapeutic methods
Both groups received basic treatment such as red blood, reducing intracranial pressure and nourishing neurons.
Removal of hematoma from small bone window (11)
Brain CT examination was performed before operation, and general anesthesia was given to patients with tracheal intubation. The approach of operation was frontotemporal top of hematoma side. After the formation of bone flap, the dura mater was suspended and opened, and the arachnoid membrane of lateral fissure was separated to the completely exposed guide vane. Hematoma was punctured by brain puncture needle, and then the hematoma was entered along the puncture channel and sucked out by suction device. In this process, it is not allowed to forcibly scrape off the small blood clots and hematoma wall at the bottom to avoid further bleeding. The hematoma was cleaned with normal saline, the drainage tube was left after the liquid was clear, and the skull was closed.
Stereotactic soft channel puncture and drainage (12)
Before operation, CT examination was performed to identify the hematoma site. After local anesthesia, the projection area of the scalp at the largest level of the hematoma was used as the puncture point, avoiding important functional areas and large blood vessels. The syringe with drainage device was inserted into the hematoma cavity from the bone hole with a vertical long axis or according to the long axis of the hematoma. The core of the needle was pulled out after the blood was found with the aid of silica gel tube. Push the drainage tube 1–3 cm and fix it. After aspirating hematoma, connect tee head to maintain drainage. Brain CT was reexamined 24 hours after the operation. Normal saline and urokinase were injected according to the amount of residual hematoma. The catheter was removed within 5–10 days after the operation.
Evaluation criterion
Therapeutic effect
After treatment, the hematoma was cleared completely, the level of nerve defect was reduced by more than 90%, and the independent living ability was improved by more than 90%. No complications occurred after operation, which can be regarded as remarkable treatment effect; After treatment, the hematoma was basically cleared completely, the level of nerve defect was reduced by more than 60–89%, the independent living ability was improved by more than 60–89%, and the postoperative complications were less, which could be regarded as effective treatment. After treatment, the hematoma was not cleared completely, the level of nerve defect was reduced by 59%, and the independent living ability was improved by 59%. There were many complications after operation, which could be regarded as invalid treatment (13).
Neurological deficit level
The degree of neurological deficit in stroke (China Stroke Scale, CSS) was evaluated. The total score of the scale is 45 points, 0 point is regarded as no defect, 0–15 points as light defect, 16–30 points as moderate defect, 31–45 points as severe defect (14).
Independent living standard
Independent living ability scale was adopted for evaluation. High score means high independent living standard ability (15).
Hematoma volume
The volume of hematoma was measured before treatment, 1 week, 2 weeks and 4 weeks after treatment.
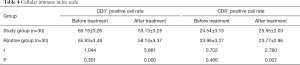
Cellular immunity index
The indexes of cellular immunity were detected, including the rate of CD3+ and CD8+ cells. In the morning, 2 mL of elbow vein blood was taken from the patients with fasting ≥8 h, heparin anticoagulation was added, and the detection was completed within 24 h after collection. Take the flow tube, add 10 µL of monoclonal antibody, then add 100 µL of peripheral blood to mix well, place it away from light at room temperature for 20 min, add 2 mL of hemolysin, and place it at room temperature for 20 min. Centrifugation, discard the supernatant, add 2 mL PBS for washing. Centrifugation, discard the supernatant, and then suspend it in 500 µL PBS again. The cytomics FC500 flow cytometer from Beckman Coulter company was used for detection, and the CXP analysis software was used for analysis (16).
Postoperative complications
The complications of the two groups were analyzed through counting the incidence of complications, such as lung infection, urinary tract infection, liver and kidney dysfunction.
Statistical methods
The research data mainly includes measurement data and enumeration data. SPSS22.0 software was used to analyze the data. Among them,
Results
Analysis of therapeutic effect of two groups of patients
The total effective rate of the study group was 96.67%, which was significantly higher than that of the routine group (80.00%). The difference is statistically significant (P<0.05) (Table 1).
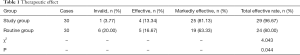
Full table
Analysis of independent living standard and neurological deficit in two groups
The independent living standard of the study group was significantly higher than that of the control group, and the level of neurological deficit was significantly lower than that of the routine group. The difference is statistically significant (P<0.05) (Table 2).
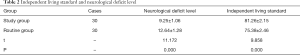
Full table
Evaluation of hematoma volume in two groups
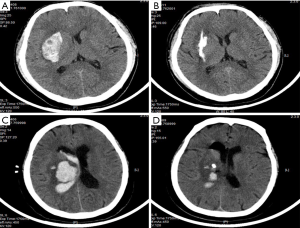
Before treatment, there was no significant difference in hematoma volume between the two groups (P>0.05). After 1, 2 and 4 weeks of treatment, the volume of hematoma in the two groups decreased, and the volume of hematoma in the study group was significantly less than that in the routine group, the difference was statistically significant (P<0.05) (Table 3). Figure 1 represents the brain CT scanning map for patients with hypertensive cerebral hemorrhage preoperative and postoperative.
