
Factors associated with chronic thoracic spine and low back pain in caregivers of cancer patients
Introduction
Caregiving is strongly associated with physical symptoms that affect caregivers’ ability to provide care (1,2). Caregivers tend to have more health problems, such as the development of heart disease and poor wound healing, than non-caregivers of a similar age (2,3). Three symptoms particularly interfere with daily activities: heart disease, arthritis, and chronic back pain (CBP) (4). However, previous studies have mainly focused on caregiving for people with dementia, or on heart-related diseases in cancer caregivers (1-3). For example, caregivers of relatives with cancer have a greater risk of cardiovascular disease (5). One cross-sectional survey conducted 5 years after cancer diagnosis found that 14.9% of family caregivers had heart-related disease, 28.3% arthritis, and 31.5% CBP (1). There are no individual studies of CBP in caregivers.
To the best of our knowledge, there are no surveys examining the effect of cancer caregiving-related factors on CBP in family caregivers of cancer patients. Cancer caregiving follows diverse trajectories; for example, patients’ status and severity may change (through e.g., remission, recurrence, and debilitation), and this changes the status of their caregivers (6). Musculoskeletal disorders, such as CBP, are likely to occur when caregivers support patients in their daily activities. As cancer progresses, patients’ activities decrease and the physical burden of caregiving increases, which may contribute to CBP. Caregivers who perform more physical tasks show higher levels of CBP severity and longer periods of CBP than those who do not perform physical tasks (7).
CBP in family caregivers of cancer patients is associated with subjective psychological stress rather than cancer severity (1). Many family caregivers of advanced cancer patients also experience mental health problems such as lifestyle interference, and negative moods and emotions (8). Depression symptoms in family caregivers of cancer patients have a negative effect on physical health conditions such as body pain (9). Caregivers also experience high levels of sleep disturbance, which is associated with symptoms of depression and the effects of caregiving (10).
Many studies have shown that subjective psychological stress (e.g., depression, anxiety, and insomnia) affect CBP (11-15), but few have differentiated between thoracic spine and lower back pain or assessed both in a single research project. The Medical Subject Headings (MeSH) database defines back pain as pain located in the posterior regions of the thorax, lumbosacral region, or adjacent regions. The thoracic spine is generally defined as the region above the costal margin and below the neck, and the lower back as the region below the costal margin and above the inferior gluteal folds (16). Back pain is widespread, and there is a limit to what can be regarded as a single site. For example, the physical tasks of family caregivers who must lift bedridden cancer patients are related to patients’ cancer severity. It is likely that caregiver back pain is affected more by such tasks than by subjective psychological stress, and that the lower back is more burdened than the thoracic spine. It is therefore important to identify back pain location as either the thoracic spine or lower back, and examine cancer caregiving-related factors that affect CBP in each location.
It is also necessary to assess whether or not pain improvement goals are achieved. Pain intensity (PI) is often associated with a decline in body function rather than pain duration and the number of pain locations (17). Higher intensity CBP is associated with a greater likelihood of depressive symptoms (18). In palliative care, personalized pain goals (PPG), patient-reported outcomes of pain management, have increasingly become the focus of attention (19). In one study, analgesics were not required for 80% of cancer patients who achieved their pain improvement goal (20). The achievement of PPG in patients with cancer pain is associated with mild pain and atypical depression (20).
Our research goal was to test the hypothesis that factors related to caregiving for cancer patients differ according to the family caregiver’s back pain location and the achievement of pain improvement goals. We present the following article in accordance with the SURGE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-803).
Methods
Objective
A survey of CBP associated with cancer caregiving was conducted. Cancer caregiving-related factors associated with CBP in family caregivers of cancer patients were identified and categorized according to back pain location and achievement of pain improvement goals. We examined the association of cancer caregiving-related factors with the presence and absence of CBP in family caregivers of cancer patients.
