
Association between vitamin D deficiency and fragility fractures in Chinese elderly patients: a cross-sectional study
Introduction
Osteoporosis is a major health problem in the aging population, and it increases the risk of fragility fractures (1). One of the severe consequences of osteoporosis is hip fractures, which in turn increases mortality rates and the risk of premature death (2). With an increasingly aging population, the incidence of hip fractures is similarly increasing dramatically worldwide, resulting in a severe social and economic burden (1,3,4). The incidence rate of osteoporosis-associated hip fractures is predicted to be about 45–70% of total hip fractures in 2050 (5). To reduce the cost of fracture care, it is critical to develop effective therapies designed both to treat and also prevent osteoporosis. Based on the World Health Organization (WHO) guidelines, osteoporosis is diagnosed when a patient’s bone mineral density (BMD) is 2.5 standard deviations below the mean for young healthy women (6). A reduction in BMD is associated with a variety of factors including endocrine dysfunction, side-effects of certain medications, and low diet intake of calcium and vitamin D (7).
Vitamin D [1,25 (OH)2D3] is a seco-steroid that plays a critical role in calcium and phosphate homeostasis. Serum vitamin D levels are positively correlated with BMD values (8). Vitamin D deficiency leads to a reduction in BMD and increases the risk of bone fractures in elderly people (9). Growing evidence has shown that vitamin D insufficiency is highly prevalent in Asian populations (10), however, research focusing on the association between vitamin D deficiency and osteoporotic hip fractures is limited, particularly in Chinese populations. The aim of this study was to measure the prevalence of vitamin D insufficiency and deficiency in elderly patients with hip fractures who had no calcium and vitamin D supplementation. The association between vitamin D levels and osteoporosis was then assessed further.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-19-610).
Methods
Study population
This cross-sectional study was conducted over a period of 12 months (January 2017–December 2018). The study included 60 patients who were admitted to Wenkou Hospital of Qixia and were diagnosed with a hip fracture. Inclusion criteria were as follows: (I) patients aged 65 or over, (II) patients who agreed to participate in the study and signed the informed consent form, (III) patients with fresh fractures treated in Department of Orthopaedics at Wenkou Hospital of Qixia. The exclusion criteria included: (I) a history of joint operations; (II) a history of other joint injuries such as vascular necrosis, inflammatory arthropathy, or infection around knee.
This study was conducted according to the Declaration of Helsinki (as revised in 2013) principles and the ethics was approved by the institutional review board of Wenkou Hospital of Qixia (ethical ID number: QXWK2016082001). Informed consent was obtained from all individual participants included in the study.
BMD T-score analysis
Dual X-ray absorptiometry (DXA) analysis (Hologic QDR, 4,500 W) was used to measure bone density in the lumbar vertebral and femoral bone (femur neck, trochanter and Ward triangle). The BMD T-score analysis was conducted with reference to the WHO’s criteria (6). If the patient’s BMD T score was ≤–2.5 at the lumbar spine, femur neck, and total femur, they were classified as osteoporotic. The patients with BMD T-scores greater than –1.0 in each of these regions were categorized as non-osteoporotic.
Assessment of circulating 25-hydroxyvitamin D (25OHD) concentration
25OHD is the main circulating form of vitamin D. Patients’ venous blood was collected in the non-fasting state and centrifuged at 1,000 rpm for 10 minutes. The supernatant was collected and stored at –80 °C. Serum 25OHD concentrations were measured using an electrochemiluminescence immunoassay (11). The inter- and intra-assay coefficients of variation for serum 25OHD were 8.3% and 6.7% respectively. The serum 25OHD concentrations were further categorized: optimal (≥30 ng/mL), insufficient (21–29 ng/mL), and deficient (<20 ng/mL). These categories were based on the 2011 clinical practice guidelines that were recommended by the Endocrine Society (12).
Other general assessment
Patients with a body mass index (BMI) ≥25 kg/m2 were classified as overweight/obese. Diabetes mellitus was identified if the patient’s plasma glucose level was 200 mg/dL (11.1 mmol/L) or more, or by self-reported use of diabetic medication or physician-diagnosed diabetes.
