
The characteristics of ICU physical restraint use and related influencing factors in China: a multi-center study
Introduction
Physical restraint refers to the use of any physical or mechanical equipment, materials or tools to attach or be adjacent to the patient’s body so that the patient cannot be easily removed to restrict the patient’s free movement or prevent the patient from approaching some spaces (1). The use of physical restraint has become a common phenomenon in clinical practice at home and abroad, especially in the intensive care units (ICUs). Due to the unfamiliar treatment environment, the suffering of the disease, and the particularity of treatment, patients often experience nervousness, restlessness, thus they can unintentionally remove some important tubes for life supporting, such as tracheal intubation, central venous catheter (CVC) and other various drainage tubes (2). These acts not only cause physical trauma to the patient, but also bring a lot of treatment disturbances and risks (3). Therefore, ICU nurses often use physical restraints on patients during the nursing process to temporarily limit their activities to ensure the safety of patients and the smooth progress of treatment, so that the use of physical restraints is more common than other general departments among hospitals (4).
It’s been reported that although ICU accounts for about one-fifth of the total number of beds in hospitals, the use of physical restraints accounts for more than half of hospitals (5,6). A Canadian survey (7) on the use of physical restraint in mechanical ventilation patients have showed that about half of mechanically ventilated patients are physically restrained at least once during the period of ICU stay, with an average use of 4.1 days, of which 53% patients continue to use restraint more than 1 day. The incidence of physical restraint use in China is rather higher. Gu et al. (8). reported that 69.4% of ICU patients were physically restrained once or more. Chen et al. (9) conducted a survey on 102 ICU patients in Nanjing, and the result has showed that the incidence of physical constraints is 45.7%. Furthermore, there are many problems in the process of physical restraint use, such as unclear use indications, lack of relevant medical orders, and failure to inform family members or patients the details of physical restraint use et al. (10,11).
There have been many surveys on the current status of ICU physical restraint use in home and abroad, but the sample size of the reported surveys is relatively small. Multi-center survey with larger sample sizes on the current status and potential predicators of ICU patients’ physical restraint use are needed. The use of physical restraints can be affected by many factors. To regulate the use of physical restraints in ICUs and develop effective strategies and related guidelines for reducing the use of restraints, we must firstly understand the current status of physical restraints in ICU patients and related influencing factors. The purpose of this study is to evaluate the status of physical restraint use of patients in ICU, and to identify the potential factors affecting the physical restraint use, thereby providing theoretical basis for formulating targeted interventions in ICU practices.
We present the following article in accordance with the MDAR reporting checklist (available at http://dx.doi.org/10.21037/apm-20-563).
Methods
Ethical considerations
This present study was approved by the Medical Research Ethics Committee of our hospital (No. 20191068), and written informed consents were obtained from all the participants. And the study conformed to the provisions of the Declaration of Helsinki (as revised in 2013).
Participants
Our study design was a cross-sectional investigative study. The patients in 16 ICUs of five hospitals from September 15 to October 15, 2019 were included. The inclusion criteria were the stay of patients must be ≥24 h and age ≥18 years old. The exclusion criteria were: patients with a history of mental illness; patients in close isolation, or protective isolation.
Survey process
On-site investigations were conducted in the ICUs by two of our investigators after uniform training. We used the ICU Patients’ Physical Restraint Evaluation Scale (12) as survey tool. It’s been well-documented that the Cronbach’s coefficient of the total score of the evaluation scale was 0.704, and the intra-evaluator correlation coefficient (ICC) was 0.946. The assessment scale is composed of two parts, the basic information form and the assessment content scale. The basic information includes: the patient’s gender, age, bed number, hospitalization number, main clinical diagnosis, and physical restraint site. The assessment content form includes the behavioral, treatment and muscle strength level in three dimensions for ICU patients, with 35 detailed items for evaluation. Specifically, the tube importance judgement related to life was referred to previous report (13).
Before the data collection, the nurses who participated in the data collection were trained uniformly before the survey began, and the nurses were instructed to explain the survey purpose, method, meaning, requirements for completing the questionnaire, and the time required to complete the survey by using unified guidelines. In the process of data collection, investigators made clinical observations, consultation with the nurses in charge, and checked the medical records. When the questionnaire was recovered, the investigator rechecked the nursing process sheet and other medical records. If there were missing items and obvious logical errors, they were verified personally and modified accordingly.
