
Predictive value of ACEF score for clinical prognosis of elderly patients with ST-segment elevation myocardial infarction after percutaneous coronary intervention
Introduction
With the progression of social aging issue, the incidence rate of acute myocardial infarction in the elderly population (aged ≥75 years) has also been gradually increased. Previous studies (1) have demonstrated that patients aged ≥75 years might account for up to 1/3 of the acute coronary syndrome population. Reperfusion therapy can significantly reduce the mortality rate and improve clinical prognosis of patients diagnosed with ST-segment elevation myocardial infarction (STEMI).
Due to the updating advancement of medical instruments and the maturity of detection technology, the safety and effectiveness of direct percutaneous coronary intervention (PCI) have been steadily improved. However, how to choose a reasonable revascularization strategy for the elderly patients (aged ≥75 years) with acute STEMI is still controversial. Therefore, the risks and benefits of PCI must be evaluated before clinical decision-making, which is also known as the risk stratification analysis of the affected patients (2,3).
ACEF score (age, creatinine, and ejection fraction score) mainly consists of three categories of clinical data including age, creatinine and left ventricular ejection fraction (LVEF), which should be initially proposed and verified in patients before undergoing coronary artery bypass grafting (4). Subsequently, multiple clinical trials have indicated that the ACEF score is also applicable to PCI patients (5-7). Wykrzykowska et al. (8) have delivered ACEF score assessment to the patients undergoing PCI enrolled in the LEADERS trial and have suggested that ACEF score may be a simple risk stratification tool to predict the mortality rate and the risk of myocardial infarction in PCI patients. Nevertheless, whether ACEF score can be used to predict the cardiac death in Chinese patients aged ≥75 years diagnosed with acute STEMI at 1 month and 1 year after emergency PCI has been rarely reported.
To add evidence to this unresolved issue, 360 patients aged ≥75 years old with STEMI undergoing emergency PCI in the Department of Cardiology of Anhui Provincial Hospital from January 2013 to April 2018 were consecutively recruited to unravel the predictive value of ACEF score for the cardiac mortality at 1 month and 1 year follow-up after emergency PCI.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-591).
Methods
Study population
STEMI patients undergoing PCI in the Department of Cardiology of Anhui Provincial Hospital from January 2013 to April 2018 were consecutively recruited in this clinical trial. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by ethics committees of Anhui Provincial Hospital (No.: 2020-P-052) and informed consent was taken from all the patients.
Inclusion and exclusion criteria
Inclusion criteria: (I) symptoms of ischemic chest pain for at least 20 minutes suggestive of acute myocardial infarction; (II) ST-elevation of at least 0.1 mV in two contiguous limb leads OR ST elevation of at least 0.2 mV in two contiguous precordial leads; (III) an occluded infarct-related artery at the time of coronary angiography (TIMI Flow Grade 0 or 1) The diagnostic criterion of STEMI was established according to the first edition of Guidelines on the Diagnosis and Treatment of STEMI in China proposed in 2010 and Fourth universal definition of myocardial infarction (2018) (9). Direct PCI was also performed based on the Guidelines on the Diagnosis and Treatment of STEMI in China proposed in 2010. Exclusion criteria: Patients with angina pectoris and chest pain caused by other reasons, and those refuse, have contraindications and/or are not suitable for invasive PCI were eliminated from this clinical trial.