Study design
This was a cross-sectional survey of family caregivers of advanced cancer patients. Participants provided demographic information by completing questionnaires (age, sex, relationship with the patient, site of CBP, PI measure, and PPG) and completed self-report questionnaires on depression, anxiety, insomnia, and caregiver burden. Participants also provided the following demographic information about the cancer patients (care recipients): age, sex, outpatient status, primary cancer site, and performance status. The patients’ time from survey until death was assessed 6 months after the survey using medical records and inquiries to the hospice institution. All dates were registered with the identification code to patient anonymity for each participant. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics committee of Kansai Medical University, Japan (No. 2015660) and informed consent was taken from all study participants. This study was registered with the University hospital Medical Information Network Clinical Trials Registry (approval number: UMIN000021639) on March 27, 2016.
Participants
The inclusion criteria were family caregivers who directly provided care to a primary family member with cancer, had at least 1 month of caregiving experience at home, and had either non-specific chronic pain or pain from specific causes, such as a herniated disc. The exclusion criteria were aged younger than 20 years, or cognitive impairments that made communication difficult. This study was conducted from 2016 to 2018 at the Kansai Medical University Hospital. During this period, 1,175 family caregivers of advanced cancer patients who visited the palliative care department were continuously enrolled in the study. Of these, 823 met the inclusion criteria. We obtained consent for participation from 351 caregivers. Of these, 31 met the exclusion criteria. A final total of 320 caregivers were included in the study.
We defined a family caregiver as a primary family member (including spouses) who directly provided care to a relative with cancer and had at least 1 month of caregiving experience at home. A definition of chronic pain based on pain duration has not been clearly established, but duration of 3 or 6 months or more is generally used (21). We therefore defined chronic pain as any subjective pain lasting for more than 6 months.
Analytical parameters
CBP site
Study participants were asked whether they had CBP (possible responses: “yes” or “no”). If they had CBP, they were instructed to touch the CBP sites and were asked whether those sites were on the thoracic spine, low back, or both.
PI
Participants evaluated their average PI during the previous 24 hours using an 11-point numerical rating scale (NRS) ranging from 0 (no pain) to 10 (worst possible pain) (22). Pain scores of 1–4 were considered to indicate mild PI, 5–6 moderate PI, and 7–10 severe PI (23). The reliability and validity of this scale have been established (24).
PPG
One way of ensuring that pain management goals are tailored to individual needs is to use a PPG, which relies on participants’ own criteria for meaningful pain relief. PPG is assessed in a similar way to PI. Family caregivers’ PPGs were assessed by asking participants “What is the maximum level of pain that would allow you to achieve comfort in physical, functional, and psychosocial domains?” Participants indicated their responses using an 11-point NRS ranging from 0 (I feel comfortable and at ease at the NRS of 0 points) to 10 (I feel comfortable even at the NRS of 10 points). There are no reports of median PPG among family caregivers with pain, and only three among cancer patients (19). However, studies have shown that PPG does not change day-to-day or during follow-up periods (20).
PPG achievement
The achievement of PPG was defined as achieving an average PI lower than or equal to the PPG (PI ≤ PPG) in the previous 24 hours (20,25).
Hospital Anxiety and Depression Scale (HADS)
Each participant completed the HADS to evaluate levels of depression and anxiety (26,27). This scale comprises 14 items scored from 0 to 3, seven for the depression subscale (HADS-D, 0–21) and seven for the anxiety subscale (HADS-A, 0–21). Higher scores indicate more severe emotional distress. The sensitivity and specificity for both HADS-D and HADS-A were approximately 0.80 (26,27). In this study, a HADS-D/HADS-A score of 8 or more was considered to indicate depression or anxiety. These cutoff points provide the optimal balance between sensitivity and specificity (26).
Japanese version of Pittsburgh Sleep Quality Index (PSQI-J)
The PSQI-J is the most frequently used scale for assessing insomnia in the previous month among family caregivers of patients with advanced cancer (28). It contains seven components: sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep difficulty, hypnotic use, and daytime dysfunction. The score for each component ranges from 0–3. The PSQI-J total score is the total score of all components; higher scores indicate poorer sleep. A PSQI-J total score cutoff point of 5.5 provides sufficient sensitivity and has been validated in caregivers of oncology patients, with a Cronbach’s α of 0.68 (29).