Statistical analyses
All collected data were recorded and analyzed using SPSS 23.0 software. The statistical descriptions were presented as frequency or rate, χ2 tests were used for comparisons. The continuous values were presented as mean and standard deviation, and t-tests were performed for data comparison. According to that whether to use physical restraint as the dependent variable, we set potential related factors that influence the occurrence of physical restraint as independent variables, and statistically significant indicators were further applied to multivariate logistic regression models. P<0.05 was considered statistically significant in this present study.
Results
The characteristics of included patients
Of the 16 ICUs of five hospitals, a total of 386 patients were included in this present study, of which 228 patients have undergone physical restraint use, and the incidence of physical restraint use among the investigated ICU patients was 59.07%. As Table 1 presented, we included 119 female patients and 267 male patients, and the majority of the length of ICU stay was less than 1 week. And mechanical ventilation treatments were applied for 117 patients. Moreover, 89.64% patients received the treatments related to catheter or tube use.

Full table
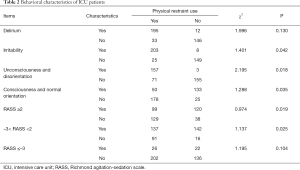
The behavioral characteristics of ICU patients
As Table 2 presented, the incidence of physical restraint uses in patients with irritability, unconsciousness and disorientation, Richmond agitation-sedation scale (RASS) ≥2 or –3< RASS <2 was significantly higher that other conditions (all P<0.05).
Full table
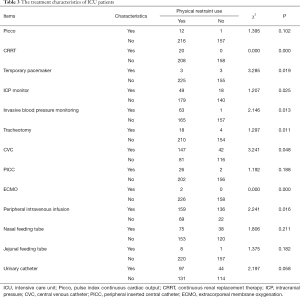
The treatment characteristics of ICU patients
As Table 3 presented, the incidence of physical restraint uses in patients with continuous renal replacement therapy (CRRT), temporary pacemaker, intracranial pressure (ICP) monitor, invasive blood pressure monitoring, tracheotomy, CVC, extracorporeal membrane oxygenation (ECMO), peripheral intravenous infusion was significantly higher that other conditions (all P<0.05).
Full table
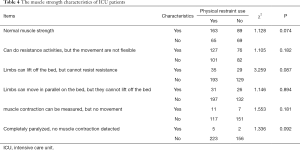
The muscle strength characteristics of ICU patients
As Table 4 presented, no significant differences in the muscle strength characteristics on the restraint use were found (all P>0.05).
Full table
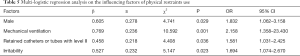
The influencing factors of physical restraints use
As Table 5 showed, the male gender, mechanical ventilation, retained catheters or tubes with level II or irritability were the independently influencing factors for the physical restraint use (all P<0.05).
Full table
Discussion
There is a trend of reducing the use of ICU physical restraint in recent years (14). In this present study, the incidence of restraint use among the 16 ICUs is 59.07%, which is slightly higher than that previous reports (15,16). It is worth-noting that there are currently many countries with a low rate of ICU physical restraint. There were two ICUs in Turkey and four ICUs in the United Kingdom did not use physical restraint (17). Therefore, there is still much room for improvement in reducing the use of physical restraint use in ICU. The results of this present study have found that the patients with male gender, mechanical ventilation, retained catheters or tubes with level II or irritability have higher risks of physical restraint use.
The results of this study indicate that male ICU patients are more likely to be physically restrained. This is consistent with the reported results of Mion et al. (18). This may be because male patients are more prone to restlessness and discomfort with treatment, which is also the focus of physical restraint (19). The incidence of using physical restraint by patients with agitation is higher than that of patients in quiet status. Similar conclusions were obtained in the study by Choi et al. (20). In his study, patients with agitation and carrying high-risk catheters accounts for 70.2% among the patients with physical restraint behavior. This also suggests that the correct assessment of the patient’s behavioral status can be used as an important aspect of the development of physical restraint decision-making assessment tools, especially the level assessment of patient agitation behavior (21).
