
Lactate level and unplanned readmission to the surgical intensive care unit: a retrospective cohort study
Introduction
Intensive care unit (ICU) readmission after discharge is among the key markers of quality of care and outcomes in critically ill patients (1,2). In previous studies, the ICU readmission rates ranged from 1.2% to 14.5% (3-6). ICU readmission is known to be associated with increased hospitalization and mortality rates among critically ill patients (3,4,7-10). Therefore, reducing ICU readmission rates has considerable implications with respect to the improvement of hospital outcomes, quality of care, hospital resource utilization, and cost savings in critically ill patients (11).
The serum lactate level, which was first reported by Broder and Weil et al. (12,13), has been widely used as an important marker, that reflects altered tissue perfusion in critically ill patients (14). In particular, the elevation in lactate levels directly reflects tissue hypoperfusion induced by macrocirculatory or microcirculatory dysfunction (15,16), reduced oxygen delivery (17), enhanced glycolysis (18), or metabolic blocks of pyruvate dehydrogenase (19). Thus, elevated lactate levels or lactate kinetics is known to be a predictive factor for poor outcomes in critically ill patients (20). Previous studies have reported that elevated lactate levels were associated with higher mortality among surgical ICU patients (21) and neurologic ICU patients (22). Therefore, elevated lactate levels may serve as an indicator in predicting outcomes including ICU readmission among ICU patients. However, the outcome measure of these studies mostly included mortality and not ICU readmission, and thus, the association between lactate levels in the ICU and ICU readmission rates remains unclear.
Therefore, this study aimed to investigate the association between lactate levels (initial lactate at ICU admission, peak level during ICU stay, and last level before ICU discharge) and unplanned ICU readmission rates within 48 or 120 h in surgical ICU patients. We hypothesized that increased lactate levels during the ICU stay are associated with unplanned ICU readmission rates in surgical and critically ill patients.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-291).
Methods
Study design and data source
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This retrospective cohort study was conducted in a single tertiary academic hospital and was approved by the Institutional Review Board (IRB) of Seoul National University Bundang Hospital (SNUBH) (IRB approval number: B-1904/534-103). The requirement for informed consent was waived owing to the retrospective design of this study. Data were collected from the electronic medical records of Bundang Hospital Electronic System for Total Care (BESTCare) at SNUBH (23).
Study population
We evaluated adult patients (≥18 years old) who were admitted to the ICU in the surgical department and were discharged from there between January 2012 and December 2018. For multiple ICU admissions (≥2) in one patient, only the first ICU admission during the study period was included in the analysis, given that the main endpoint of this study was unplanned ICU readmission. Patients who were transferred to another hospital directly after ICU discharge and those with incomplete or missing medical records pertaining to serum lactate levels were excluded.
Measurement of lactate level
The lactate level was commonly measured using radial or femoral arterial blood in the ICU. The initial lactate level (mg dL-1) was defined as the first serum lactate level measured within 6 hours after ICU admission, regardless of whether the patient was admitted to the ICU from the emergency room, general ward, or postoperatively. The last lactate level was defined as the last measurement before ICU discharge. The maximum value of the lactate level during ICU stay was defined as the peak lactate level.
Assessment of unplanned ICU readmission
Unplanned ICU readmission was defined as an unexpected second admission to the ICU, from which the patient was originally discharged during the same hospitalization. We evaluated ICU readmission within 48 and 120 h based on previous studies (5,24). We selected 48 h, as proximate readmissions may be most likely to be attributable to ICU care or triage decisions (25). In contrast, readmissions after 120 hours are more likely to be elective or caused by events occurring on the floor after discharge.
Potential covariates
Clinicodemographic data, including sex, age (years), body mass index (BMI, kg m-2), socioeconomic status [e.g., type of insurance (medical aid beneficiary program or national health insurance program)], Charlson comorbidity index at ICU admission, Acute Physiology and Chronic Health Evaluation (APACHE) II score at ICU admission, characteristics of ICU stay (year of discharge, duration, ventilator care, postoperative ICU care, and admission to the cardiothoracic department), were collected. Medical aid beneficiaries include those having low incomes; the bulk of the hospital charges for these patients are paid by the government. For patients in the national health insurance program, the government covers approximately two-thirds of their hospital charges. The International Classification of Disease-10 (ICD-10) codes in the electronic health record system were used to calculate the Charlson comorbidity index of all patients.