Japanese version of Zarit Caregiver Burden Interview (J-ZBI)
The level of caregiving burden felt by caregivers was evaluated using the J-ZBI. The higher scores indicate caregiving burden. This contains 22 questions that assess the two components of personal strain and role strain. The total possible score ranges from 0 to 88. A J-ZBI score of 24 or higher, the cutoff value for depression risk, was considered indicative of high caregiver burden (30). The J-ZBI has high test–retest reliability (r=0.76) and internal consistency (Cronbach’s alpha =0.93) (31).
Eastern Cooperative Oncology Group performance status (ECOG PS)
The ECOG PS is used by physicians to assess severity of toxicity experienced by patients in oncology treatment trials. The ECOG PS measures toxicity effects on a five-point scale: 0 is “fully active, able to carry on all pre-disease performance without restriction” and 5 indicates that the patient is deceased (32).
Sample size calculation
The sample size was set as the size that could be achieved within the 2 years of the study period. The prevalence of CBP was assumed to be 40%, from earlier studies of the general population (13,18,33,34). To examine the degree of association between the presence or absence of CBP and other factors, the error was set at 5, the reliability at 95%, and the common standard deviation at 30 for the set number of cases.
Statistical analysis
Data were reported as means with standard deviations, ranges, frequencies (%), and 95% confidence intervals (95% CI), as appropriate. When participants provided missing data, we used the worst scores in the data. Patients were classified into three groups: without CBP, with CBP (and PI ≤ PPG), and with CBP (and PI > PPG). We assessed the relationship between presence of thoracic spine/low back pain and demographics; PI; PPG; care recipients’ ECOG PS and time from survey until death; and caregivers’ HADS, PSQI-J, and J-ZBI scores using the Kruskal–Wallis test, Wilcoxon rank-sum test, and chi-square test. For variables for which the Kruskal–Wallis test indicated significant differences, the Bonferroni correction for multiple comparisons was used. Spearman’s rank correlation coefficients were calculated for the groups CBP with PI ≤ PPG and CBP PI > PPG to assess associations between thoracic spine/low back pain and demographics, HADS score, PSQI-J score, J-ZBI score, and care recipients’ ECOG PS and time from survey until death. As correlations are effect sizes, we described the strength of the effects as 0.00–0.19: very weak; 0.20–0.39: weak; 0.40–0.59: moderate; and 0.60–0.79: strong. Finally, we carried out a multivariate logistic regression analysis using the forced entry method, with the presence of thoracic spine/low back pain as the dependent variable, and HADS-D score, HADS-A score, PSQI-J score, J-ZBI score, ECOG PS (care recipients), and duration from survey until death (care recipients), as the independent variables. ECOG PS and duration from survey until death were categorical variables (ordinal scale); the other variables were continuous.
A P value of less than 0.05 was considered statistically significant. Statistical analyses were conducted using SPSS version 25.0J for Macintosh (SPSS, Inc., IBM, Chicago, IL, USA).
Results
The demographic and clinical characteristics of study participants (family caregivers) and patients (care recipients) are shown in Tables 1,2. No missing data were provided in the data of 320 caregivers. In total, 152 study participants (47.5%) reported CBP; 31.4% had chronic pain in the thoracic spine (CTSP), 28.3% had chronic pain in the lower back (CLBP), and 38 (11.9%) had experienced both CTSP and CLBP. In total, 60.0% (60/100) of those with CTSP and 46.7% (42/90) of those with CLBP had achieved their pain improvement goal.
