
Barriers to palliative care use among surgical patients: perspectives of practicing surgeons across Michigan
Introduction
The American College of Surgeons (ACS) has increasingly supported initiatives to better incorporate palliative care principles into surgery (1). In 2005, the ACS expanded their “Statements of Principles of Palliative Care” to broaden palliative care’s reach to surgical patients beyond end-of-life care (2,3). Initially focused on cancer patients and those with terminal or life-threatening chronic illnesses, palliative care has proven beneficial for a wider range of seriously-ill patients (4,5). Surgical patients, specifically, are distinct from patients with chronic and/or terminal illnesses in that they often experience rapid changes in health status. Providers with expertise in managing prognostic uncertainty and eliciting patient and family values help by facilitating goal-concordant care at the same time providing relief from the physical and emotional symptoms related to their underlying illnesses and burdensome treatments.
However, despite the benefits of palliative care, surgical patients are less likely to receive palliative care consultations when compared to their medical counterparts (6-8). When palliative care referrals do occur, they are often performed within 24–48 hours of death (7,9,10), which is associated with poorer symptom control and more aggressive interventions at the end of life (11,12). Recent studies attempt to explain this underuse as a consequence of surgeons’ misconceptions of the role of palliative care and the discomfort in introducing these services to patients and families. This is largely attributed to a lack of exposure to palliative care during training (13-16). Although these data provide some insight into how surgeons make decisions about the management of seriously-ill and dying patients, much of this work is limited by survey methods and sampling from single institutions or a single surgical subspecialty (17). The factors influencing how surgeons employ palliative care approaches (i.e., primary palliative care skills performed by the surgical team), as well as refer to palliative care services (i.e., specialty palliative care support obtained through consultation) is poorly characterized.
In this context, we conducted semi-structured interviews with a diverse range of practicing surgeons across the state of Michigan to gain an in-depth understanding of surgeon attitudes and experiences with both palliative care approaches and services. We describe participants’ perceptions of how, when, and why palliative approaches and services have been and should be utilized with the overall goal of informing strategies to improve the delivery of palliative care to surgical patients.
We present the following article in accordance with the MDAR reporting checklist (available at http://dx.doi.org/10.21037/apm-20-948).
Methods
Study design
This report represents a part of a larger exploratory study designed to gain a comprehensive understanding of how surgeons make decisions about high-risk surgery. High-risk was defined as an increased likelihood of either postsurgical death (i.e., inpatient mortality of at least 1%) or poor outcomes (e.g., unexpected intensive care unit admission, prolonged hospital stay, unanticipated non-home discharge disposition) (18-20). The findings in this manuscript focus only on part of the interview—use of palliative care.
Interview participants
Purposive sampling (21) was used to recruit participants by email through the Michigan Surgical Quality Collaborative (MSQC), the Michigan Chapter of the American College of Surgeons (MCACS), and the Michigan Society of Colon and Rectal Surgeons (MSCRS). Forty-six surgeons from community, tertiary-care, and academic institutions agreed to participate in this study. Participants were selected to represent a diverse cohort with respect to age, gender, race, year in practice, type of practice, and surgical subspecialty (Table 1). Participants were eligible if they were a practicing surgeon in the state of Michigan. Participants were monetarily compensated for their participation in the interviews.