Examinations and parameters
All patients underwent ECG examination upon admission. Venous blood was collected to detect the glucose level, blood lipid, liver function, kidney function, myocardial enzyme, etc. All patients were immediately examined by echocardiography. Hypertension is defined as measuring blood pressure three times on different days without using anti-hypertensive drugs, with systolic blood pressure ≥140 mmHg (1 mmHg =0.133 kPa) and/or diastolic blood pressure ≥90 mmHg or with definite hypertension history. Hyperlipidemia is defined as total cholesterol (TC) >5.18 mmol/L or low-density lipoprotein cholesterol (LDL-C) >3.37 mmol/L or high-density lipoprotein cholesterol (HDL-C) <1.04 mmol/L or triglyceride (TG) >1.70 mmol/L, or has a history of hyperlipidemia and is receiving lipid-regulating drug therapy. Type 2 diabetes mellitus is defined by adopting the standards of the American Diabetes Association. Fasting blood glucose ≥7 mmol/L at 8 h after diet and/or blood glucose ≥11.1 mmol/L at 2 h after diet, or those with a definite history of type 2 diabetes. Definition of smoking: smokers who smoke more than 1 cigarette a day and continue smoking for longer than 1 year are considered as smokers. Anemia was defined as hemoglobin less than 12 g/dL for men or less than 11 g/dL for women. Cardiogenic shock refers to the clinical syndrome of insufficient perfusion of tissues and organs due to the obvious decrease of cardiac output. The main manifestations include: (I) persistent hypotension (systolic blood pressure <90 mmHg for more than 30 min); (II) there were signs of organ perfusion injury (at least one item): mental state change, skin dampness and coldness, oliguria and elevated serum lactic acid level. The glomerular filtration rate (EGFR) was estimated by the modified dietary adjustment formula for Chinese people: EGFR (mL/min/1.73m2) = 175 × (sCr) − 1.234 × (age) − 0.179 for adult males and 175 × (sCr) − 1.234 × (age) − 0.179 ×0.79 for females. Left ventricular ejection fraction was calculated as: M-mode echocardiography was performed at the mitral valve apex level on the long axis view of left heart, and ED and ES were measured respectively. EDV and ESV were obtained by the software of the instrument, and EF = (EDV-ESV)/EDV × 100%.
Coronary angiography
All patients were scheduled to receive coronary angiography. The severity of stenosis was measured according to the reference value of the proximal end of the stenosis relative to the normal lumen. One lesion is defined as a vessel lumen stenosis ≥50% in the left anterior descending branch, left circumflex branch and right coronary artery, two and three lesions are defined as 2 or 3 major vessel lumen stenosis ≥50%, respectively, and the left main lesion is defined as the left main lumen stenosis ≥50%.
As recommend by Guidelines on the Diagnosis and Treatment of STEMI in China (2010), PCI should be directly performed in patients with STEMI (including positive and posterior myocardial infarction) or with new or possible new left bundle branch block. The patients who were more than 75 years old, had cardiogenic shock less than 36 hours of onset, were suitable for vascular reconstruction and could be performed within 18 hours after the onset of shock, if the patient’s previous cardiac function is good, suitable for vascular reconstruction and agreed to interventional treatment, direct PCI can be considered. If the patient is 12–24 hours after onset and has the one of the following conditions or more, direct PCI is feasible: (I) severe heart failure; (II) hemodynamic or ECG instability; (III) evidence of persistent ischemia. The arterial approach included radial, femoral and brachial arteries. Direct PCI is not recommended for STEMI patients with stable hemodynamics and electrocardiographic stability and without obvious ischemic symptoms for more than 12 hours. All patients enrolled in this study underwent primary PCI treatment. Thrombus aspiration was not routinely performed during the operation, but thrombus aspiration was performed in patients with heavy thrombus load. Intra-aortic balloon pump (IABP) is used in patients with STEMI complicated with hypotension, low cardiac output and ineffective drug therapy. In this study, drug-eluting stents were used in emergency PCI operations. Complete revascularization was defined when no visually estimated stenosis ≥70% for the left main and no stenosis ≥50% for other major arteries and/or their major branches at discharge. 30.0% of STEMI patients underwent complete revascularization during hospitalization, while 8 patients (2.2%) had persistent ischemia after PCI due to cardiogenic shock or infarction related artery. During hospitalization, complete revascularization was performed by PCI again. Since all the patients in this study were STEMI patients aged 75 years and above, emergency CABG (coronary arty bypass grafting) had not been carried out in our hospital when we choose the emergency reperfusion strategy.
ACEF scoring analysis
The ACEF score was calculated according to the following formula: ACEF = age/left ventricular ejection fraction (%) + 1 (if creatinine was >2.0 mg/dL). All patients were divided into tertiles based on the ACEF score (1).