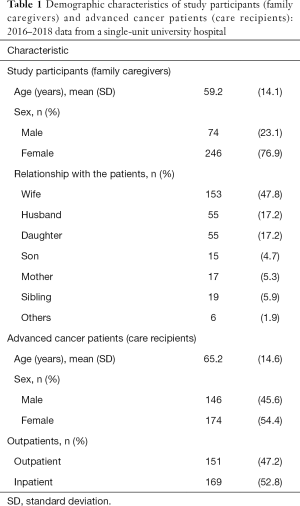
Full table
Full table
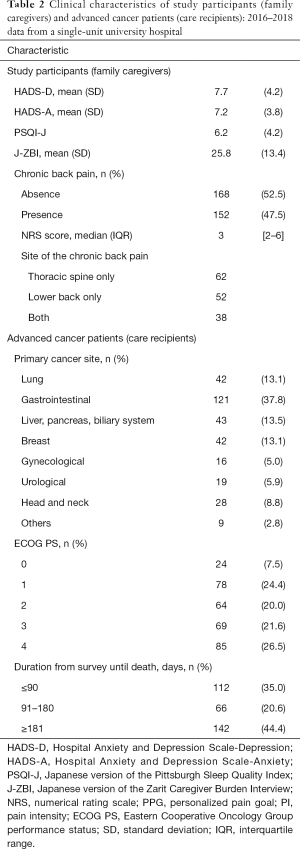
Table 3 shows a comparison of three groups: one group without CTSP and two groups with CTSP (PI ≤ PPG and PI > PPG), by demographic characteristics of both family caregivers and care recipients, family caregivers’ scores for the HADS-A, HADS-D, PSQI-J, J-ZBI, NRS, and PPG, and care recipients’ ECOG PS score and time from survey until death. Groups with CTSP (both PI ≤ PPG and PI > PPG) had significantly higher HADS-D and PSQI-J scores than the group without CTSP (P<0.001), but there was no significant difference between the two groups with CTSP (PI ≤ PPG and PI > PPG) (P=1.000). The group with CTSP (PI > PPG) had higher J-ZBI scores than the group without CTSP, and there was a significant between-group difference (P=0.001). No significant difference was found on this measure between the two groups with CTSP (PI ≤ PPG and PI > PPG) (P=0.270). The group with CTSP (PI > PPG) had a higher HADS-A score, but this was not significantly different from the HADS-A score of the group without CTSP (P=0.291) and the group with CTSP (PI ≤ PPG) (P=0.067).
Full table
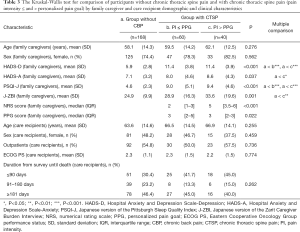
Table 4 shows the same comparison as Table 3, but for CLBP. The group with CLBP (PI > PPG) had significantly higher J-ZBI scores than the groups without CLBP and with CLBP (PI ≤ PPG) (P=0.001), but there was no significant difference between the groups without CLBP and with CLBP (PI ≤ PPG) (P=1.000). The groups with CLBP (PI ≤ PPG and PI > PPG) had significantly higher scores than the group without CLBP for both the HADS-D (P=0.023 and P<0.001) and PSQI-J (P=0.010 and P<0.001). However, there was no significant difference between the two groups with CLBP (PI ≤ PPG and PI > PPG) (HADS-D: P=0.689; PSQI-J: P=0.225). The group with CLBP (PI > PPG) had significantly higher ECOG PS scores and shorter time from survey until death than the groups without CLBP and with CLBP (PI ≤ PPG) (P<0.001), but there was no significant difference between the groups without CLBP and with CLBP (PI ≤ PPG) (P=1.000). The group with CLBP (PI > PPG) was older, and there was a significant age difference between the groups with CLBP (PI > PPG) and without CLBP (P=0.040), but no significant difference between the groups with CLBP (PI ≤ PPG) and without CLBP (P=1.000). For outpatients, there was a significant difference between the three groups; the scores for the groups with CLBP (PI ≤ PPG and PI > PPG) were not significantly higher than those for the group without CLBP (P=0.248 and P=0.086).