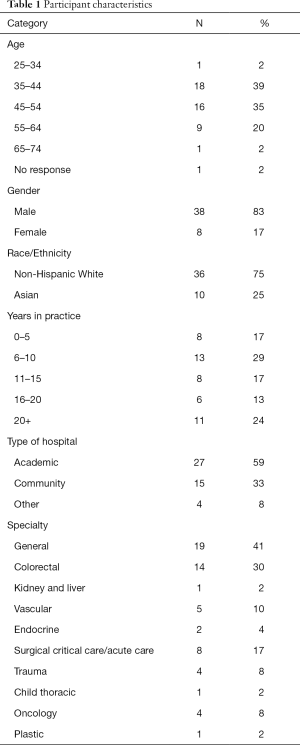
Full table
Interview procedures
All participants were provided with a written or oral informed consent statement and verbally consented before their interview. Individual interviews were conducted in-person or over the phone between October 2018 and April 2019 by two research analysts (CAV and MEB), who have expertise in qualitative interviewing, and the senior author (PAS), a surgeon and health services researcher. Two members of the research team (CAV and PAS) designed an exploratory interview guide to explore high risk decision-making for older adult (>65 years) patients (Supplement 1). Participants were asked to walk the interviewer through the steps they would take in making decisions about high-risk surgery. Participants were further prompted to consider the following as they relate to how decisions are made about high-risk surgery: the role of preoperative cognitive and functional status; the role of post-operative complications including cognitive and functional outcomes; barriers and facilitators to use of palliative care services; and surgeon responses after an unexpected post-operative outcome or complication. Three iterations of the interview guide were generated and piloted based on content validity, and presentation and clarity of information. All data, including those collected during pilot interviews, were included in the final data analysis. All interviews were digitally recorded and lasted between 30 and 60 minutes. Audiotapes were transcribed verbatim and de-identified for names and places. Transcripts were not returned to participants for review.
Analysis
The data were analyzed through iterative steps informed by thematic analysis (22). Five members of the research team independently identified an initial set of codes. The team then met to discuss the codes and map them to a coding schema, creating a codebook based on overarching domains. Due to the exploratory nature of the interview instrument, the initial coding process was kept intentionally broad, and focused on organizing data into overarching domains. Two members of the research team (CAV and ACD) independently coded transcripts, meeting regularly to discuss discrepancies and modify the codebook when necessary. From there, each domain was assigned to a research member based on research interest. A codebook for the palliative care domain was created iteratively with involvement from the entire research team. Transcribed interviews were coded in MAXQDA (version 18.2.3, VERBI Software, Berlin, Germany), a computer-assisted, qualitative data analysis software. Microsoft Excel (version 16.16.20, Microsoft Corporation, Redmond, WA) was used to assist with synthesizing and categorizing results.
This study was deemed exempt by the University of Michigan Medicine Institutional Review Board (IRBMED HUM00157651).
Results
Six major themes emerged describing surgeon-reported barriers to palliative care approaches and use of palliative care services, which were observed at the surgeon-level, patient and family-level, and system-level.
At the surgeon-level, the following three major themes emerged:
At the patient and family-level, two major themes were identified:
At the system-level, two major themes emerged:
Themes are summarized with illustrative quotes in Tables 2-4.
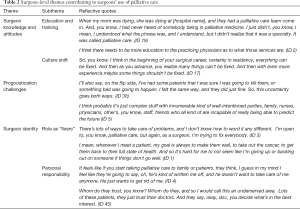
Full table

Full table
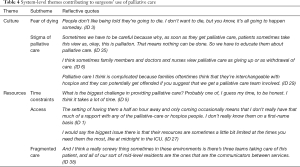
Full table
Surgeon-level barriers
Surgeon knowledge and attitudes
When reflecting on knowledge and attitudes towards palliative care, surgeons reported limited knowledge of evidence regarding both palliative care approaches and specialty services; specifically, the benefits of palliative care and the distinction between palliative care and hospice. For many, this was due to limited education and training surrounding palliative care. Participants described how exposure to goals of care discussions were often limited to informal training experiences, modeled by senior residents or surgeons over the course of their training, which were inherently variable. Very few reported undergoing training with experts in the management of complex, seriously-ill, or dying patients. In addition to the lack of formal training, participants also asserted a lack of knowledge regarding the palliative care services available at their institution, including uncertainty in what exactly the palliative care team would provide, as well as more logistical concerns, such as how and when to call them.