Primary and secondary endpoint events
The primary endpoint event was cardiac death at postoperative 1 month and 1 year. Secondary endpoint events included any target lesion revascularization, cardiac death, death from any cause, myocardial infarction, stent thrombosis, device success, and lesion success within 1 year after emergency PCI. All patients were followed up by outpatient, medical record or telephone call. The follow-up time was 31 months, 1 year or until the end-point event occurred.
Statistical analysis
SPSS 20.0 statistical software was used for data analysis (SPSS Inc., Chicago, IL, U.S.). The normally distributed measurement data were expressed as mean ± standard deviation (SD). Student t-test was employed for comparison between two groups. The counting data were expressed as the percentage (%) and chi-square test were adopted. The ROC curve was delineated to evaluate the ACEF scoring system to predict the postoperative 30-d and 1-year mortality rate. Cox regression model using univariate analysis was carried out. A P value of less than 0.05 was considered as statistical significance.
Results
Patient grouping
A total of 360 STEMI patients undergoing PCI in the Department of Cardiology of Anhui Provincial Hospital from January 2013 to April 2018 were consecutively recruited. Among them, there were 215 male and 145 females. According to the ACEF score upon admission, all patients were assigned into the low-to-intermediate risk group (n=80) and high-risk group (n=280). In the low-to-intermediate risk group, there were 53 male and 27 females, aged 78.76±3.36 years on average. In the high-risk group, 162 patients were male and 118 females with a mean age of 80.95±459 years old.
Baseline data
As illustrated in Table 1, the gender proportion, heart rate, medical history of hypertension, stroke, myocardial infarction, diabetes mellitus, atrial fibrillation, anemia and cardiogenic shock did not significantly differ between the low-to-intermediate risk and high-risk groups (all P>0.05). However, the mean age in the low-to-intermediate risk group was 78.76±3.36 years on average, significantly lower compared with 80.95±4.59 years in the high-risk group (P<0.001). The heart rate in the low-to-intermediate risk group was 71.69±15.45, remarkably less compared with 77.29±19.06 in the high-risk group (P=0.016). In addition, the LVEF in the low-to-intermediate risk group was measured as 59.84±22.22, significantly higher than 44.27±15.60 in the high-risk group (P<0.001). The eGFR also significantly differed between two groups (P=0.005).
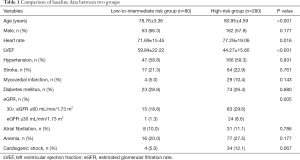
Full table
PCI outcomes
Among all PCI parameters, the complete revascularization rate in the low-to-intermediate risk group was calculated as 10.0%, which was significantly lower compared with 20.0% in the high-risk group (P=0.039). Except the this parameter, the left main lesion (8.5% vs. 6.7%, P=0.607), IABP (43.8% versus 38.6%, P=0.404), arterial puncture route (P=0.955), mean stent number (1.43±0.69 vs. 1.48±0.80, P=0.588) and mean stent length (41.80±22.63 vs. 40.31±24.95, P=0.633) did not significantly differ between the low-to-intermediate risk group and high-risk group, as illustrated in Table 2.
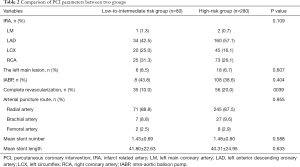
Full table
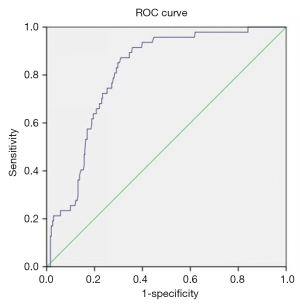
ROC curve analysis
As demonstrated in Figure 1, the area under the ROC curve of the ACEF scoring system in predicting cardiac death at 1 month after PCI was calculated as 0.809. In addition, the sensitivity of the ACEF scoring system in predicting cardiac death at 1 month after PCI was 86.3% and the specificity of the ACEF scoring system in predicting cardiac death at 1 month after PCI was assessed as 75.4%.
