
Use of thromboelastography to monitor effects of the hemocoagulase on the blood coagulation in patients after thoracic surgery
Introduction
Because chest disease covers a wide range, involving the heart, lung, mediastinum and other important organs, large lesions, invasion of large vessels, mediastinum and other parts, and thoracic surgery is easy to cause intraoperative bleeding, usually leads to bleeding (1). Reasonable use of hemostatic drugs can effectively reduce intraoperative and postoperative bleeding. Since the 1970s, snake venom thrombin-like (SVTLEs) preparations, owing its low toxicity, fast onset, and long-lasting efficacy, many basic researchers and clinicians have carried out extensive research on it. At present, SVTLEs is mainly used in hemostasis, antithrombotic, diagnostic reagents and so on. Studies have shown that the efficiency of hemocoagulase for hemostasis in surgical incisions is notably better than that of hemostatic drugs like etamsylate, carbazochrome sodium sulfate, vitamin K, etc. (2). Hemocoagulase that is isolated and purified from snake venom is a protease with thrombin-like activity. Its main mechanism is hydrolyzing fibrinogen (FIB) to form fibrin and further promote coagulation. The three most routinely used venom thrombin-like preparations in our hospital are Baquting (Bothrops atrox) (Penglai Nuokang Pharmaceutical Co., Ltd., No. 118 Jinchuang Road, Penglai City, Shandong Province), Bangting (Amphiesma boulengeri) (Ahon Pharmaceutical Co., Ltd., No. 55 Songshan Street, Taihe District, Jinzhou City, Liaoning Province) and Su Ling (Agkistrodon acutus) (Beijing Konruns Pharmaceutical Co., Ltd., No. 7, Zhongguancun Life Science Park Road, Changping District, Beijing). In recent years, cases of hypofibrinogenemia and bleeding after using the hemocoagulase have been reported (3,4) and cannot be ignored. This article analyzed the coagulation status of patients who underwent thoracic surgery and used hemocoagulase hemostatic drugs in our hospital. In the other similar report study, the Coagulation state is the amount of bleeding, which can only study the bleeding state. This study uses TEG detection, TEG can more truly reflect the coagulation state of patients, because it simulates the whole blood coagulation state. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-1221).
Methods
General materials
Inclusion criteria
Patients treated with venom thrombin-like preparations following thoracic surgery in the First Affiliated Hospital of Soochow University between June 2018 and June 2019 were recruited; preoperative blood routine and blood coagulation routine and thromboelastography (TEG) 48 h after thoracic surgery were evaluated. None of the patients received antiplatelet or anticoagulant therapy before blood collection. All patients were started on intramuscular injection of hemocoagulase immediately after the operation, with an injection of two units at a time, twice a day. Patients were excluded according to the following criteria: (I) preoperative application of anticoagulant therapy; (II) anemia; (III) liver and kidney dysfunction; no preoperative history of clotting disorders.
In the present study, patients with coagulation index (CI) <−3 on TEG results 48 h after surgery were set as the low CI group, and those with normal coagulation status were selected as the Control Group and matched to the low CI group in terms of gender, age, and disease type.
Drugs
Hemocoagulase for injection included Baquting (Bothrops atrox) (Penglai Nuokang Pharmaceutical Co., Ltd.), Bangting (Amphiesma boulengeri) (Ahon Pharmaceutical Co., Ltd.), and Su Ling (Agkistrodon acutus) (Beijing Konruns Pharmaceutical Co., Ltd.).
Methodology
The data collection indicators including gender, age, diagnosis, types of hemocoagulase used, blood routine, blood coagulation routine, TEG, etc. were obtained from the hospital medical record system. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was reviewed and approved by the ethics committee of the hospital with approval number: [2020] ethical research No. 088. This was a retrospective study, so informed consent is not required. Among the patients in the low CI group, 2 were given injection of Baquting, 22 were given injection of Bangting, and 19 were given injection of Suling. Meanwhile, in the control group, 10 were given injection of Baquting, 20 were given injection of Bangting, and 24 were given injection of Suling.
Statistical method
The SPSS17.0 software system was used for data processing, and measurement data was expressed as mean ± standard deviation (mean ± s). A t-test was used for comparisons between the two sets of measurement data, and a rank-sum test was used for data if one set of the measurement data did not conform to the normal distribution and homogeneity of variance. A P value of <0.05 indicated that the difference was statistically significant.