“I think barriers are more in terms of, I think I mentioned it a little before in terms of palliative care, is the lack of education of the physicians in the hospital as to what those services are. You know, what is palliative care? What are they going to do? Because obviously, patients and family members I think aren’t necessarily aware of what that is, but I think sometimes the physicians aren’t even sure what that is exactly. Do I call palliative care when they’re, you know, at what point do you call them? So, there’s lack of education.” (ID 2).
Participant beliefs were also influenced by personal experiences with palliative care teams, with some stating that their experiences interacting with specialty services for their own loved one influenced their perceptions about the benefits of palliative care.
Several participants alluded to cultural and generational shifts in improved knowledge and awareness of involving palliative care services. Younger generations of surgeons were described as being more agreeable to palliative care, noted by increased discussions and openness with patients and families within surgical contexts. This cultural shift was attributed to palliative care exposure as early as medical school and residency, as well as the evolution of the field of hospice and palliative medicine as a medical subspecialty over the last several decades. As one participant described:
“I think older generation surgeons have a misunderstanding, don’t know enough about it, don’t involve it enough.” (ID 6).
Prognostication challenges
Participants described challenges in the ability to predict the future, especially when health status can shift quickly post-surgery. For some, the decision to not refer to palliative care services was influenced by prior experiences of patients who made a full recovery despite a low likelihood of survival.
“And I can actually, this 27-year-old guy I can think of right now who is like now 37 and going to work today, you know? It’s like, what was that all about?” (ID 5).
Conversely, the decision to decline surgery or refer to palliative care services was less difficult in patients who were older, frailer, had multiple comorbidities, or were considered less likely to recover secondary to the extent of physiologic insult. For these patients, participants described greater confidence in the patient’s inability to recover, leading to a greater tendency to discuss nonoperative options or initiate referrals.
Surgeon identity
Participants described how the “fixer” identity of the surgeon played a significant role in surgeons’ willingness to discuss nonoperative management or involve palliative care services. As described by one surgeon, “that’s not why we went into medicine.” (ID 3). Participants asserted that anything less than a cure could often result in feelings of personal frustration, such that referral to palliative care services equaled defeat with the semblance of withholding care.
“I’ve had surgeons that just weren’t kind of, were used to being able to fix things, and it’s kind of that, like you don’t want to, even patients who are really sick, like trauma patients or something, we could usually do something to make them better.” (ID 4).
The perceived role of the surgeon also influenced relationships with patients and families, with participants asserting the perception that patients and/or families viewed conversations around palliative care as the surgeon giving up.
Patient and family-level barriers
Expectations
Participants described scenarios in which patients’ and families’ unrealistic expectations prevented them from considering palliative care because the patient and/or family did not or could not anticipate a poor outcome or prolonged recovery. For example, one surgeon reflected on the frequently held belief of patients and families that “if you just operate and take it out,” then “all would be fine.” (ID 2) Such expectations were described as patients’ and families’ desire to do any intervention possible, at any expense, no matter how small the chance of meaningful recovery. This optimism sometimes prevented participants from initiating palliative care conversations when they thought they should.
“The biggest roadblock that I encounter on a day-to-day basis is everyone thinks that whatever condition they have is something that we’re going to be able to cure and that it’s not going to impact their longevity.” (ID 1).
Conversely, participants reported that having ongoing, open communication helped prevent palliative care referrals from being a surprise to the family and helped to build trust and rapport. When specialty services were utilized, they were considered an important resource to meet with patients and families such that they could “understand the decisions they’re making.” (ID 2).
Discordance
Participants recognized discordance that sometimes arose with the recommendation of palliative care referral when patients and families also believed that benefit could be derived from surgery. This was reinforced in statements illustrating surgeon’s perceptions of directly opposing goals between the surgical and palliative care specialties.
“I think there’s a resistance on some of the providers. You know, that’s not what we went into medicine for, at least not why I did. You know, obviously, the people that went into palliative care, that’s kind of their area of specialty for this transition to end-of-life stuff. That’s what they’re interested in. I’m not interested in that. I want to solve every problem and have you get better and get back to being better than you were before. But obviously that’s not realistic on every patient.” (ID 3).