Nearly all patients with mechanical ventilation use physical restraint to prevent any unplanned extubation, although a number of studies (22-24) have confirmed that physical restraint produce no significant effect in preventing accidental extubation related to mechanical ventilation. Some studies (25,26) have suggested that the main reason for the ineffective effect of physical restraint in preventing mechanical ventilation extubation is caused by improper physical restraint methods, such as loose restraint, etc., but some experts (2,27) believe that proper fixation of the catheters, timely meeting the various needs of patients with mechanical ventilation, and the provision of auxiliary expression tools are the fundamental effective measures to prevent unplanned extubation (3).
Prospective studies (28-30) have found that the use of sedatives is the most obvious predictor of ICU physical restraint use. However, the impact of sedative drugs on physical restraint is more complicated. On one hand, patients who need sedation generally have a certain degree of agitation, so they are more likely to be physically restrained (31). On the other hand, insufficient sedation will increase the use of restraints (32). For example, a survey (7) showed that patients with sedation and agitation score <3 had a significantly longer restraint time. And patients on daily sedation discontinuation regimens are significantly more likely to be constrained than other sedative patients (33). This may be due to insufficient sedation to control patient’s agitation, yet excessive sedation may cause other behavioral reactions, but both will increase the risk of physical restraint use (34). Therefore, the rational use of sedative drugs is particularly important for ICU patients (35).
It should be aware that nurses’ attitudes and beliefs on physical restraints are also key factors affecting the use of physical restraints. Previous surveys (36,37) show that most of ICU’s physical restraint decisions are made by nurses. It is therefore particularly important for nurses to have a correct and complete understanding of physical constraints (38). At present, the clinical nurse’s cognitive misunderstanding of physical restraint is exaggerating the effect of restraint use, ignoring the harm caused by restraint to patients, and at the same time using physical restraint as a method to protect themselves and reduce their workload, leading to a tendency to abuse (39,40). Previous study (41) has showed that 8% of nurses said that when there is insufficient manpower, more patients will be physically restrained to ensure medical safety. Therefore, it is necessary to actively guide the correct cognition of physical restraints of ICU nurses, enable nurses to grasp the indications of using physical restraints and know the harm that physical restraints may bring to patients (42). Furthermore, it’s necessary to learn to use physical restraints properly, and evaluate and observe patients in a timely manner (43).
Several limitations must be considered in this present study. Firstly, we took convenient sampling methods in different regions and different levels of hospitals to conduct the survey, the random and stratified sampling has not been performed, therefore, the obtained samples may be biased. Secondly, Cognitive impairment may be a risk factor of physical restraint use, there is a lack of mature and unified scales on the recognition, anxiety, depression and other mental state for ICU patients, it’s difficult for us to evaluate the relations of patient’s mental state with the restraints use. Thirdly, the sample size was rather small, it might underpower to detect the related risk factors for physical restraint use, future studies with larger sample size are needed.
In conclusion, the use of physical restraints in ICU is very common, and the patients with male gender, mechanical ventilation, retained catheters or tubes with level II or irritability may have higher risks of physical restraint use. However, limited by sample size, further interventional research should be conducted in the future to explore strategies and methods for effectively reducing and regulating ICU physical restraint use, and to evaluate the effectiveness and safety of strategies.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the MDAR reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-563
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-563
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-563). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This present study was approved by the Medical Research Ethics Committee of our hospital (No. 20191068), and written informed consents were obtained from all the participants. And the study conformed to the provisions of the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lach HW, Leach KM, Butcher HK. Evidence-based practice guideline: changing the practice of physical restraint use in acute care. J Gerontol Nurs 2016;42:17-26. [Crossref] [PubMed]
- Teece A, Baker J, Smith H. Identifying determinants for the application of physical or chemical restraint in the management of psychomotor agitation on the critical care unit. J Clin Nurs 2020;29:5-19. [Crossref] [PubMed]
- Khajeh M, Bazghaleh M, Tabarraie Y, et al. Workshop and package education intervention to knowledge, attitude and practice of ICU nurses on the use of physical restraints. J Complement Integr Med 2020. [Crossref] [PubMed]
- Via-Clavero G, Guardia-Olmos J, Gallart-Vive E, et al. Development and initial validation of a Theory of Planned Behaviour questionnaire to assess critical care nurses' intention to use physical restraints. J Adv Nurs 2019;75:2036-49. [Crossref] [PubMed]
- Fogel JF, Berkman CS, Merkel C, et al. Efficient and accurate measurement of physical restraint use in acute care. Care Manag J 2009;10:100-9. [Crossref] [PubMed]
- Mahmood SA, Mahmood OS, El-Menyar AA, et al. Self-extubation in patients with traumatic head injury: determinants, complications, and outcomes. Anesth Essays Res 2019;13:589-95. [Crossref] [PubMed]
- Luk E, Sneyers B, Rose L, et al. Predictors of physical restraint use in Canadian intensive care units. Crit Care 2014;18:R46. [Crossref] [PubMed]
- Gu T, Weng W, Wang Y, et al. Characteristics and current situation of physically restrained patients in ICU in a third-level hospital. Journal of Clinical Medicine in Practice 2018;22:118-26.