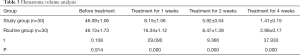
Full table
Cellular immune index in two groups
There was no significant difference in CD3+ positive cell rate and CD8+ positive cell rate between the two groups before treatment (P>0.05). After treatment, the CD8+ positive cell rate of the study group was lower than that of the routine group, and the CD3+ positive cell rate of the study group was higher than that of the routine group, the difference was statistically significant (P<0.05) (Table 4).
Full table
Analysis of postoperative complications in two groups
The incidence of postoperative complications such as pulmonary infection, urinary tract infection, liver and kidney dysfunction in the study group was significantly lower than that in the routine group (P<0.05) (Table 5).

Full table
Discussion
Hypertensive intracerebral hemorrhage is a cardiovascular disease with high incidence. It has the characteristics of sudden onset, high risk, high disability rate and high mortality. Relevant data show that the mortality rate of the disease is more than 35% (4,17-20). At present, there are many controversies on the treatment of hypertensive intracerebral hemorrhage, such as craniotomy hematoma clearance, hand-directed hard channel puncture, small bone window hematoma clearance, stereotactic soft pass puncture, stereotactic evacuation of intracranial hematoma, etc. In general, the treatment is mainly based on the age of patients and the characteristics of bleeding. However, the treatment principles are mainly to reduce intracranial pressure, clear hematoma and improve the prognosis of patients (19,21-23). The purpose of this study is to analyze the effect of stereotactic soft channel puncture and drainage in the treatment of hypertensive cerebral hemorrhage. The results showed that the total effective rate was 96.67% in the study group and 80.00% in the routine group, indicating that stereotactic soft channel puncture and drainage had a significant effect on hypertensive cerebral hemorrhage. In addition, there was no difference in the amount of hematoma between the two groups before treatment. The volume of hematoma in the study group was lower than that in the routine group, indicating that stereotactic soft channel puncture and drainage could effectively clear the hematoma. The independent living standard of the study group was higher than that of the routine group, and the level of neurological deficit was lower than that of the routine group. The results showed that stereotactic soft channel puncture and drainage was beneficial to the recovery of postoperative neurological function and the improvement of independent living ability. There was no difference in CD3+ positive cell rate and CD8+ positive cell rate between the two groups before treatment. After treatment, the positive rate of CD8+ cells in the study group was lower than that in the routine group, and the positive rate of CD3+ cells was higher than that in the routine group, suggesting that stereotactic soft channel puncture and drainage can improve the prognosis of patients with hypertensive cerebral hemorrhage. The incidence of postoperative complications such as pulmonary infection, urinary tract infection, liver and kidney dysfunction in the study group was lower than that in the routine group, indicating that the postoperative complications were less and the safety was high. The operation window of small bone window hematoma removal is clear, which can accurately distinguish hematoma and surrounding tissue, avoid damage to normal tissue, and effectively remove hematoma. However, this operation is not complete in intracranial decompression, so it is difficult to treat unstable hemorrhage. Stereotactic soft channel puncture and drainage was first put forward in 1989. It has become a new surgical method for the treatment of hypertensive cerebral hemorrhage through continuous improvement in clinical practice. This method is to locate the hematoma by CT, puncture the hematoma with professional drainage device, complete suction and drainage, so as to achieve the effect of reducing intracranial pressure and clearing the hematoma (24,25). With this method, the drainage speed can be controlled manually, the location is accurate, the stimulation of brain tissue is small, and the bleeding of various parts of the brain can be removed. The indications are basically the same, so it has won the praise of doctors and patients.
In conclusion, stereotactic soft channel puncture and drainage has many advantages. The treatment of hypertensive intracerebral hemorrhage with this method can promote the recovery of neurological function, improve the independent living standard and effectively improve the prognosis, which is worthy of clinical use.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by ethics board of Funing People’s Hospital (No. 2019009).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Salvetti M, Paini A, Bertacchini F, et al. Therapeutic Approach to Hypertensive Emergencies: Hemorrhagic Stroke. High Blood Press Cardiovasc Prev 2018;25:191-5. [Crossref] [PubMed]