Participants reported that their perceptions of patient and family members’ understanding of the role of palliative medicine directly impacted their readiness to pursue consultation. These reflections suggest that surgeons feel their role in providing palliative care is better suited in performing surgical techniques to improve quality of life, and the absence of doing so resembles a contradiction to surgical training and dogma, creating inner conflict for the surgeon.
System-level barriers
Culture
Participants reported that a desire to live forever influenced how decisions regarding palliative care were made. For some, this included a desire for patients, families, and sometimes even surgeons to initiate or continue life sustaining treatment at all costs.
“The American culture, right, we’re all about keeping somebody alive, and the technology, and we can do it. We can put them on vents. You can do these things to keep them around. But at what cost, and is it really right to do that?” (ID 18).
This was distinct from the stigma of palliative care, which focused on surgeons’ and families’ reactions to palliative care, and what palliative care referrals meant. To this end, participants reflected on the need for palliative care to be reframed in how it is discussed within the wider community.
“Palliative care I think is complicated because families oftentimes think that they’re interchangeable with hospice and they can potentially get offended if you suggest that we get a palliative care team involved. When really, the goal of that is to also help define expectations, goals of care, etc. That it’s not, you know, committing the patient to any particular course of treatment or assuming a terrible outcome. But I think once you explain that to people, I mean, most people are willing to have, you know, all of that available to them, at their disposal, to help make a decision.” (ID 29).
In contrast, participants acknowledged greater social acceptance of palliative care referral during instances in which it was deemed, the “right time to let people go.” (ID 27).
Resources
Participants frequently cited time constraints as a significant barrier to engage in goals of care conversations with patients and their families specifically when providing primary palliative care approaches. One participant asserted, “I think time for me is my biggest, I guess my most precious commodity and my biggest problem at the same time.” (ID 38). In addition, even when surgeons had engaged palliative care services to conduct goals of care conversations, they struggled to find time to attend these meetings due to a need to be in the clinic or operating room.
Limited access to institutional resources affected many surgeons’ ability to utilize specialty palliative care services. Several participants reported that their institution lacked a full-time palliative care team. Several described the logistics involved with referring to a palliative care team that was not on-site, or whose long commute functioned as a deterrent. Further, the lack of in-house palliative care team led to many surgeons having weaker relationships with palliative care services.
“I leave a message asking that they come see the patient. And I’m not sure if they’re actually going to come see the patient and then, you know, no one calls, and all of a sudden, I get a, or I see a message in the chart saying that a social worker has met with the patient and their family. They’ve set up a meeting with the family to discuss palliative care and, you know, on Friday at 3:00 p.m., and it’s like Tuesday.” (ID 2).
Fragmented care affected partcipants’ willingness to utilize palliative care services. Yet, some participants saw this multidisciplinary decision-making positively, describing it as a way to gain consensus on treatment decisions. Whereas other participants described the tension of differing opinions across specialties, or difficulties in defining the division of responsibility.
“Yeah, I mean, that’s where I’m still a little bit confused, I think. When I do call them, I think it’s varied in terms of who ends up coming to see the patient. And then, you know, there’s a family meeting, and then I think that they don’t always necessarily, it gets confusing then. All of a sudden now you have the ICU team taking care of the patient. Then you’ve got the surgical team and then the palliative care team. And I think the confusion comes into, okay, well, the palliative care team has come in, and they’ve made their recommendations now, so who executes that plan now?” (ID 2).
Discussion
A surgeon’s perception of their role in medicine is shaped by deep historical roots and philosophies, intermixed with individual professional experiences. It is further impacted by the contemporaneous societal expectations of what their role should be. Atul Gawande has described the evolution of the definition of surgeon in Webster’s dictionary: in 1913, a surgeon was defined as “one whose profession or occupation is to cure diseases or injuries of the body by manual operation (23),” whereas today it is defined as “a medical specialist who practices surgery (24).” Many of the subjects in our study perceived their roles similarly to the antiquated version, as “fixers,” indicating that they identify with surgery for its technical role in medicine, as opposed to the role of a physician who treats diseases and the person as a whole. Perhaps, it is in this dated sense of identity, that many surgeons today continue to grapple with the integration of approaches introduced by newer medical specializations such as palliative care medicine, which only became formally recognized by the American Board of Medical Subspecialties in 2006.