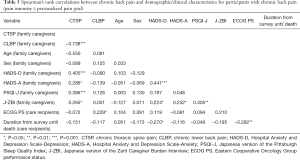
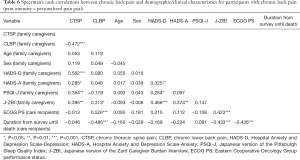
Full table
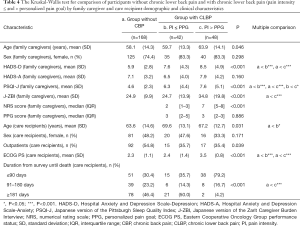
Table 5 shows the correlation coefficients for comparisons between sets of the following variables: CTSP; CLBP; age; sex; HADS-A, HADS-D, PSQI-J, and J-ZBI scores; ECOG PS; and time from survey until death for the CBP with PI ≤ PPG group. Table 6 shows the same comparison for the CBP with PI > PPG group.
Full table
Full table
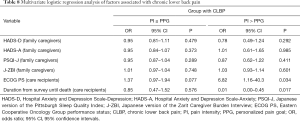
The logistic regression analysis showed that HADS-D score was associated with CTSP (both PI ≤ PPG and PI > PPG) (P=0.001 and P=0.027), and PSQI-J score was associated with CTSP (PI > PPG) (P=0.018) (Table 7). Table 8 shows that the ECOG PS and time from survey until death was associated with CLBP (PI > PPG) (P=0.034 and P=0.017).

Full table
Full table
Discussion
To the best of our knowledge, this is the first report of an individual survey of cancer caregiving-related factors that affect CBP in family caregivers.
There was a high proportion of women among the family caregivers in this study, particularly wives of care recipients, and they reported a high level of subjective stress. More than half of care recipients had terminal cancer and had a prognosis of less than 6 months, but their cancer severity was not associated with the ECOG PS score. There is only one previous study on CBP in family caregivers; this was carried out 5 years after the care recipients’ cancer diagnosis and showed that 31.5% of family caregivers complained of CBP (1). We found a higher percentage of CBP (47.5%) in this study. However, family caregivers in the previous study may have had a lower physical burden because the study included caregivers of cancer survivors and deceased family members. We found that 31.4% of family caregivers complained of CTSP and 28.3% of CLBP. This is similar to findings from previous studies on the general population (CTSP: 4.7–46.7%; CLBP: 35.6–42.0%) (13,18,33,34).
The most important finding of this study is that the effect of cancer caregiving-related factors on CBP differs according to pain location. To reduce CTSP, it is important to address subjective psychological stress in family caregivers. In particular, it has been reported that symptoms of depression have a negative effect on physical health conditions, such as body pain, in family caregivers of cancer patients (9). To reduce CLBP, it is important to consider caregiving services according to cancer severity of care recipients. Many therapeutic interventions report pain improvement after exercise intervention for CBP (35,36).
Our findings suggest that CTSP in family caregivers is likely to be affected by subjective stress from caregiving. For depression and insomnia in particular, the CLBP group scored close to the cutoff, but the CTSP group generally exceeded the cutoff score. As this study was cross-sectional, causality cannot be inferred. However, it is possible that subjective stresses from caregiving, such as depression and insomnia, tend to impose a mental burden that manifests as thoracic spine pain in family caregivers. Myofascial pain is a symptom of several psychological disorders and is related to stress (37). Previous reports have identified relationships between myofascial pain and psychosocial factors such as depression, anger, and alexithymia (38-41). Trigger points in the upper back (or the upper trapezius) can also cause myofascial pain (16,38,39,41,42).
CLBP may be associated with several cancer severity-related factors in care recipients, including a decrease in ECOG PS score and a short time from survey until death. Unlike CLBP, however, CTSP did not show a relationship with cancer severity-related factors in care recipients. We therefore suggest that providing caregiving for patients with greater cancer severity places a physical burden on the lower back. There are reports of a relationship between CLBP and physical burden of caregiving in family caregivers of non-cancer patients (7,18,43). Caregiving activities such as body repositioning contribute to CLBP and are related to the illness severity of care recipients (43). In one study, female caregivers of children with physical impairments also showed a decline in body function and a higher level of CLBP severity (7). Another study found that when non-caregivers maintained good body function, they had a higher proportion of CTSP, but the proportion of CLBP increased when their body function declined (44).
