
Evaluation of maternal and fetal outcomes in pregnancy complicated with pulmonary arterial hypertension
Introduction
Pulmonary hypertension (PH) is a common condition characterized by several disorders from our bodies, including left heart disease, lung disease and chronic thromboembolic disease. PH occurs primarily because a majority of the minute arteries located within the lung becomes so narrow in diameter that they subsequently enhance the resistance towards the blood flow passing through the bilateral lungs (1,2). To counteract the elevated resistance, the blood pressure in the pulmonary artery and the right ventricle of the heart increases to pump the blood from the heart into the pulmonary artery. Consequently, hypertension tends to injure the right ventricle.
Pulmonary arterial hypertension (PAH), one type of PH, comprise of a category of progressive disorders. It is characterized by hypertension in the pulmonary artery, which transfers the blood from the heart into the lung. PAH occurs when hypertension fails to completely counteract the increased resistance, leading to the insufficiency of the oxygen-containing blood flowing to the rest parts of our bodies. PAH can acutely attack pregnant women, which is accompanied by a sudden onset of syncope, chest pain, or dyspnea. Signs and symptoms of PAH include dyspnea, fainting, dizziness, chest pain, and limb edema, etc. Since the symptoms and signs of PAH are similar to those of chronic obstructive pulmonary disease, a specific and accurate diagnosis should be delivered before any treatments and interventions (3).
For patients with pre-existing PAH or suffering from PAH during pregnancy, abortion remains to be the most recommendatory management. The mortality rate of PAH during pregnancy has been declined dramatically due to medical developments and advancements. However, PAH remains to be a severe issue in the postpartum period. Therefore, we are aimed to investigate the relations between PAH and pregnancy to precisely monitor the health conditions of pregnant women.
In the clinical trial, 59 pregnant women who were complicated with PAH undergoing termination of pregnancy were enrolled in this study. They were divided into mild, moderate and severe groups according to the severity of PAH. Multiple parameters were comprehensively monitored and analyzed, including age, gestational week, NYHA cardiac functional classification, UCG, blood test, pregnancy complications, pulmonary arterial systolic pressure, and maternal and fetal outcomes. We successfully evaluated the associations between these parameters and the maternal and fetal outcomes for pregnancy. We present the following article in accordance with the STROBE Reporting Checklist (available at http://dx.doi.org/10.21037/apm-20-551).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of Peking Union Medical College Hospital (No. s-k 1334). Written informed consent was obtained from all individual participants included in the study.
Data collection
A total of 59 pregnant women with PAH who were admitted to Peking Union Medical College Hospital from Jan. 2000 to Dec. 2018 were recruited in this study. Multiple parameters, including age, gestational week, NYHA cardiac functional classification, ultrasonic cardiogram UCG, blood test, pregnancy complications, pulmonary arterial systolic pressure and maternal and fetal outcomes, were comprehensively detected and analyzed.
Alternative primary diseases
The primary diseases which the 59 patients had were classified as lupus nephritis (n=6), congenital heart disease (n=19), systemic scleroderma (n=1), bilateral renal leiomyoma (n=1), gestational diabetes mellitus (n=3), heart failure (n=5), Sjogren’s syndrome (n=1), hyperthyroidism (n=1), hypothyroidism (n=2), hypertrophic cardiomyopathy (n=1) and rheumatic heart disease (n=4).
Diagnostic and inclusion criteria
PAH was defined with a mean PAH ≥25 mmHg in reference with a normal pulmonary capillary wedge pressure (≤15 mmHg). Inclusion criteria: (I) patients with PAH ≥25 mmHg on average; (II) patients with complete medical record; and (III) patients who received UCG monitoring.
Classification of PAH severity
The pulmonary arterial systolic pressure was assessed by UCG monitoring. All patients were divided into mild PAH group (30–49 mmHg), moderate PAH group (50–79 mmHg) and severe PAH group (>79 mmHg), respectively.
Statistical analysis
SPSS statistical software (version 22.0) was used for data analyses (SPSS Inc., Chicago, IL, USA). Enumeration data were expressed as percentage. Measurement data were expressed as means ± standard deviation (SD). Comparative analysis was carried out by using chi-square test and t-test. P<0.05 was considered as statistical significance.
Results
Baseline data
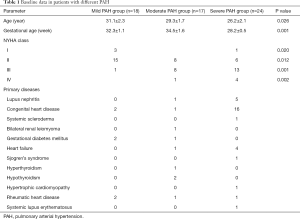
A total of 59 pregnant women who complicated with PAH were enrolled in the present study. Their ages were ranging from 18 to 41 years old, with an average of 27.7±1.3 years. The gestational ages were ranged from 10 to 40 weeks, with an average of 32.5±2.2 weeks. Among them, 18 pregnant women were classified into the mild PAH group (32.2%), 17 were assigned into the moderate PAH group (28.8%), and 24 were allocated into the severe PAH group (39%), respectively. Based on the New York Heart Association (NYHA) cardiac functional classification, 1 patient was classified as grade I, 27 were classified as grade II, 24 were classified as grade III, and 5 were classified as grade IV (Table 1).