The decision of whether to pursue curative or palliative intent surgery versus comfort care is a time-intensive and emotionally taxing venture. The constraints of limited and divided time between the operating room, other daily demands of surgical practice, and dedicated time for patient counseling can limit the robustness of these conversations between patients, loved ones, and surgeons. This directly impacts prioritizing patient autonomy and shared decision making, core principles of surgical palliative care. Given the overall increase in emergency surgeries in the United States (25), communication tools for surgeons working in high-pressure, high-stakes environments are paramount. Communication and goal concordant care conceptual models have been adapted for critically-ill patients (26), and measure the context and delivery of communication between clinicians and patients. However, data on the efficacy of these tools are minimal (27,28), and require more intensive study on its implementation to better understand their effects.
Unsurprisingly, communication was frequently discussed in tandem with the theme of prognostication challenges (17). Technology and research continue to advance the field of surgery as do prognostication tools, nomograms, and risk calculators, which can assist surgeons in decision making. Many participants described the two extremes of palliative care—circumstances characterized as “gray areas”, wherein prognostic tools are of little use, versus extremes of circumstances, wherein death or recovery are believed to be more likely (e.g., traumatic injury in older patients). These data reinforce a previously reported finding, that when uncertainty prevails and surgeon’s confidence decreases, there is the potential for negative consequences on subsequent decision-making and referrals to palliative care (29).
Surgeon-reported perceptions of limited palliative care services within their home institutions contributed to consult underutilization, despite the significant expansion of hospital palliative care services in the last decade (30). Smaller hospitals are less likely than larger ones to staff a palliative care team, highlighting the need for non-palliative care specialists to be formally trained in palliative medicine, and perhaps, specifically, surgeons due to their central role in caring for patients during critical illness. Furthermore, surgeons working at smaller hospitals may lack the same access to opportunities for observation as participants in this study, who reported learning palliative care approaches from other surgeons. These limitations to palliative care knowledge highlight the need for more educational opportunities for surgeons during training and beyond. Studies have shown that residents demonstrate increasing interest and willingness to learn about palliative care principles (31,32). Immersive palliative care training programs can significantly improve residents’ knowledge, attitudes, and skills (33), and structured teaching can improve junior residents’ knowledge to be similar to those who have learned experientially (34).
Many participants who had prior exposure to and/or training in palliative care approaches described the use of services as limited to “third party” roles in facilitating communication and establishing goals of care. These remarks assume the role of palliative care as an adjunct, rather than a core component of standard surgical practices, contradicting the established principles set forth by the American College of Surgeons Committee on Surgical Palliative Care (ACS CSPC) for advanced and serious illness (1). Although data from this study suggest that younger generations of surgeons are more aware of the need to involve palliative care services, little is known regarding the use of palliative care approaches among surgeons without specialty palliative care training.
There were limitations to this study that should be addressed. Inherent to qualitative research, our study sample is not generalizable to all surgeons or practice settings. However, we purposively sampled a diverse cohort by specialty, age, experience, and practice setting. Further, social desirability bias may influence some responses about their typical approaches to high-stakes decision making, as surgeons may feel there is a “correct answer” to some of these questions. Despite this possibility, many of the participants were interviewed through the Michigan Surgical Quality Collaborative, which is a community of surgeons that have exhibited high vulnerability in past studies and interactions in an effort to improve care for surgical patients across Michigan. Finally, in pursuit of drawing out participants’ complete understanding of palliative care, we did not specifically ask about their understanding of the differences between primary palliative care approaches and palliative care services. However, we have no reason to believe that the lack of standardized definitions provided to the participants would alter their responses to the challenges they encounter when communicating and managing seriously ill and complex patients.