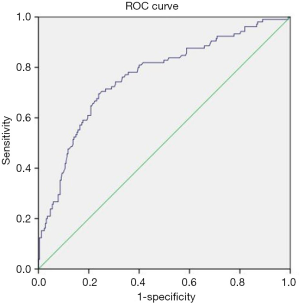
Moreover, the area under the ROC curve of the ACEF scoring system in predicting cardiac death at 1 year after PCI was calculated as 0.763. In addition, the sensitivity of the ACEF scoring system in predicting cardiac death at 1 year after PCI was 81.9% and the specificity of the ACEF scoring system in predicting cardiac death at 1 year after PCI was assessed as 70.7%, as illustrated in Figure 2.
Discussion
Considering the rapidly expanding surgical indications for PCI, clinical complexity and the concomitant increasing age of patients undergoing these procedures, risk assessment in terms of the overall rate of major adverse cardiovascular events, especially the mortality rate has become an extremely necessary aspect of clinical decision making in clinical practice. Multiple risk-assessment models such as EUROScore, have been established for patients scheduled to undergo surgery, which has been increasingly applied in the evaluation of patients undergoing PCI, particularly when decisions are required in terms of the appropriateness of surgical versus percutaneous revascularization in patients with extensive coronary artery diseases complicated with multiple diseases. Some of these risk scores, such as Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery (SYNTAX), possess excellent prognostic value (3,8,10,11), whereas SYNTAX is merely dependent upon the anatomic information and solely indirectly integrate clinical features. The elderly patients and those suffer from renal insufficiency are more likely to have more calcified vessels and more diffuse diseases. A majority of these surgical risk models integrate excessive variables, probably leading to a higher risk of the inaccuracies and over-fitting. Moreover, certain models incorporate patient characteristics which might impart a high risk to surgically treated patients alone, but not necessarily to those patients receiving PCI. The ACEF score is simple and convenient to calculate, which consists of three vital parameters including age, creatinine and LVEF (12). Consequently, the ACEF score is highly applicable to patients undergoing PCI.
Kalaycı et al. (13) applied the improved ACEF scoring system to evaluate STEMI patients. The score can predict the morbidity and mortality rate of heart disease patients within postoperative 1 year. Pyxaras et al. (7) have demonstrated that ACEF score can predict major adverse cardiovascular events in patients with severe coronary artery calcification after rotational abrasion and stent implantation within one year. However, researches by Di Serafino et al. (6) confirm that ACEF score is also applicable to PCI with chronic total coronary occlusion. Dziewierz et al. (14) have demonstrated that ACEF score can not only predict the mortality rate of patients with acute coronary syndrome, but also predict serious adverse events including hemorrhage.
In the present investigation, the application value of ACEF score in predicting the clinical prognosis of elderly STEMI patients after undergoing PCI was evaluated. The ROC curve analysis demonstrates that the ACEF score could effectively distinguish the short-term mortality rate of 360 enrolled aged patients with STEMI and have predictive value, which was consistent with previous findings. Nevertheless, Ye et al. (15) have obtained different outcomes that the ACEF score yields low predictive value in 104 STEMI patients. The discrepancy occurs probably due to the following aspects: First, the prognostic value of age was not observed. Second, the creatinine level does not accurately reflect the true level of renal function in elderly patients due to age, body mass index and other reasons. Third, the general situation of elderly STEMI patients who can undergo PCI is acceptable, and certain selection deviation may be induced, which cannot fully represent the elderly STEMI patients as a specific group.
There were still some limitations in this study. The sample size is relatively small, the follow-up time is 1 year, and all patients are recruited from a single center. It is necessary to further expand the sample size, prolong the follow-up duration to further consolidate the preliminary conclusion.
Conclusions
ACEF value upon admission can predict the cardiac death rate at 1 month and 1 year after emergency PCI in STEMI patients aged ≥75 years old.
Acknowledgments
We are grateful to Yiyuan Zhang and Lijun Jia for their outstanding effort at data collection.