Statistical analysis
Statistical analyses were performed using SPSS 25. For the purpose of analysis, all laboratory values below the limit of detection for a particular assay were recorded as the lowest value for that assay. Comparison between the patients with both hip fractures and osteoporosis, and the subjects with hip fractures but without osteoporosis were conducted using a student’s t-test or chi-square test. Non-parametric variables were analyzed using the Mann-Whitney U test.
Results
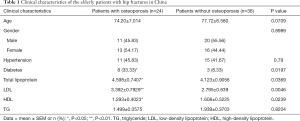
A total of 60 hip fracture patients were included in this study during a 1-year period. Table 1 depicts the demographic and clinical characteristics of the patients. The mean age of these patients was 76.62±6.7. Overall, in all of the patients with hip fractures, the mean serum levels of 25OHD were 28.59 ng/mL and the prevalence of vitamin D deficiency and insufficiency was 10% and 53.33% respectively. Twenty-nine females and 31 males were included in this study. No statistical differences were observed between female and male patients in terms of vitamin D concentrations (P>0.05) (Table 1).
Full table
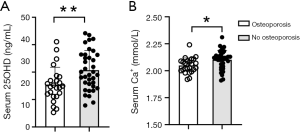
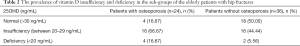
We then divided the patients with hip fractures into two groups according to BMD assessment. Twenty-four patients (40%) with hip fractures were classified as osteoporotic (BMD t value ≤–2.5) and the remainder (36 patients, 60%) were classified as non-osteoporotic. No statistical differences were found between these two groups in terms of age or gender. The patients with both hip fracture and osteoporosis (Figure 1A, are presentative image had significant lower levels of serum 25OHD (25.43±6.35 ng/mL) compared with the patients without osteoporosis (Figure 1B, a representative image) whose serum 25OHD was 30.70±7.17 ng/mL (Figure 2A, P<0.01).The serum Ca2+ was also lower in patients with osteoporosis (Figure 2B, P<0.05). Within the patients with osteoporosis, the prevalence of vitamin D insufficiency and deficiency was 66.7% and 16.7%, respectively. In patients without osteoporosis, the prevalence of vitamin D insufficiency and deficiency was 44.44% and 5.56%, respectively (Table 2).

Full table
Discussion
Our study has shown that low serum vitamin D is common among elderly patients in China who were hospitalized with a hip fracture. Of these patients, the serum levels of 25OHD were significantly lower in those patients with osteoporosis in comparison to those without osteoporosis. This finding is novel, as it reveals a negative association between serum vitamin D levels and osteoporosis in elderly Chinese people, which is consistent with findings in Western populations (13-15).
In our study, the prevalence of vitamin D insufficiency was very high in the elderly patients with hip fractures. In Western patients, this has been shown in approximately 60% of elderly patients with hip fractures (13-15). In other Asian populations, Ramason et al. reported that the prevalence of vitamin D insufficiency in Singapore was 90.5% in Malay patients, 61.1% in Indian patients and 55% in Chinese patients (16). Niikura et al. found that vitamin D insufficiency and deficiency was 71.7% and 21.4%respectively in 360 Japanese patients with fragility fractures of the hip (17). Other studies reported that the prevalence of vitamin D insufficiency was 74% (18) or 39.3% (19) in Japan. Our study showed an overall prevalence of vitamin D insufficiency in 53.3% of 60 elderly Chinese patients with hip fractures. The small discrepancy in the prevalence of vitamin D deficiency across Asian populations could be attributed to the effects of latitude, seasons, religion, poor diet vitamin intake, and possible vitamin D genetic polymorphisms (10). Overall, our finding consistently reported an overall high prevalence of vitamin D insufficiency in elderly Chinese patients with hip fractures.
In addition, our result has also shown that low serum vitamin D levels were associated with a reduced BMD. BMD is a measure of bone calcium content, and a reduction in BMD is a hallmark of osteoporotic fractures. Vitamin D is a key regulator of calcium balance by promoting calcium absorption in the intestine and reducing resorption from the bone (20). A positive correlation between serum vitamin D levels and BMD has been well-documented in the Western population (8). Our study further validated this association in an elderly Chinese cohort.