- Chen L, Li X, Chen X. The current status and analysis of physical restraint usage in intensive care unit. Chinese Nursing Management 2014;14:1022-4.
- Ye J, Xiao A, Yu L, et al. Staff training reduces the use of physical restraint in mental health service, evidence-based reflection for China. Arch Psychiatr Nurs 2018;32:488-94. [Crossref] [PubMed]
- Lam K, Kwan JSK, Wai Kwan C, et al. Factors associated with the trend of physical and chemical restraint use among long-term care facility residents in Hong Kong: data from an 11-year observational study. J Am Med Dir Assoc 2017;18:1043-8. [Crossref] [PubMed]
- Cui N, Gan X, Zhang C, et al. Construction of physical restraint assessment scale for ICU patients based on Delphi method. Journal of Nursing Science 2018;33:62-4.
- Lu H, Huang Y, Wang Y, et al. The best evidence summary of unplanned extubation prevention strategies for ICU adult tracheal tube. South China Journal of Defense Medicine 2019;9:639-42.
- Kor PP, Kwan RYC, Liu JY, et al. Knowledge, practice, and attitude of nursing home staff toward the use of physical restraint: have they changed over time? J Nurs Scholarsh 2018;50:502-12. [Crossref] [PubMed]
- Gu T, Wang X, Deng N, et al. Investigating influencing factors of physical restraint use in China intensive care units: a prospective, cross-sectional, observational study. Aust Crit Care 2019;32:193-8. [Crossref] [PubMed]
- Jiang H, Li C, Gu Y, et al. Nurses' perceptions and practice of physical restraint in China. Nurs Ethics 2015;22:652-60. [Crossref] [PubMed]
- Benbenbishty J, Adam S, Endacott R. Physical restraint use in intensive care units across Europe: the PRICE study. Intensive Crit Care Nurs 2010;26:241-5. [Crossref] [PubMed]
- Mion LC. Physical restraint in critical care settings: will they go away? Geriatr Nurs 2008;29:421-3. [Crossref] [PubMed]
- Hine K. The use of physical restraint in critical care. Nurs Crit Care 2007;12:6-11. [Crossref] [PubMed]
- Choi E, Song M. Physical restraint use in a Korean ICU. J Clin Nurs 2003;12:651-9. [Crossref] [PubMed]
- Galazzi A, Adamini I, Consonni D, et al. Accidental removal of devices in intensive care unit: an eight-year observational study. Intensive Crit Care Nurs 2019;54:34-8. [Crossref] [PubMed]
- da Silva PS, Fonseca MC. Unplanned endotracheal extubations in the intensive care unit: systematic review, critical appraisal, and evidence-based recommendations. Anesth Analg 2012;114:1003-14. [Crossref] [PubMed]
- Lucchini A, Bambi S, Galazzi A, et al. Unplanned extubations in general intensive care unit: A nine-year retrospective analysis. Acta Biomed 2018;89:25-31. [PubMed]
- Cosentino C, Fama M, Foa C, et al. Unplanned Extubations in Intensive Care Unit: evidences for risk factors. A literature review. Acta Biomed 2017;88:55-65. [PubMed]
- Chao CM, Sung MI, Cheng KC, et al. Prognostic factors and outcomes of unplanned extubation. Sci Rep 2017;7:8636. [Crossref] [PubMed]
- Chao CM, Lai CC, Chan KS, et al. Multidisciplinary interventions and continuous quality improvement to reduce unplanned extubation in adult intensive care units: A 15-year experience. Medicine (Baltimore) 2017;96:e6877. [Crossref] [PubMed]