Statistical analysis
Baseline characteristics have been presented as the mean value with the standard deviation (SD) for continuous variables or numbers with percentages for categorical variables. Univariable logistic regression analysis was initially conducted to investigate the individual association of all covariates with ICU readmission. Covariates with a P value of <0.2 in the univariable model were then entered into the final multivariable logistic regression model. All the results of the logistic regression model were provided as odds ratio (OR) with 95% confidence interval (CI), and the goodness of fit in each multivariable model was confirmed via the Hosmer-Lemeshow statistic test with a criterion of P>0.05. We analyzed multi-collinearity in each multivariable model with a variance inflation factor <2.0. Finally, we performed receiver operating characteristic (ROC) analysis for unplanned readmission within 48 h based on three main variables (i.e., initial lactate, last lactate, and peak lactate level during ICU stay) with two traditional scoring systems, namely, APACHE II and Charlson comorbidity index. The results of the ROC analysis were presented as the areas under the curve (AUC) with 95% CI. All analyses were performed using the R software package, version 3.6.0 (R Foundation for Statistical Computing, Vienna, Austria), and P<0.05 was considered statistically significant.
Results
Patient characteristics
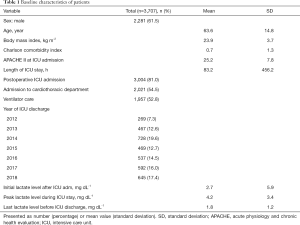
Among the 11,552 adult patients (age ≥18 years) discharged alive from the surgical ICU between January 2012 and December 2018, 7,845 were excluded due to multiple admissions (n=712), transfer to another hospital after ICU discharge (n=114), and incomplete or missing medical records of serum lactate levels at ICU admission and discharge (n=7,019). Finally, 3,707 patients were included in the analysis. The baseline patient characteristics are presented in Table 1. The mean (SD) initial, peak, and last lactate level (mg dL-1) after ICU admission were 2.7 (5.9), 4.2 (3.4), and 1.8 (1.2), respectively. The unplanned ICU readmission rates within 48 and 120 h were 2.1% (n=78 patients) and 4.5% (n=166 patients), respectively (Figure 1). The departments with the highest readmission rates were the neurosurgery department (53.6%), followed by cardiopulmonary (23.8%), general surgery (9.8%), and orthopedic surgery departments (5.6%).
Full table
Unplanned ICU readmissions and lactate level
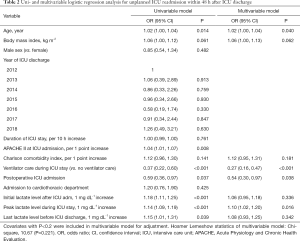
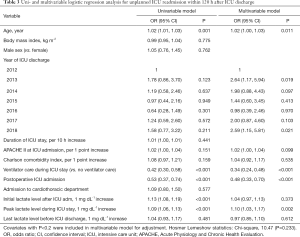
The mean peak lactate level was 6.66 and 4.13 mg dL-1 in those who were and were not readmitted within 48 h, respectively, and was 5.55 and 4.11 mg dL-1 in those who were and were not readmitted within 120 h, respectively. The results of uni- and multivariable logistic regression analyses for unplanned ICU readmission within 48 h after ICU discharge are presented in Table 2. In the multivariable logistic regression model for unplanned ICU readmission within 48 h, a 1 mg dL-1 increase in peak lactate level during ICU stay was associated with a 1.1-fold increase in unplanned ICU readmission within 48 h (OR: 1.10; 95% CI: 1.02 to 1.2; P=0.016), but the initial and last lactate levels during ICU stay were not (P=0.336 and P=0.342, respectively). The results of uni- and multivariable logistic regression analyses for unplanned ICU readmission within 120 h after ICU discharge are presented in Table 3. In the multivariable logistic regression model for unplanned ICU readmission within 120 h, a 1 mg dL-1 increase in peak lactate level during ICU stay was associated with a 1.1-fold increase of unplanned ICU readmission within 120 h (OR: 1.10; 95% CI: 1.03 to 1.17; P=0.002). However, both initial and last lactate levels during ICU stay were not significantly associated with unplanned ICU readmission within 120 h (P=0.373 and P=0.612, respectively).