Results
Basic materials
A total of 1,025 patients from the Department of Thoracic Surgery at The First Affiliated Hospital of Soochow University admitted from June 2018 to June 2019 were enrolled. According to the results of postoperative TEG, 43 patients with low CI 71 were set as the low CI group (CI was one of indicator of TEG). From a total of the 43 patients, 22 were males and 21 were females, with an average age of 59.3±11.18 years. In terms of malignancies, 20 patients had pulmonary malignant tumor, 1 patient had pulmonary carcinoma in situ, 3 patients had esophageal malignant tumor, 1 patient had thymoma, 3 patients had mediastinal malignant tumor, 14 patients had benign lung lesions, and 1 patient had pericardial cyst. A control group of 54 patients randomly selected from the patients with normal coagulation status were age-, gender- and disease- matched to the low CI group. Among the 54 patients, 30 were males and 24 were females, with an average age of 59.03±11.3 years. In terms of malignancies 22 patients had pulmonary malignant tumor, 5 patients had pulmonary carcinoma in situ, 4 patients had esophageal malignant tumor, 2 patients had thymoma, 3 patients had mediastinal malignant tumor, and 18 patients had benign lung lesions.
The primary parameters of TEG for statistical comparisons between the low CI group and the control group were reaction time (R), clotting time (K), maximum angle of elasticity (α-angle), and maximal amplitude (MA) (Table 1).
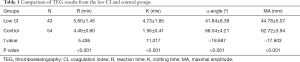
Full table
Indices of preoperative platelet and blood coagulation routine for comparison between the two groups (Table 2) included prothrombin time (PT), international standardized ratio (PT-INR), activated partial thromboplastin time (APTT), thrombin time (TT), FIB, antithrombin III (AT-III), and platelet (PLT). The levels of FIB in the low CI group were significantly lower compared with those in the Control group (P<0.01). No significant differences were found among other indices.
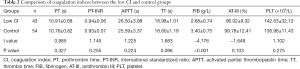
Full table
Treatment and outcome of the patients with low CI
Of the 43 patients with low CI, two had bleeding. An elderly esophageal cancer patient started on Bongting 2KU Bid immediately following the operation. The TEG showed a CI of −4.3 48 h after the operation. A total of 680 mL of drainage fluid was found in the gastric tube, thoracic drainage tube, mediastinal drainage tube, abdominal drainage, tube and neck wound drainage tube within 24 h after the operation, which was a significant increase. Prior to this point, Bangting was being administered to 8 U and was immediately discontinued under medical advice. Following administration of 400 mL of fresh frozen plasma, the drainage fluid was reduced to 450 mL in the 24th hour on the third day. Re-examination of TEG parameters showed an R value of 5.5, a K value of 1.5, an α-angle value of 69.1, an MA value of 65, and a CI value of 1.5, indicating normal coagulation status. The patient was discharged after a normal extubation 12 days after the operation. Another young male patient with a benign lung lesion was administered Bangting 2KU Bid immediately after the operation. Around 48 h after the operation, the TEG showed a CI of −4.4. In the early morning of the second postoperative day, the patient's drainage fluid suddenly increased to 1,000 mL. Due to rapid bleeding, 4 U of suspended leukoerythrocytes and 600 mL of fresh frozen plasma were immediately infused. Following an emergency thoracotomy, around 500 mL of a moderate amount of blood clot was detected in the front edge of the original incision. Emergency examination of blood coagulation routine showed FIB 1.95 g/L, which was significantly lower than that before surgery. Bangting 6 U had been used and was immediately suspended under medical advice. During the emergency operation, 1 g of FIB, 400 mL of fresh frozen plasma, and 4 U of cryoprecipitate were infused intraoperatively; and 3 U of suspended leukocytes, 400 mL of fresh frozen plasma, and 4 U of cryoprecipitate were given after the emergency operation. After, the drainage volume returned to 970 mL 21 h after the emergency operation. Following transfusion of 1g FIB, 400 mL of fresh frozen plasma, and 4 U of cryoprecipitate, the drainage volume decreased significantly on the second day after the emergency operation. The reexamination of TEG showed normal coagulation status with an R of value 5.2, a K of value 1.2, an α-angle of 70.8, an MA value of 67.3 and a CI value of 1.9. On the third day after the emergency operation, the drainage volume was observed each day, and the discharge volume was maintained at around 250 mL. The patient was discharged 1 week later. The other 41 patients did not show increased drainage or other tendency to bleeding.