Conclusions
Our study adds to the growing body of literature identifying surgeon-reported barriers to the use of palliative care approaches and services among surgical patients. Our research strives to elevate the understanding surgeon experiences that will further aid in the implementation of much needed strategies to better assist surgeons’ use of palliative approaches and consultative services for their patients.
Acknowledgments
The authors would like to thank the participants who participated in these interviews and the Michigan Surgical Quality Collaborative for assistance recruiting surgeon subjects and promoting this study.
Funding: This project was funded by the Thomas R. Russell Faculty Research Fellowship from the American College of Surgeons, Society of Surgery of the Alimentary Tract and Research Foundation of the American Society of Colon and Rectal Surgeons Joint Faculty Research Award, and the National Institute on Aging Grants for Early Medical/Surgical Specialists’ Transition to Aging Research (GEMSSTAR, R03 AG056588-02).
Footnote
Reporting Checklist: The authors have completed the MDAR reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-948
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-948). PAS serves as an unpaid editorial board member of Annals of Palliative Medicine from May 2019 to Apr 2021. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dunn GP. Surgery, palliative care, and the American College of Surgeons. Ann Palliat Med 2015;4:5-9. [PubMed]
- Bulletin of the American College of Surgeons. Statement of Principles of Palliative Care. 2005.
- Sigman M, Miller P. Practicing primary palliative care: A call to action. 2019.
- Enguidanos S, Vesper E, Lorenz K. 30-day readmissions among seriously ill older adults. J Palliat Med 2012;15:1356-61. [Crossref] [PubMed]
- Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010;363:733-42. [Crossref] [PubMed]
- Kross EK, Engelberg RA, Downey L, et al. Differences in end-of-life care in the icu across patients cared for by medicine, surgery, neurology, and neurosurgery physicians. Chest 2014;145:313-21. [Crossref] [PubMed]
- Olmsted CL, Johnson AM, Kaboli P, et al. Use of Palliative care and hospice among surgical and medical specialties in the veterans health administration. JAMA Surg 2014;149:1169-75. [Crossref] [PubMed]
- Rodriguez KL, Barnato AE, Arnold RM. Perceptions and utilization of palliative care services in acute care hospitals. J Palliat Med 2007;10:99-110. [Crossref] [PubMed]
- Rodriguez R, Marr L, Rajput A, et al. Utilization of palliative care consultation service by surgical services. Ann Palliat Med 2015;4:194-9. [PubMed]
- Wilson DG, Harris SK, Peck H, et al. Patterns of care in hospitalized vascular surgery patients at end of life. JAMA Surg 2017;152:183-90. [Crossref] [PubMed]
- Pizzo PA, Walker DM. Should we practice what we profess? care near the end of life. N Engl J Med 2015;372:595-8. [Crossref] [PubMed]
- Teno JM, Gozalo PL, Bynum JPW, et al. Change in end-of-life care for medicare beneficiaries: Site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA 2013;309:470-7. [Crossref] [PubMed]
- Suwanabol PA, Reichstein AC, Suzer-Gurtekin ZT, et al. Surgeons’ perceived barriers to palliative and end-of-life care: A mixed methods study of a surgical society. J Palliat Med 2018;21:780-8. [Crossref] [PubMed]
- Ball CG, Navsaria P, Kirkpatrick AW, et al. The impact of country and culture on end-of-life care for injured patients: Results from an international survey. J Trauma 2010.691323-33; discussion 1333-4. [Crossref] [PubMed]
- Hurdle V, Ouellet JF, Dixon E, et al. Does regional variation impact decision-making in the management and palliation of pancreatic head adenocarcinoma? Results from an international survey. Can J Surg 2014;57:E69-E74. [Crossref] [PubMed]
- Cauley CE, Block SD, Koritsanszky LA, et al. Surgeons’ Perspectives on Avoiding Nonbeneficial Treatments in Seriously Ill Older Patients with Surgical Emergencies: A Qualitative Study. J Palliat Med 2016;19:529-37. [Crossref] [PubMed]
- Suwanabol PA, Kanters AE, Reichstein AC, et al. Characterizing the Role of U.S. Surgeons in the Provision of Palliative Care: A Systematic Review and Mixed-Methods Meta-Synthesis. J Pain Symptom Manage 2018;55:1196-215.e5. [Crossref] [PubMed]
- Schwarze ML, Barnato AE, Rathouz PJ, et al. Development of a list of high-risk operations for patients 65 years and older. JAMA Surg 2015;150:325-31. [Crossref] [PubMed]
- Weingart SN, Iezzoni LI, Davis RB, et al. Use of administrative data to find substandard care: Validation of the complications screening program. Med Care 2000;38:796-806. [Crossref] [PubMed]
- Iezzoni LI, Daley J, Heeren T, et al. Identifying complications of care using administrative data. Med Care 1994;32:700-15. [Crossref] [PubMed]
- Bernard HR. Research methods in anthropology: Qualitative and quantitative approaches. Walnut Creek, CA: AltaMira Press, 2001.