Full table
Full table
Receiver operating characteristic analysis
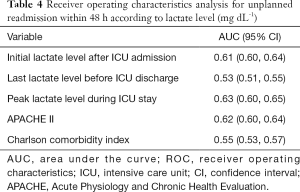
On ROC analysis for unplanned ICU readmissions within 48 h, the AUCs of the initial, last, and peak lactate levels during ICU stay were 0.61 (95% CI: 0.60 to 0.64), 0.53 (95% CI: 0.51 to 0.55), and 0.63 (95% CI: 0.60 to 0.65), respectively (Table 4). Additionally, the AUCs of the APACHE II score and Charlson comorbidity index were 0.62 (95% CI: 0.60 to 0.64) and 0.55 (95% CI: 0.53 to 0.57), respectively.
Full table
Discussion
The present study showed that in surgical ICU patients, the peak level of lactate during ICU stay was significantly associated with unplanned ICU readmission both, within 48 and 120 h, but the initial lactate level after ICU admission or last lactate level before ICU discharge was not. These results indicate that the peak lactate level during ICU admission is the most appropriate predictor of unplanned ICU readmission among surgical patients. However, our results also showed that the lactate level during ICU stay has poor predictive capability (AUC <0.7), and cannot be used alone to predict unplanned ICU readmission.
The most important finding in this study was that among the initial, peak, and last lactate levels during ICU stay, only the peak lactate level was significantly associated with unplanned ICU readmission. This finding may reflect the characteristics of our surgical cohort. First, our cohort included 81.0% (3,004/3,707) of patients who were admitted to the surgical ICU postoperatively. A higher lactate level in the postoperative period during ICU stay could reflect postoperative complications (26,27). Further, the peak lactate level in these patients may have reflected the severity of postoperative complications. In addition, a higher peak lactate level in these patients may have also reflected surgical stress (28), which may be affected by blood loss, surgical extent, or duration of surgery. Similarly, the peak lactate level was associated with postoperative outcomes such as mortality in cardiac surgery (29) or high-risk gastrointestinal surgery (30). Therefore, it is possible that in patients postoperatively admitted to the ICU, a higher peak lactate level during ICU admission could reflect both, postoperative complications and surgical stress, and this could influence unplanned ICU readmission.
However, our results showed that ICU admission in the postoperative period or mechanical ventilator use was associated with a lower rate of unplanned readmission compared with other patients in the surgical department or with no use of mechanical ventilators. This finding may have been influenced by the characteristics of the study population. Our cohort only involved patients who were discharged from the ICU to the ward and excluded those who were severely ill or needed palliative care, and not ICU management (i.e., those who died in ICU, those who were transferred to another hospital, or those who agreed to sign a do-not-resuscitate form). Therefore, the results on postoperative ICU admission or mechanical ventilator use in the ICU need to be interpreted carefully, because these factors were not causal factors for lowering unplanned readmission rates, but reflected the characteristics of the study population
In our cohort, 19.0% (703/3,707) of the patients were not postoperatively admitted to the ICU but were rather admitted from the emergency department or ward. While many patients who undergo elective surgery are postoperatively admitted to the ICU only for continuous monitoring (31), surgical patients who are admitted to the ICU from the emergency department or ward may have more severe illnesses such as sepsis or bleeding. In these patients, the peak lactate level may reflect the disease severity, since an elevated lactate level is a useful marker for the severity of acute illness in critically ill patients (32). Therefore, the peak lactate level during ICU stay in this cohort reflects not only the severity of critical illness, but also predicts unplanned ICU readmission.
A recent study by Martin et al. suggested that a validated clinical nomogram, which was derived from seven physiologic and demographic variables, could predict unplanned ICU readmission within 72 h among surgical patients (33). In their study, the clinical nomogram had an AUC of 0.71 for predicting unplanned ICU readmission within 72 h, which is relatively higher than that of the peak lactate level (0.63) or initial lactate level (0.61) in our study. However, the clinical nomogram was validated using seven physiologic and demographic variables (33), and we only used one variable, that is, lactate levels. Thus, if the lactate level during ICU admission is combined with other variables for developing a new model for predicting the risk of unplanned ICU admission, this model will have more predictive power. Future studies are needed to validate a new model or scoring system for predicting unplanned ICU readmission among surgical patients.