Funding: The project was supported by the Open Research Fund of Anhui Institute of Cardiovascular Diseases (KF2018007) and the Scientific and Technological Project of Anhui Province (Grant No. 1604a0802074) and “Borrow to transfer to supplement” project of Hefei independent innovation policy (Grant No. J2019Y02)
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-591
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-591
Peer Review File: Available at http://dx.doi.org/10.21037/apm-20-591
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-591). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by ethics committees of Anhui Provincial Hospital (No.: 2020-P-052) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Alnasser SM, Huang W, Gore JM, et al. Late Consequences of Acute Coronary Syndromes: Global Registry of Acute Coronary Events (GRACE) Follow-up. Am J Med 2015;128:766-75. [Crossref] [PubMed]
- Subherwal S, Bach RG, Chen AY, et al. Baseline risk of major bleeding in non-ST-segment-elevation myocardial infarction: the CRUSADE (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA Guidelines) Bleeding Score. Circulation 2009;119:1873-82. [Crossref] [PubMed]
- Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 2009;360:961-72. [Crossref] [PubMed]
- Sullivan PG, Wallach JD, Ioannidis JP. Meta-Analysis Comparing Established Risk Prediction Models (EuroSCORE II, STS Score, and ACEF Score) for Perioperative Mortality During Cardiac Surgery. Am J Cardiol 2016;118:1574-82. [Crossref] [PubMed]
- Lee JH, Bae MH, Yang DH, et al. Prognostic value of the age, creatinine, and ejection fraction score for 1-year mortality in 30-day survivors who underwent percutaneous coronary intervention after acute myocardial infarction. Am J Cardiol 2015;115:1167-73. [Crossref] [PubMed]
- Di Serafino L, Borgia F, Maeremans J, et al. The age, creatinine, and ejection fraction score to risk stratify patients who underwent percutaneous coronary intervention of coronary chronic total occlusion. Am J Cardiol 2014;114:1158-64. [Crossref] [PubMed]
- Pyxaras SA, Mangiacapra F, Wijns W, et al. ACEF and clinical SYNTAX score in the risk stratification of patients with heavily calcified coronary stenosis undergoing rotational atherectomy with stent implantation. Catheter Cardiovasc Interv 2014;83:1067-73. [Crossref] [PubMed]
- Wykrzykowska JJ, Garg S, Onuma Y, et al. Value of age, creatinine, and ejection fraction (ACEF score) in assessing risk in patients undergoing percutaneous coronary interventions in the 'All-Comers' LEADERS trial. Circ Cardiovasc Interv 2011;4:47-56. [Crossref] [PubMed]
- Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction (2018). J Am Coll Cardiol 2018;72:2231-64. [Crossref] [PubMed]
- Capodanno D, Capranzano P, Di Salvo ME, et al. Usefulness of SYNTAX score to select patients with left main coronary artery disease to be treated with coronary artery bypass graft. JACC Cardiovasc Interv 2009;2:731-8. [Crossref] [PubMed]
- Capodanno D, Di Salvo ME, Cincotta G, et al. Usefulness of the SYNTAX score for predicting clinical outcome after percutaneous coronary intervention of unprotected left main coronary artery disease. Circ Cardiovasc Interv 2009;2:302-8. [Crossref] [PubMed]
- Ranucci M, Castelvecchio S, Menicanti L, et al. Risk of assessing mortality risk in elective cardiac operations: age, creatinine, ejection fraction, and the law of parsimony. Circulation 2009;119:3053-61. [Crossref] [PubMed]
- Kalaycı A, Oduncu V, Geçmen Ç, et al. A simple risk score in acute ST-elevation myocardial infarction: Modified ACEF(age, creatinine, and ejection fraction) score. Turk J Med Sci 2016;46:1688-93. [Crossref] [PubMed]
- Dziewierz A, Siudak Z, Rakowski T, et al. The ACEF (age, creatinine, ejection fraction) score predicts ischemic and bleeding outcomes of patients with acute coronary syndromes treated conservatively. Postepy Kardiol Interwencyjnej 2017;13:160-4. [Crossref] [PubMed]
- Ye SD, Li L, Sun ZW, et al. Role of ACEF score in assessment of primary PCI for ≥75 years old STEMI patients. Chin J Geriatr Heart Brain Vessel Dis 2017;19:1260-3.