- Yoon EL, Yeon JE, Ko E, et al. An Explorative Analysis for the Role of Serum miR-10b-3p Levels in Predicting Response to Sorafenib in Patients with Advanced Hepatocellular Carcinoma. J Korean Med Sci 2017;32:212-20. [Crossref] [PubMed]
- Fukui N, Golabi P, Otgonsuren M, et al. Hospice care in Medicare patients with primary liver cancer: the impact on resource utilisation and mortality. Aliment Pharmacol Ther 2018;47:680-8. [Crossref] [PubMed]
- Sun Y, Xu B, Zhang Q. Nerve growth factor in combination with Oxiracetam in the treatment of Hypertensive Cerebral Hemorrhage. Pak J Med Sci 2018;34:73-7. [Crossref] [PubMed]
- Sun G, Li X, Chen X, et al. Comparison of keyhole endoscopy and craniotomy for the treatment of patients with hypertensive cerebral hemorrhage. Medicine (Baltimore) 2019;98:e14123. [Crossref] [PubMed]
- Kato N, Chin-Kanasaki M, Tanaka Y, et al. Successful renal replacement therapy for a patient with severe hemophilia after surgical treatment of intracranial hemorrhage and hydrocephalus. Case Rep Nephrol 2011;2011:824709. [Crossref] [PubMed]
- Wang T, Zhao QJ, Gu JW, et al. Neurosurgery medical robot Remebot for the treatment of 17 patients with hypertensive intracerebral hemorrhage. Int J Med Robot 2019;15:e2024. [Crossref] [PubMed]
- Wang GQ, Li SQ, Huang YH, et al. Can minimally invasive puncture and drainage for hypertensive spontaneous Basal Ganglia intracerebral hemorrhage improve patient outcome: a prospective non-randomized comparative study. Mil Med Res 2014;1:10. [Crossref] [PubMed]
- Liang KS, Ding J, Yin CB, et al. Clinical study on minimally invasive liquefaction and drainage of intracerebral hematoma in the treatment of hypertensive putamen hemorrhage. Technol Health Care 2017;25:1061-71. [Crossref] [PubMed]
- Xia L, Han Q, Ni XY, et al. Different Techniques of Minimally Invasive Craniopuncture for the Treatment of Hypertensive Intracerebral Hemorrhage. World Neurosurg 2019;126:e888-94. [Crossref] [PubMed]
- Gai Y, Jia P, He Z, et al. The comparison of key hole and minimally invasive puncture approach in the management of hypertensive cerebral hematoma: A systematic review. Chin J Cerebrovasc Dis 2010;4:21-4. (Electronic Edition).
- Liu J, Xie B, Sun W, et al. Effect of stereotactic soft channel puncture and drainage on hypertensive cerebral hemorrhage. Journal of Nanchang University 2017;57:59-60. (Medical Sciences).
- Jiang F. Clinical analysis of 68 cases of hypertensive intracerebral hemorrhage treated by stereotactic soft channel minimally invasive hematoma puncture and external drainage. Chin J Mod Drug Appl 2014;8:91-3.
- Liu F, Zhang K. Correlations between Serum Levels of IL-6, MMP-9, TIMP-1, hs-CRP, NGF and Neurological Deficits of Patients with Acute Cerebral Infarction. Practical Journal of Cardiac Cerebral Pneumal and Vascular Disease 2017;25:35-8.
- Wang H, Fang S. Effect of continuous nursing on independent living ability and psychosocial adaptation of patients with hypertensive cerebral hemorrhage after discharge. Nursing and Rehabilitation Journal 2014;13:482-4.
- Xi N, Zhou L, Qiao S, et al. Influence of bigeminy nerve nutrition scheme on clinical effects and laboratory indexes of patients with hypertensive cerebral hemorrhage. International Journal of Immunology 2018;41:403-7.
- Zhang X, Zhou S, Zhang Q, et al. Stereotactic aspiration for hypertensive intracerebral haemorrhage in a Chinese population: a retrospective cohort study. Stroke Vasc Neurol 2019;4:14-21. [Crossref] [PubMed]
- Liu X, Zhang P, Guo C, et al. Effect of rehabilitation therapy and nursing intervention on postoperative recovery of patients with hypertensive intracerebral hemorrhage. Exp Ther Med 2019;17:4598-604. [PubMed]
- Gavito-Higuera J, Khatri R, Qureshi IA, et al. Aggressive blood pressure treatment of hypertensive intracerebral hemorrhage may lead to global cerebral hypoperfusion: Case report and imaging perspective. World J Radiol 2017;9:448-53. [Crossref] [PubMed]
- Wang T, Frangou C, Zhang J. Fatty acid oxidation (FAO) metabolic switch: metastasis in lymph nodes driven by yes-associated protein (YAP) activation. Biotarget 2019;3. [Crossref] [PubMed]
- Zhang YB, Zheng SF, Yao PS, et al. Lower Ionized Calcium Predicts Hematoma Expansion and Poor Outcome in Patients with Hypertensive Intracerebral Hemorrhage. World Neurosurg 2018;118:e500-4. [Crossref] [PubMed]
- Wen AY, Wu BT, Xu XB, et al. Clinical study on the early application and ideal dosage of urokinase after surgery for hypertensive intracerebral hemorrhage. Eur Rev Med Pharmacol Sci 2018;22:4663-8. [PubMed]
- Zhang Z, Zhang W. Fragmentation patterns of circulating cell-free DNA demonstrate biomarker potential for human cancers. Biotarget 2019;3. [Crossref] [PubMed]
- Qureshi AI, Palesch YY, Barsan WG, et al. Intensive Blood-Pressure Lowering in Patients with Acute Cerebral Hemorrhage. N Engl J Med 2016;375:1033-43. [Crossref] [PubMed]
- Inamasu J, Nakae S, Adachi K, et al. Angiotensin II receptor blockers following intravenous nicardipine administration to lower blood pressure in patients with hypertensive intracerebral hemorrhage: a prospective randomized study. Blood Press Monit 2017;22:34-9. [Crossref] [PubMed]