- Ertuğrul B, Özden D. The effect of physical restraint on neurovascular complications in intensive care units. Aust Crit Care 2020;33:30-8. [Crossref] [PubMed]
- Perren A, Corbella D, Iapichino E, et al. Physical restraint in the ICU: does it prevent device removal? Minerva Anestesiol 2015;81:1086-95. [PubMed]
- van der Kooi AW, Peelen LM, Raijmakers RJ, et al. Use of physical restraints in Dutch intensive care units: a prospective multicenter study. Am J Crit Care 2015;24:488-95. [Crossref] [PubMed]
- Shehabi Y, Bellomo R, Reade MC, et al. Early goal-directed sedation versus standard sedation in mechanically ventilated critically ill patients: a pilot study*. Crit Care Med 2013;41:1983-91. [Crossref] [PubMed]
- Mehta S, Cook D, Devlin JW, et al. Prevalence, risk factors, and outcomes of delirium in mechanically ventilated adults. Crit Care Med 2015;43:557-66. [Crossref] [PubMed]
- Burry LD, Williamson DR, Perreault MM, et al. Analgesic, sedative, antipsychotic, and neuromuscular blocker use in Canadian intensive care units: a prospective, multicentre, observational study. Can J Anaesth 2014;61:619-30. [Crossref] [PubMed]
- Via-Clavero G, Sanjuan-Navais M, Romero-Garcia M, et al. Eliciting critical care nurses' beliefs regarding physical restraint use. Nurs Ethics 2019;26:1458-72. [Crossref] [PubMed]
- Pun BT, Balas MC, Barnes-Daly MA, et al. Caring for Critically Ill Patients with the ABCDEF Bundle: Results of the ICU Liberation Collaborative in Over 15,000 Adults. Crit Care Med 2019;47:3-14. [Crossref] [PubMed]
- Coursin DB, Skrobik Y. What is safe sedation in the ICU? N Engl J Med 2019;380:2577-8. [Crossref] [PubMed]
- Thibaut B, Dewa LH, Ramtale SC, et al. Patient safety in inpatient mental health settings: a systematic review. BMJ Open 2019;9:e030230. [Crossref] [PubMed]
- Wong AH, Crispino L, Parker JB, et al. Characteristics and severity of agitation associated with use of sedatives and restraints in the emergency department. J Emerg Med 2019;57:611-9. [Crossref] [PubMed]
- Mayerl H, Trummer T, Stolz E, et al. Nursing professionals' attitudes toward use of physical restraints in Styrian nursing homes Austria. Pflege 2019;32:57-63. [Crossref] [PubMed]
- Scheepmans K, Dierckx de Casterle B, Paquay L, et al. Restraint use in older adults in home care: a systematic review. Int J Nurs Stud 2018;79:122-36. [Crossref] [PubMed]
- Freeman S, Yorke J, Dark P. The management of agitation in adult critical care: Views and opinions from the multi-disciplinary team using a survey approach. Intensive Crit Care Nurs 2019;54:23-8. [Crossref] [PubMed]
- Wu D. Problems of ICU patients' physical constraints and nursing countermeasures. Anhui Meidcal Journal 2012;33:1713-5.
- Hall DK, Zimbro KS, Maduro RS, et al. Impact of a restraint management bundle on restraint use in an intensive care unit. J Nurs Care Qual 2018;33:143-8. [Crossref] [PubMed]
- Kirwan L, Coyne I. Use of restraint with hospitalized children: a survey of nurses' perceptions of practices. J Child Health Care 2017;21:46-54. [Crossref] [PubMed]