The second important finding of this study is that the association between HADS-D score and CTSP was stronger in the group with PI ≤ PPG than in the group with PI > PPG (higher odds ratio). The median score for back pain was 3, and the group with CTSP (PI ≤ PPG) had a score of 2, defined as mild pain (23). However, the HADS-D score for the groups with CTSP (PI ≤ PPG and PI > PPG) was extremely high (11.4 for both groups). Although we cannot assume causality, these results may indicate that the presence of depression can affect the development or alleviation of mild thoracic spine pain. However, we cannot determine from these data whether the pain is caused by depression or whether the pain is prolonged by depression (depression affects whether the PPG has been achieved) and thereby becomes chronic.
Compared with the group with CLBP (PI ≤ PPG), the care recipients of the group with CLBP (PI > PPG) had a higher ECOG PS score and a shorter time from survey until death. The percentage of CLBP improvement goals achieved was less than or equal to 50%, a low treatment effectiveness rate. This may be because of the high median pain score of 7. The achievement of PPGs in patients with cancer pain is usually linked to mild pain (20), and PI is also associated with a decline in body function (17).
This study had several limitations. First, it was cross-sectional so causation cannot be inferred. Second, the participants were family caregivers who visited a hospital as attendants of care recipients; they did not present at hospital with a chief complaint of CBP. The diagnosis of CBP was made from medical history. Further, the data may not completely reflect the fact that participants were the primary family caregivers of cancer patients. Third, more than half of family caregivers were studied when their care recipients were hospitalized. These participants were directly caregiving at home, but were also indirectly caregiving (e.g., when visiting their care recipients in hospital), which might have affected some of the results. Fourth, data on caregiver traits and the background details of depression/anxiety were not collected; such data may have influenced the study findings. Fifth, only a few previous studies have classified back pain location as thoracic spine or lower back in a single research project. Furthermore, this study did not include date on pain in the cervical region which has a high prevalence of pain. Finally, this was a single-center study and lacks generalizability, so larger-scale data are required to confirm the conclusions.
Our results suggest that the factors related to caregiving in cancer patients differ according to back pain location. To reduce CBP, it is important to address subjective psychological stress and physical burden with reference to back pain location.
Acknowledgments
We thank Melissa Leffler, MBA, and Diane Williams, PhD, from Edanz Group (https://en-author-services.edanzgroup.com/ac) for editing a draft of this manuscript.
Funding: This work was supported by an Imai Kimi Memorial Stress-Related Disease Research Grant Fund.
Footnote
Reporting Checklist: The authors have completed the SURGE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-803
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-803
Peer Review File: Available at http://dx.doi.org/10.21037/apm-20-803
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-803). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics committee of Kansai Medical University, Japan (No. 2015660) and informed consent was taken from all study participants. This study was registered with the University hospital Medical Information Network Clinical Trials Registry (approval number: UMIN000021639) on March 27, 2016.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kim Y, Carver CS, Shaffer KM, et al. Cancer caregiving predicts physical impairments: roles of earlier caregiving stress and being a spousal caregiver. Cancer 2015;121:302-10. [Crossref] [PubMed]
- Vitaliano PP, Zhang J, Scanlan JM. Is caregiving hazardous to one's physical health? A meta-analysis. Psychol Bull 2003;129:946-72. [Crossref] [PubMed]
- Center for Disease Control and Prevention (CDC). Disability and Health. Atlanta, GA: CDC, 2011. Available online: https://www.cdc.gov/ncbddd/disabilityandhealth/healthyliving.html. Accessed July 1, 2016.
