
Treatment of hyperlipidemia with proprotein convertase subtilisin/kexin type 9 inhibitor in a patient with nephrotic syndrome: a case report
Introduction
Nephrotic syndrome is a clinical syndrome characterized by peripheral edema, massive proteinuria, hypoalbuminemia, and hyperlipidemia. Elevated plasma levels of cholesterol, low-density lipoprotein (LDL), triglycerides, and lipoprotein(a) are commonly observed in patients with nephrotic syndrome. Although statin is the first line drug for treating hyperlipidemia in patients with nephrotic syndrome, patients may present with statin intolerance or severe side effects. Here, we report a case of hyperlipidemia treated using a proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitor in a patient of nephrotic syndrome with statin intolerance. This is a unique case of treating hyperlipidemia with PCSK9 inhibitor in patient with nephrotic syndrome with toxic epidermal necrolysis (TEN). We present the following case in accordance with the CARE Reporting Checklist (available at http://dx.doi.org/10.21037/apm-19-587).
Case presentation
A 54-year-old woman presented to the Department of Nephrology owing to generalized edema. She denied history of any underlying disease or medication. Dipstick urine analysis showed 4+ proteinuria without hematuria. Laboratory examination revealed: blood urea nitrogen, 14.7 mg/dL; serum creatinine, 0.80 mg/dL, total protein 4.7 g/dL, serum albumin 2.6 g/dL, total cholesterol 371 mg/dL, LDL-cholesterol 202 mg/dL. Her 24-hour urine protein was 5.89 g/day. Therefore, we diagnosed her with nephrotic syndrome and performed renal biopsy. Pathologically, she was diagnosed with minimal change disease, and we prescribed high dose steroids (deflazacort 72 mg/day). Two weeks after the onset of treatment, she complained of a skin rash on her neck, trunk, and lower extremities, which presented as mildly pruritic erythematous diffuse patches with desquamation. The lesions spread over time as they grew in size and turned into bullae, affecting more than 60% of the body surface. She was admitted under suspicion of TEN. All drugs except steroids and diuretics were discontinued, and antibiotics were administered owing to the risk of secondary infections caused by the skin lesions. Rosuvastatin was suspected as a causative agent of TEN.
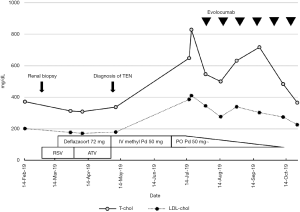
Skin lesions gradually improved after discontinuation of the suspected causative agent; however, proteinuria did not decrease despite continued treatment with steroids. Hyperlipidemia also persisted, with total cholesterol levels of 829 mg/dL and LDL cholesterol levels of 410 mg/dL. Nevertheless, we could not reuse statins because of the possibility of cross-reactivity of statin hypersensitivity. Thus, we decided to adopt an alternative treatment plan for control of hyperlipidemia owing to the severity of the symptoms. We administered 140 mg of evolocumab, a PCSK9 inhibitor, to the patient every 2 weeks. Her total cholesterol and LDL cholesterol levels were controlled without the use of statins (Figure 1).
Discussion
This report presents the case of a 54-year-old woman with nephrotic syndrome who showed signs of statin intolerance and was successfully treated for hyperlipidemia using PCSK9 inhibitors. Hyperlipidemia and lipiduria are commonly seen in patients with nephrotic syndrome. The most common lipid abnormalities in patients with nephrotic syndrome are hypercholesterolemia and hypertriglyceridemia. The two known pathophysiologic mechanisms of hyperlipidemia in nephrotic syndrome are decreased clearance and decreased plasma oncotic pressure, which stimulates hepatic lipoprotein synthesis resulting in hypercholesterolemia. Impaired metabolism is also responsible for nephrotic hypertriglyceridemia. The lipid abnormalities induced by the nephrotic syndrome improve with resolution of the disease. Most patients are initially treated using a 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitor (statin). The most well-known adverse effects of statins are myalgia, rhabdomyolysis, and liver dysfunction. Significant skin reactions are uncommon. To our knowledge, only one case of TEN induced by statin has been reported previously (1). In that case, administration of the statin that caused TEN was not attempted, and the diagnosis was based on the temporal relationship alone. In our case, the drug challenge test could not be performed owing to the fatal symptoms of the patient. However, a temporal relationship was observed between rosuvastatin use and TEN development, suggesting a causative agent.
PCSK9 is a protease involved in LDL receptor degradation, mainly produced by the liver and released into the systemic circulation. The blood levels of PCSK9 are elevated in nephrotic patients and have been observed to decrease with resolution of nephrotic syndrome (2,3). The total cholesterol and LDL cholesterol levels correlated with plasma PCSK9 level (2). Therefore, we presumed that hypercholesterolemia could be treated by using PCSK9 inhibitor in patients with nephrotic syndrome. Recently, two studies have been published in which patients with nephrotic syndrome were administered PCSK9. Kohli et al. used PCSK9 inhibitor in 52-year-old woman with statin intolerance and nephrotic syndrome (4). Although there was a response after using pioglitazone in this patient, PCSK9 inhibitor effectively reduced LDL cholesterol levels. Awanami et al. used evolocumab in a 61-year-old woman with refractory nephrotic syndrome (5). They reported that PCSK9 inhibitors not only reduced LDL cholesterol levels but also regulated the nephrotic condition itself. In our patients, it was difficult to control hyperlipidemia owing to severe adverse cutaneous reactions caused by statins. We could effectively control hyperlipidemia in the patient without additional side effects by administering PCSK9 inhibitors. Nevertheless, this case has some limitations. First, as mentioned above, the challenge test was not performed to identify the causative agent of TEN. The second limitation is that it is difficult to completely rule out the possibility that the hyperlipidemia has improved due to the effects of steroids used to treat TEN.
In conclusion, we present a case of nephrotic syndrome patients with TEN caused by statin use that effectively controlled hyperlipidemia with PCSK9 inhibitors. Thus, PCSK9 inhibitors may be a good alternative to control hyperlipidemia in patients with statin intolerance or serious side effects of statin.
Acknowledgments
Funding: This study was supported by the Bio & Medical Development Program of the National Research Foundation (NRF) funded by the Korean government (MSIT) (2017M3A9E8023001 and 2017M3A9E8023016).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-19-587). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pfeiffer CM, Kazenoff S, Rothberg HD. Toxic epidermal necrolysis from atorvastatin. JAMA 1998;279:1613-4. [Crossref] [PubMed]
- Jin K, Park BS, Kim YW, et al. Plasma PCSK9 in nephrotic syndrome and in peritoneal dialysis: a cross-sectional study. Am J Kidney Dis 2014;63:584-9. [Crossref] [PubMed]
- Haas ME, Levenson AE, Sun X, et al. The Role of Proprotein Convertase Subtilisin/Kexin Type 9 in Nephrotic Syndrome-Associated Hypercholesterolemia. Circulation 2016;134:61-72. [Crossref] [PubMed]
- Kohli M, Patel K, MacMahon Z, et al. Pro-protein subtilisin kexin-9 (PCSK9) inhibition in practice: lipid clinic experience in 2 contrasting UK centres. Int J Clin Pract 2017. [Crossref] [PubMed]
- Awanami Y, Fukuda M, Nonaka Y, et al. Successful treatment of a patient with refractory nephrotic syndrome with PCSK9 inhibitors: a case report. BMC Nephrol 2017;18:221. [Crossref] [PubMed]