This study has some limitations. First, because this was retrospective cohort study, there were several confounders that should be controlled. Second, the generalizability of our findings may be limited, because the study was conducted in a single center. Third, many patients (7,019 patients) were excluded because their lactate level was not measured, and this could have affected the patient characteristics. For instance, relatively healthy patients whose lactate level did not need to be assessed during ICU admission may have been excluded from the final analysis. Lastly, the timing of measurement of lactate levels differed, and this could have led to bias.
In conclusion, this study showed that in surgical ICU patients, the peak lactate level during ICU admission was independently associated with unplanned ICU readmission within both, 48 and 120 h. However, the lactate level alone has relatively poor predictive capability for unplanned ICU readmission, and thus, a new model is needed.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-291
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-291
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-291). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This retrospective cohort study was conducted in a single tertiary academic hospital and was approved by the Institutional Review Board (IRB) of Seoul National University Bundang Hospital (SNUBH) (IRB approval number: B-1904/534-103). The requirement for informed consent was waived owing to the retrospective design of this study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Berenholtz SM, Dorman T, Ngo K, et al. Qualitative review of intensive care unit quality indicators. J Crit Care 2002;17:1-12. [Crossref] [PubMed]
- Rhodes A, Moreno RP, Azoulay E, et al. Prospectively defined indicators to improve the safety and quality of care for critically ill patients: a report from the Task Force on Safety and Quality of the European Society of Intensive Care Medicine (ESICM). Intensive Care Med 2012;38:598-605. [Crossref] [PubMed]
- Elliott M, Worrall-Carter L, Page K. Intensive care readmission: a contemporary review of the literature. Intensive Crit Care Nurs 2014;30:121-37. [Crossref] [PubMed]
- Kramer AA, Higgins TL, Zimmerman JE. The association between ICU readmission rate and patient outcomes. Crit Care Med 2013;41:24-33. [Crossref] [PubMed]
- Brown SE, Ratcliffe SJ, Kahn JM, et al. The epidemiology of intensive care unit readmissions in the United States. Am J Respir Crit Care Med 2012;185:955-64. [Crossref] [PubMed]
- Al-Jaghbeer MJ, Tekwani SS, Gunn SR, et al. Incidence and Etiology of Potentially Preventable ICU Readmissions. Crit Care Med 2016;44:1704-9. [Crossref] [PubMed]
- de Lima VC, Bierrenbach AL, Alencar GP, et al. Increased risk of death and readmission after hospital discharge of critically ill patients in a developing country: a retrospective multicenter cohort study. Intensive Care Med 2018;44:1090-6. [Crossref] [PubMed]
- Jeong BH, Na SJ, Lee DS, et al. Readmission and hospital mortality after ICU discharge of critically ill cancer patients. PLoS One 2019;14:e0211240. [Crossref] [PubMed]
- Kareliusson F, De Geer L, Tibblin AO. Risk prediction of ICU readmission in a mixed surgical and medical population. J Intensive Care 2015;3:30. [Crossref] [PubMed]
- Ponzoni CR, Correa TD, Filho RR, et al. Readmission to the Intensive Care Unit: Incidence, Risk Factors, Resource Use, and Outcomes. A Retrospective Cohort Study. Ann Am Thorac Soc 2017;14:1312-9. [Crossref] [PubMed]
- Kramer AA, Higgins TL, Zimmerman JE. Intensive care unit readmissions in U.S. hospitals: patient characteristics, risk factors, and outcomes. Crit Care Med 2012;40:3-10. [Crossref] [PubMed]
- Broder G, Weil MH. Excess Lactate: An Index of Reversibility of Shock in Human Patients. Science 1964;143:1457-9. [Crossref] [PubMed]