- Anderson LA, Edwards VJ, Pearson WS, et al. Adult caregivers in the United States: characteristics and differences in well-being, by caregiver age and caregiving status. Prev Chronic Dis 2013;10:E135. [Crossref] [PubMed]
- Ji J, Zöller B, Sundquist K, et al. Increased risks of coronary heart disease and stroke among spousal caregivers of cancer patients. Circulation 2012;125:1742-7. [Crossref] [PubMed]
- Kim Y, Given BA. Quality of life of family caregivers of cancer survivors: across the trajectory of the illness. Cancer 2008;112:2556-68. [Crossref] [PubMed]
- Tong HC, Kandala G, Haig AJ, et al. Physical functioning in female caregivers of children with physical disabilities compared with female caregivers of children with a chronic medical condition. Arch Pediatr Adolesc Med 2002;156:1138-42. [Crossref] [PubMed]
- Cameron JI, Franche RL, Cheung AM, et al. Lifestyle interference and emotional distress in family caregivers of advanced cancer patients. Cancer 2002;94:521-7. [Crossref] [PubMed]
- Shaffer KM, Kim Y, Carver CS, et al. Depressive symptoms predict cancer caregivers' physical health decline. Cancer 2017;123:4277-85. [Crossref] [PubMed]
- Carter PA. Caregivers' descriptions of sleep changes and depressive symptoms. Oncol Nurs Forum 2002;29:1277-83. [Crossref] [PubMed]
- Marshall PWM, Schabrun S, Knox MF. Physical activity and the mediating effect of fear, depression, anxiety, and catastrophizing on pain related disability in people with chronic low back pain. PLoS One 2017;12:e0180788. [Crossref] [PubMed]
- Pinheiro MB, Ferreira ML, Refshauge K, et al. Symptoms of depression as a prognostic factor for low back pain: a systematic review. Spine J 2016;16:105-16. [Crossref] [PubMed]
- Murase K, Tabara Y, Ito H, et al. Knee Pain and Low Back Pain Additively Disturb Sleep in the General Population: A Cross-Sectional Analysis of the Nagahama Study. PLoS One 2015;10:e0140058. [Crossref] [PubMed]
- Elbinoune I, Amine B, Shyen S, et al. Chronic neck pain and anxiety-depression: prevalence and associated risk factors. Pan Afr Med J 2016;24:89. [Crossref] [PubMed]
- Liu F, Fang T, Zhou F, et al. Association of Depression/Anxiety Symptoms with Neck Pain: A Systematic Review and Meta-Analysis of Literature in China. Pain Res Manag 2018;2018:3259431. [Crossref] [PubMed]
- Meleger AL, Krivickas LS. Neck and back pain: musculoskeletal disorders. Neurol Clin 2007;25:419-38. [Crossref] [PubMed]
- Silva AG, Alvarelhão J, Queirós A, et al. Pain intensity is associated with self-reported disability for several domains of life in a sample of patients with musculoskeletal pain aged 50 or more. Disabil Health J 2013;6:369-76. [Crossref] [PubMed]
- Weiner DK, Haggerty CL, Kritchevsky SB, et al. How does low back pain impact physical function in independent, well-functioning older adults? Evidence from the Health ABC Cohort and implications for the future. Pain Med 2003;4:311-20. [Crossref] [PubMed]
- Dalal S, Hui D, Nguyen L, et al. Achievement of personalized pain goal in cancer patients referred to a Supportive Care Clinic at a comprehensive cancer center. Cancer 2012;118:3869-77. [Crossref] [PubMed]
- Arthur J, Tanco K, Park M, et al. Personalized pain goal as an outcome measure in routine cancer pain assessment. J Pain Symptom Manage 2018;56:80-7. [Crossref] [PubMed]
- Dworkin RH, Turk DC, Peirce-Sandner S, et al. Research design considerations for confirmatory chronic pain clinical trials: IMMPACT recommendations. Pain 2010;149:177-93. [Crossref] [PubMed]
- Caraceni A, Cherny N, Fainsinger R, et al. Pain measurement tools and methods in clinical research in palliative care: recommendations of an Expert Working Group of the European Association of Palliative Care. J Pain Symptom Manage 2002;23:239-55. [Crossref] [PubMed]
- Serlin RC, Mendoza TR, Nakamura Y, et al. When is cancer pain mild, moderate or severe? Grading pain severity by its interference with function. Pain 1995;61:277-84. [Crossref] [PubMed]