The mechanisms underlying the negative correlation between serum vitamin D levels and osteoporosis are attributed to the classical function of vitamin D on calcium and phosphate homeostasis. Vitamin D promotes calcium absorption in the intestine and maintains serum calcium and phosphate levels (21). Low vitamin D not only reduces calcium levels, it also induces a compensatory increase of the parathyroid hormone (PTH), which leads to excessive bone absorption (22). Our results have shown that patients with osteoporosis also had low levels of calcium, which could be a consequence of vitamin D deficiency. When serum calcium cannot be maintained at the normal range, vitamin D and PTH could mobilize bone calcium and enhance calcium reabsorption in kidney. Therefore, vitamin D deficiency results in alterations in bone structure and low bone mass.
Apart from vitamin D deficiency, multiple factors contribute to the risk of developing fragility fractures. These include high alcohol consuming, smoking, sex, aging, the use of glucocorticoids, disorders such as rheumatoid arthritis and malnutrition (7). As vitamin D is well known for its role in promoting calcium and phosphates absorption, it has been used as non-pharmacological intervention in the treatment of osteoporosis. In young adult (aged 20–49 years), serum vitamin D levels are also positively correlated with BMD (8) and vitamin D deficiency is also a risk factor of osteoporosis in this population (23).
One limitation of our study is there lative small sample size, which will be addressed by recruiting more patients with hip fractures in future studies. In addition, we only recruited patients with hip fractures who had not taken vitamin D and calcium supplementation, since only a very small number of patients took supplementation prior to admission to the hospital. As our results revealed that the patients with hip fractures and osteoporosis had significant lower levels of vitamin D than those without osteoporosis, inclusion of patients who were taking vitamin D supplementation would provide useful information with regard to the effectiveness of vitamin D supplementation in preventing osteoporosis.
Conclusions
Our data reported a high prevalence of vitamin D insufficiency in an elderly Chinese population, and an association between vitamin D insufficiency and osteoporosis. A recent meta-analysis summarizing 19 studies has revealed that vitamin D supplementation results in a small but significant increase in the density of femoral neck (24). Since the frequency of falls and fractures significantly increases as people age, cost-effective preventive interventions are required. Vitamin D supplements are cheap and safe, and could be a candidate for public health interventions and inclusion in clinical practice.
Acknowledgments
We thank all participants for their participation in our study. The authors thank Dr. Alice Petty from the University of Queensland for her diligent proofreading of the manuscript.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-19-610
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-19-610
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-19-610). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the institutional review board of Wenkou Hospital of Qixia (ethical ID number: QXWK2016082001) and was conducted in compliance with the Declaration of Helsinki (as revised in 2013). Written informed consent forms were obtained from all subjects.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rodan GA. Good hope for making osteoporosis a disease of the past. Osteoporos Int 1994;4 Suppl 1:5-6. [Crossref] [PubMed]
- Panula J, Pihlajamäki H, Mattila VM, et al. Mortality and cause of death in hip fracture patients aged 65 or older: a population-based study. BMC Musculoskelet Disord 2011;12:105. [Crossref] [PubMed]
- Lönnroos E, Kautiainen H, Karppi P, et al. Increased incidence of hip fractures. A population based-study in Finland. Bone 2006;39:623-7. [Crossref] [PubMed]