- Clarke V, Braun V. Thematic analysis. J Posit Psychol 2017;12:297-8. [Crossref]
- Webster N. Webster’s Revised Unabridged Dictionary. Available online: https://www.swordsearcher.com/bible-study-library/webster-1913-dictionary.html
- Merriam-Webster.com. Surgeon [Internet]. [cited 2020 Mar 28]. Available online: https://www.merriam-webster.com/dictionary/surgeon
- Gale SC, Shafi S, Dombrovskiy VY, et al. The public health burden of emergency general surgery in the United States: A 10-year analysis of the Nationwide Inpatient Sample - 2001 to 2010. J Trauma Acute Care Surg 2014;77:202-8. [Crossref] [PubMed]
- Sanders JJ, Curtis JR, Tulsky JA. Achieving Goal-Concordant Care: A Conceptual Model and Approach to Measuring Serious Illness Communication and Its Impact. J Palliat Med 2018;21:S17-S27. [Crossref] [PubMed]
- Lilley EJ, Cooper Z, Schwarze ML, et al. Palliative Care in Surgery: Defining the Research Priorities. Ann Surg 2018;267:66-72. [Crossref] [PubMed]
- Cooper Z, Koritsanszky LA, Cauley CE, et al. Recommendations for best communication practices to facilitate goal-concordant care for seriously ill older patients with emergency surgical conditions. Ann Surg 2016;263:1-6. [Crossref] [PubMed]
- Lee CW, Vitous CA, Silveira MJ, et al. Delays in Palliative Care Referral Among Surgical Patients: Perspectives of Surgical Residents Across the State of Michigan. J Pain Symptom Manage 2019;57:1080-8. [Crossref] [PubMed]
- America’s Care of Serious Illness: A State-by-State Report Card on Access to Palliative Care in Our Nation’s Hospitals [Internet]. 2019. Available online: https://reportcard.capc.org/wp-content/uploads/2019/09/CAPC_ReportCard19-Digital_9_19.pdf
- Rappaport W, Prevel C, Witzke D, et al. Education about death and dying during surgical residency. Am J Surg 1991;161:690-2. [Crossref] [PubMed]
- Klaristenfeld DD, Harrington DT, Miner TJ. Teaching palliative care and end-of-life issues: A core curriculum for surgical residents. Ann Surg Oncol 2007;14:1801-6. [Crossref] [PubMed]
- Raoof M, O’Neill L, Neumayer L, et al. Prospective evaluation of surgical palliative care immersion training for general surgery residents. Am J Surg 2017;214:378-83. [Crossref] [PubMed]
- Bradley CT, Webb TP, Schmitz CC, et al. Structured teaching versus experiential learning of palliative care for surgical residents. Am J Surg 2010;200:542-7. [Crossref] [PubMed]