Discussion
The perioperative period of cardiothoracic surgery is accompanied by coagulation disorders due to the malignant tumor itself, surgical injury, intraoperative blood transfusion, infusion, and the use of hypothermic and anticoagulant drugs. Bleeding is one of the common complications (5). In clinic, in order to prevent patients from postoperative bleeding, hemostatic treatment is performed by administering related coagulation drugs. Hemocoagulase has a good hemostatic function, and the adverse drug reactions are minor and well tolerated (6). It is currently a widely utilized clinical coagulation drug. At the moment, the commonly used snake venom thrombin-like preparations use snake venom thrombin as the main component. Although different snake venom-derived thrombin preparations have a slightly different effect on FIB, they all promote the conversion of fibrinogen into fibrin monomers, which then cross-link and polymerize into insoluble fibrin and eventually promote coagulation. Clinically, this kind of medicine is usually applied promptly after the surgery to prevent bleeding.
During surgical process, the patient’s coagulation function is affected by many factors. In the present study, dilute coagulation dysfunction was caused by its own coagulation dysfunction, liver and kidney dysfunction, and a preoperative injection of a large amount of stored blood was excluded. TEG, performed 48 h after the operation, found that 43 of the 1,025 patients exhibited a low coagulation status after the operation. In the 43 patients, the CI index in TEG, which indicates the comprehensive CI, was lower than −3, suggesting a low blood coagulation status, and 2 patients emerged with bleeding symptoms. Under medical advice of cessation of the hemocoagulase and a subsequent infusion of 400 mL fresh frozen plasma, one patient’s drainage volume was largely reduced. The other patient, due to a large amount of bleeding, was infused with a large amount of red blood cells, FIB, fresh frozen plasma, and cryoprecipitate; reexamination of TEG indicated normal status. Then, the infusion was suspended, and the amount of drainage fluid significantly decreased.
In the TEG, the R value primarily reflects the role of clotting factors in the formation of fibrin clots, and the K value and α-angle reflect the interaction between platelets and fibrin when clots begin to form (i.e., the rate of blood clot formation). The length of K is mainly affected by the level of FIB, and the factors affecting the α-angle are the same as the K value. MA is mainly affected by two factors of platelets and FIB, in which platelets account for about 80% and FIB accounts for about 20%. Abnormalities in platelet quantity or quality affect the MA value (7). In the present study, although the coagulation reaction time (R value) of the Low CI group was significantly longer than that of the Control group, its R value was within the normal reference range, while the value of the control group was slightly lower than the reference value, which may be related to coagulation factor activation under tumor and surgical stress situations (8). The K value of the low CI group was obviously prolonged, and the α-angle was largely smaller than that of the Control group, suggesting that the FIB level of the low CI group was overtly reduced. At the same time, the MA value in the low CI group was significantly smaller than that in the Control group. There was no difference in platelet count and platelet dysfunction between the two groups. The results indicate that the low level of CI was affected by the FIB. In summary, the hypocoagulable state found in 43 patients was caused by low FIB. Analysis of the preoperative blood coagulation routine results showed that the FIB content in the low CI group was significantly lower than that in the control group (2.68±0.74 vs. 3.40±0.75). No statistical difference was found between the other indexes. After analysis, it was found that although the content of FIB in the low CI group was mostly within the reference range, part of it was close to the lower limit of the reference value. Despite studies reporting that hemocoagulase leads to reduced FIB, there are a considerable number of cases that are a result of improper dosage and length (9). This study, by using the hemocoagulase in the same amount and time, analyzed and concluded that postoperative hypofibrinogenemia may be related to the patient’s own FIB content. Therefore, prior to clinical administration of this kind of hemocoagulase, close attention should be paid to the amount of FIB in patients. Meanwhile, there are also views that hypofibrinogenemia may affect the occurrence of endothelial cells, which will lead to a decrease in FIB. Hence, variations in FIB should also be observed in the time after applying such drugs.