- Weil MH, Afifi AA. Experimental and clinical studies on lactate and pyruvate as indicators of the severity of acute circulatory failure (shock). Circulation 1970;41:989-1001. [Crossref] [PubMed]
- Vincent JL, De Backer D. Circulatory shock. N Engl J Med 2013;369:1726-34. [Crossref] [PubMed]
- James JH, Luchette FA, McCarter FD, et al. Lactate is an unreliable indicator of tissue hypoxia in injury or sepsis. Lancet 1999;354:505-8. [Crossref] [PubMed]
- Jones AE, Puskarich MA. Sepsis-induced tissue hypoperfusion. Crit Care Clin 2009;25:769-79. ix. [Crossref] [PubMed]
- Kompanje EJ, Jansen TC, van der Hoven B, et al. The first demonstration of lactic acid in human blood in shock by Johann Joseph Scherer (1814-1869) in January 1843. Intensive Care Med 2007;33:1967-71. [Crossref] [PubMed]
- Rogatzki MJ, Ferguson BS, Goodwin ML, et al. Lactate is always the end product of glycolysis. Front Neurosci 2015;9:22. [Crossref] [PubMed]
- Heigenhauser GJ, Parolin ML. Role of pyruvate dehydrogenase in lactate production in exercising human skeletal muscle. Adv Exp Med Biol 1999;474:205-18. [Crossref] [PubMed]
- Vincent JL, Quintairos ESA, Couto L Jr, et al. The value of blood lactate kinetics in critically ill patients: a systematic review. Crit Care 2016;20:257. [Crossref] [PubMed]
- Oh TK, Song IA, Jeon YT. Peri-operative serum lactate level and postoperative 90-day mortality in a surgical ICU: A retrospective association study. Eur J Anaesthesiol 2020;37:31-7. [Crossref] [PubMed]
- Oh TK, Song IA, Bae HJ, et al. Serum lactate level upon admission to the neuro-intensive care unit and 90-day mortality: A retrospective study. J Clin Neurosci 2019;70:173-7. [Crossref] [PubMed]
- Yoo S, Lee KH, Lee HJ, et al. Seoul National University Bundang Hospital's electronic system for total care. Healthc Inform Res 2012;18:145-52. [Crossref] [PubMed]
- Woodhouse D, Berg M, van der Putten J, et al. Will benchmarking ICUs improve outcome? Curr Opin Crit Care 2009;15:450-5. [Crossref] [PubMed]
- SCCM Quality Indicators Committee. Candidate Critical Care Quality Indicators. Anaheim. CA, Society of Critical Care Medicine 1995.
- Hajjar LA, Almeida JP, Fukushima JT, et al. High lactate levels are predictors of major complications after cardiac surgery. J Thorac Cardiovasc Surg 2013;146:455-60. [Crossref] [PubMed]
- Li S, Peng K, Liu F, et al. Changes in blood lactate levels after major elective abdominal surgery and the association with outcomes: a prospective observational study. J Surg Res 2013;184:1059-69. [Crossref] [PubMed]
- Marnitz U, Dauberschmidt R, Mrochen H. The value of blood lactate determination in the postoperative phase. Anaesthesiol Reanim 1994;19:103-9. [PubMed]
- Haanschoten MC, Kreeftenberg HG, Arthur Bouwman R, et al. Use of Postoperative Peak Arterial Lactate Level to Predict Outcome After Cardiac Surgery. J Cardiothorac Vasc Anesth 2017;31:45-53. [Crossref] [PubMed]
- Creagh-Brown BC, De Silva AP, Ferrando-Vivas P, et al. Relationship Between Peak Lactate and Patient Outcome Following High-Risk Gastrointestinal Surgery: Influence of the Nature of Their Surgery: Elective Versus Emergency. Crit Care Med 2016;44:918-25. [Crossref] [PubMed]
- Kahan BC, Koulenti D, Arvaniti K, et al. Critical care admission following elective surgery was not associated with survival benefit: prospective analysis of data from 27 countries. Intensive Care Med 2017;43:971-9. [Crossref] [PubMed]
- Kushimoto S, Akaishi S, Sato T, et al. Lactate, a useful marker for disease mortality and severity but an unreliable marker of tissue hypoxia/hypoperfusion in critically ill patients. Acute Med Surg 2016;3:293-97. [Crossref] [PubMed]
- Martin LA, Kilpatrick JA, Al-Dulaimi R, et al. Predicting ICU readmission among surgical ICU patients: Development and validation of a clinical nomogram. Surgery 2019;165:373-80. [Crossref] [PubMed]