- Mann E, Icks A, Haastert B, et al. Hip fracture incidence in the elderly in Austria: an epidemiological study covering the years 1994 to 2006. BMC Geriatr 2008;8:35. [Crossref] [PubMed]
- Moratalla R, Robertson HA, Graybiel AM. Dynamic regulation of Ngfi-a (Zif268, Egr1) gene-expression in the striatum. J Neurosci 1992;12:2609-22. [Crossref] [PubMed]
- Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Ser 1994;843:1-129. [PubMed]
- Nuti R, Brandi ML, Checchia G, et al. Guidelines for the management of osteoporosis and fragility fractures. Intern Emerg Med 2019;14:85-102. [Crossref] [PubMed]
- Bischoff-Ferrari HA, Dietrich T, Orav EJ, et al. Positive association between 25-hydroxy vitamin D levels and bone mineral density: a population-based study of younger and older adults. Am J Med 2004;116:634-9. [Crossref] [PubMed]
- Cauley JA, Lacroix AZ, Wu L, et al. Serum 25-hydroxyvitamin D concentrations and risk for hip fractures. Ann Intern Med 2008;149:242-50. [Crossref] [PubMed]
- Lowe NM, Bhojani I. Special considerations for vitamin D in the south Asian population in the UK. Ther Adv Musculoskelet Dis 2017;9:137-44. [Crossref] [PubMed]
- Jafri L, Khan AH, Siddiqui AA, et al. Comparison of high performance liquid chromatography, radio immunoassay and electrochemiluminescence immunoassay for quantification of serum 25 hydroxy vitamin D. Clin Biochem 2011;44:864-68. [Crossref] [PubMed]
- Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2011;96:1911-30. [Crossref] [PubMed]
- Bischoff-Ferrari HA, Can U, Staehelin HB, et al. Severe vitamin D deficiency in Swiss hip fracture patients. Bone 2008;42:597-602. [Crossref] [PubMed]
- Gallacher SJ, McQuillian C, Harkness M, et al. Prevalence of vitamin D inadequacy in Scottish adults with non-vertebral fragility fractures. Curr Med Res Opin 2005;21:1355-61. [Crossref] [PubMed]
- Moniz C, Dew T, Dixon T. Prevalence of vitamin D inadequacy in osteoporotic hip fracture patients in London. Curr Med Res Opin 2005;21:1891-4. [Crossref] [PubMed]
- Ramason R, Selvaganapathi N, Ismail NH, et al. Prevalence of vitamin d deficiency in patients with hip fracture seen in an orthogeriatric service in sunny singapore. Geriatr Orthop Surg Rehabil 2014;5:82-6. [Crossref] [PubMed]
- Niikura T, Oe K, Sakai Y, et al. Insufficiency and deficiency of vitamin D in elderly patients with fragility fractures of the hip in the Japanese population. J Orthop Surg (Hong Kong) 2019;27:2309499019877517. [Crossref] [PubMed]
- Matsumoto T, Miki T, Hagino H, et al. A new active vitamin D, ED-71, increases bone mass in osteoporotic patients under vitamin D supplementation: a randomized, double-blind, placebo-controlled clinical trial. J Clin Endocrinol Metab 2005;90:5031-6. [Crossref] [PubMed]
- Matsumoto T, Ito M, Hayashi Y, et al. A new active vitamin D3 analog, eldecalcitol, prevents the risk of osteoporotic fractures--a randomized, active comparator, double-blind study. Bone 2011;49:605-12. [Crossref] [PubMed]
- Gallagher JC, Jerpbak CM, Jee WS, et al. 1,25-Dihydroxyvitamin D3: short- and long-term effects on bone and calcium metabolism in patients with postmenopausal osteoporosis. Proc Natl Acad Sci U S A 1982;79:3325-9. [Crossref] [PubMed]
- Li YC, Pirro AE, Amling M, et al. Targeted ablation of the vitamin D receptor: an animal model of vitamin D-dependent rickets type II with alopecia. Proc Natl Acad Sci U S A 1997;94:9831-5. [Crossref] [PubMed]
- Yoshizawa T, Handa Y, Uematsu Y, et al. Mice lacking the vitamin D receptor exhibit impaired bone formation, uterine hypoplasia and growth retardation after weaning. Nat Genet 1997;16:391-6. [Crossref] [PubMed]
- Ferrari S, Bianchi ML, Eisman JA, et al. Osteoporosis in young adults: pathophysiology, diagnosis, and management. Osteoporos Int 2012;23:2735-48. [Crossref] [PubMed]
- Reid IR, Bolland MJ, Grey A. Effects of vitamin D supplements on bone mineral density: a systematic review and meta-analysis. Lancet 2014;383:146-55. [Crossref] [PubMed]