Compared with the traditional coagulation test, TEG can dynamically observe the changes of the coagulation process, mainly including the time from the activation of coagulation facto r to the start of fibrin formation, the strengthening of fibrin, the platelet binding to the blood clot, the formation time of the blood clot, fibrinolysis process, etc. These results, which are rapidly and accurately obtained, can comprehensively reflect the coagulation status of the patient (10). In contrast, the traditional coagulation test fails to reveal a comprehensive picture of coagulation (11); it is thus incapable of accurately judging the cause of abnormal bleeding and therefore cannot provide an accurate and timely guide for clinical blood transfusion. On the contrary, TEG, by reflecting the whole process of blood clot formation, progress, stability and final degradation can provide specific reasons for abnormal blood clotting. Besides this, ample research has shown that TEG can more effectively guide perioperative blood transfusion (12,13).
This study is a retrospective analysis and, as such, has its certain limitations. In future studies, TEG testing should be performed at the same time as the preoperative examination of blood coagulation routine to perform dynamic coagulation status comparison. In current clinical work, after being treated with snake venom drugs, most patients are not monitored for coagulation status. Therefore, it is recommended that TEG and FIB tests be performed in clinic after using such drugs to avoid bleeding and other conditions. In brief, the use of hemocoagulase can cause FIB reduction and result in serious bleeding. It is important to be informed of its indications and to monitor the FIB content. For those patients with low preoperative FIB content, these drugs should be administered with caution. After surgery, TEG should be performed in time to monitor coagulation status and to ensure the safety of the patient.
In short, as hemocoagulase has been widely used in various surgical procedures, TEG is a more effective method for monitoring the coagulation status and for guiding blood transfusion in these patients.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-1221
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-1221
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-1221). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was reviewed and approved by the ethics committee of the hospital with approval number: [2020] ethical research No. 088. This was a retrospective study, so informed consent is not required.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Schirren M, Sponholz S, Oguhzan S, et al. Intraoperative bleeding during thoracic surgery: avoidance strategies and surgical treatment concepts. Chirurg 2015;86:453-8. [Crossref] [PubMed]
- Gupta G. M R M, Kumar SP. Efficacy of Hemocoagulase as a Topical Hemostatic Agent After Dental Extractions: A Systematic Review. Cureus 2018;10:e2398. [PubMed]
- Lu S, Han M, Song Y, et al. Hemocoagulase agkistrodon can prevent bleeding and induce hypofibrinogenemia in hepatic disease cases. Int J Clin Pharmacol Ther 2020;58:351-3. [Crossref] [PubMed]
- Zhang H. The Effects of Hemocoagulase on Coagulation Factors in an Elderly Patient with Upper Gastrointestinal Hemorrhage: A Case Report. Curr Drug Saf 2019;14:230-2. [Crossref] [PubMed]
- Igai H, Kamiyoshihara M, Yoshikawa R, et al. Algorithm-based troubleshooting to manage bleeding during thoracoscopic anatomic pulmonary resection. J Thorac Dis 2019;11:4544-50. [Crossref] [PubMed]
- Lan X, Ma L, Lu M, et al. Safety of hemocoagulase agkistrodon on the hemostasis in patients undergoing orthopaedic surgery. Chin J Clin Pharmocol 2016;32:273-5.
- Honickel M, Grottke O, Honickel M, et al. Rotational thromboelastometry for the diagnosis of coagulation disorders. Med Klin Intensivmed Notfmed 2018;113:542-51. [Crossref] [PubMed]
- Mandoj C, Tomao L, Conti L. Coagulation in Brain Tumors: Biological Basis and Clinical Implications. Front Neurol 2019;10:181. [Crossref] [PubMed]
- Lv T. Analysis of 5 cases of low fibrinogenemia in patients with bronchiectasis hemoptysis. Journal of China Prescription Drug 2018;16:53-4.
- Gonzalez E, Moore EE, Moore HB. Management of Trauma-Induced coagulopathy with thromboelastography. Crit Care Clin 2017;33:119-34. [Crossref] [PubMed]
- Sabate A, Blasi A. Thromboelastography and blood product usage in cirrhosis with severe coagulopathy. Hepatology 2017;65:1413-4. [Crossref] [PubMed]
- Unruh M, Reyes J, Helmer SD, et al. An evaluation of blood product utilization rates with massive transfusion protocol: Before and after thromboelastography (TEG) use in trauma. Am J Surg 2019;218:1175-80. [Crossref] [PubMed]
- Fassl J, Matt P, Eckstein F, et al. Transfusion of allogeneic blood products in proximal aortic surgery with hypothermic circulatory arrest: effect of thromboelastometry-guided transfusion management. J Cardiothorac Vasc Anesth 2013;27:1181-8. [Crossref] [PubMed]