- Hawker GA, Mian S, Kendzerska T, et al. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken) 2011;63 Suppl 11:S240-52. [Crossref] [PubMed]
- Watanabe YS, Miura T, Okizaki A, et al. Comparison of Indicators for Achievement of Pain Control With a Personalized Pain Goal in a Comprehensive Cancer Center. J Pain Symptom Manage 2018;55:1159-64. [Crossref] [PubMed]
- Bjelland I, Dahl AA, Haug TT, et al. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002;52:69-77. [Crossref] [PubMed]
- Matsudaira T, Igarashi H, Kikuchi H, et al. Factor structure of the Hospital Anxiety and Depression Scale in Japanese psychiatric outpatient and student populations. Health Qual Life Outcomes 2009;7:42. [Crossref] [PubMed]
- Maltby KF, Sanderson CR, Lobb EA, et al. Sleep disturbances in caregivers of patients with advanced cancer: A systematic review. Palliat Support Care 2017;15:125-40. [Crossref] [PubMed]
- Carney S, Koetters T, Cho M, et al. Differences in sleep disturbance parameters between oncology outpatients and their family caregivers. J Clin Oncol 2011;29:1001-6. [Crossref] [PubMed]
- Schreiner AS, Morimoto T, Arai Y, et al. Assessing family caregiver's mental health using a statistically derived cut-off score for the Zarit Burden Interview. Aging Ment Health 2006;10:107-11. [Crossref] [PubMed]
- Arai Y, Kudo K, Hosokawa T, et al. Reliability and validity of the Japanese version of the Zarit Caregiver Burden interview. Psychiatry Clin Neurosci 1997;51:281-7. [Crossref] [PubMed]
- Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 1982;5:649-55. [Crossref] [PubMed]
- Hurwitz EL, Randhawa K, Yu H, et al. The Global Spine Care Initiative: a summary of the global burden of low back and neck pain studies. Eur Spine J 2018;27:796-801. [Crossref] [PubMed]
- Luime JJ, Koes BW, Hendriksen IJ, et al. Prevalence and incidence of shoulder pain in general population: a systematic review. Scand J Rheumatol 2004;33:73-81. [Crossref] [PubMed]
- Rainville J, Hartigan C, Martinez E, et al. Exercise as a treatment for chronic low back pain. Spine J 2004;4:106-15. [Crossref] [PubMed]
- Liddle SD, Gracey JH, Baxter GD. Advice for the management of low back pain: a systematic review of randomised controlled trials. Man Ther 2007;12:310-27. [Crossref] [PubMed]
- Rivers WE, Garrigues D, Graciosa J, et al. Signs and symptoms of myofascial pain: an international survey of pain management providers and proposed preliminary set of diagnostic criteria. Pain Med 2015;16:1794-805. [Crossref] [PubMed]
- Celik D, Kaya Mutlu E. The relationship between latent trigger points and depression levels in healthy subjects. Clin Rheumatol 2012;31:907-11. [Crossref] [PubMed]
- Muñoz-Muñoz S, Muñoz-García MT, Alburquerque-Sendín F, et al. Myofascial trigger points, pain, disability, and sleep quality in individuals with mechanical neck pain. J Manipulative Physiol Ther 2012;35:608-13. [Crossref] [PubMed]
- Castelli L, De Santis F, De Giorgi I, et al. Alexithymia, anger and psychological distress in patients with myofascial pain: a case-control study. Front Psychol 2013;4:490. [Crossref] [PubMed]
- Hasuo H, Kanbara K, Abe T, et al. Relationship between Alexithymia and latent trigger points in the upper Trapezius. Biopsychosoc Med 2017;11:31. [Crossref] [PubMed]
- Bron C, Dommerholt J, Stegenga B, et al. High prevalence of shoulder girdle muscles with myofascial trigger points in patients with shoulder pain. BMC Musculoskelet Disord 2011;12:139. [Crossref] [PubMed]
- Suzuki K, Tamakoshi K, Sakakibara H. Caregiving activities closely associated with the development of low-back pain among female family caregivers. J Clin Nurs 2016;25:2156-67. [Crossref] [PubMed]
- Hasuo H, Kanbara K, Abe T, et al. Factors Associated with the Efficacy of Trigger Point Injection in Advanced Cancer Patients. J Palliat Med 2017;20:1085-90. [Crossref] [PubMed]