Full table
Primary diseases
The 59 patients were diagnosed with multiple categories of primary diseases. There were lupus nephritis (n=6, 10.2%), congenital heart disease (n=19, 32.2%), systemic scleroderma (n=1, 1.7%), bilateral renal leiomyoma (n=1, 1.7%), gestational diabetes mellitus (n=3, 5.1%), heart failure (n=5, 8.5%), Sjogren’s syndrome (n=1, 1.7%), hyperthyroidism (n=1, 1.7%), hypothyroidism (n=2, 3.4%), hypertrophic cardiomyopathy (n=1, 1.7%), rheumatic heart disease (n=4, 6.8%) and systemic lupus erythematosus (n=1, 1.7%) (Table 1).
Routine blood test
Activated partial thromboplastin time (APTT) was detected as 150 s postoperatively in 1 patient, who died subsequently. Another patient with a postoperative level of brain natriuretic peptide of 3,500 pg/mL also died. In most alive patients, the levels of urine protein, brain natriuretic peptide, blood platelet, anti-SSA antibody, hemoglobin level, white blood cell count, creatinine level and erythrocyte sedimentation rate were restored or almost restored to normal range.
Perioperative complications
In the severe PAH group, the patients had some disease complications. One patient had heart failure complicated with pericardial effusion, one had left and right atrial enlargement, 10 had right atrial enlargement complicated with tricuspid regurgitation, 11 had right atrial enlargement, and one patient had aortic stenosis complicated with tricuspid regurgitation. In the moderate PAH group, two patients had mild tricuspid regurgitation, two patients had left atrial enlargement and right ventricular enlargement, and six had left atrial enlargement complicated with tricuspid regurgitation. In the mild PAH group, one patient had an atrial defect, one had left atrial enlargement complicated with mild tricuspid regurgitation, four had tricuspid regurgitation, and one had right atrial enlargement. The rate of premature delivery in the severe PAH group was 12.5%, significantly higher than 0% in the moderate PAH group and 5.3% in the mild PAH group.
Surgical approach
Among 59 pregnant women, 55 of them underwent cesarean section (93.2%), with 52 under general anesthesia, one under epidural anesthesia and one lumbar anesthesia, respectively. The remaining 4 patients underwent an abortion (6.8%). In terms of extracorporeal membrane oxygenation (ECMO), two patients received postoperative ECMO, and one was treated with ECMO both intraoperatively and postoperatively, whereas all these three mothers and infants died postoperatively.
Maternal and neonatal outcomes
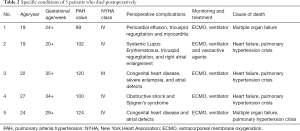
Among 59 patients, five mothers and their infants died of multiple organ failure (n=2) and severe asphyxia (n=3). Among them, one patient was diagnosed with myocarditis, one patient had systemic lupus erythematosus, one patient had primary dryness syndrome, and two patients had congenital heart disease complicated with ventricular defects (Table 2). Furthermore, 10 infants died due to various causes, including severe asphyxia (n=6), severe asphyxia (n=3) and premature delivery (n=1). The overall mortality rate for all mothers was 7.2%, who were all diagnosed with severe PAH (range, 98–160 mmHg). The mortality rate in patients with severe PAH was 20.8%, which was significantly higher than 0% in both the moderate and mild PAH groups (both P<0.05). In terms of the infants, the mortality rate in the severe PAH group was 33.3%, which was significantly higher in comparison with 5.9% in the moderate PAH group and 5.3% in the mild PAH group (both P<0.05).
Full table
Discussion
PAH is a category of disease characterized by progressive recombination of the distal pulmonary arteries. It will lead to the elevation of pulmonary vascular resistance and right heart failure, exercise intolerance and progressive dyspnea, right ventricular failure or even death. It has been estimated that the median survival time of patients with PAH is roughly 2.8 years (1), which has been relatively increased by effective interventions and therapies, such as the utilization of epoprostenol or combinational therapies (2). In spite of these advancements, the mortality rate of patients with PAH in the first year is still approximately 13–18% among different investigations (1-3). In the present study, the overall mortality rate of PAH pregnancies was approximately 8.5%, which is slightly lower than the data in previous findings, probably due to the limited sample size. However, the mortality rate in the severe PAH group was 20.8%, which was much higher than that in previous study, indicating that severe PAH probably increased the postoperative mortality rate.
The pathophysiological mechanism of PAH is considered as a complicated functional disorder of the endothelial cells, which eventually leads to the remodeling of the pulmonary arterial walls. It increases the vasoconstriction and interrupts the procedures of vasodilation. Vascular injuries are possibly correlated with or idiopathic to the alternative types of illnesses. In the healthy population, the average PAH is measured between 15–20 and 8–12 mmHg for the pulmonary arterial wedge pressure. However, the patients with PAH have an APH exceeding 25 mmHg on average, and the pulmonary capillary wedge pressure is measured <15 mmHg. Clark et al. (4) have analyzed the pulmonary artery catheterization at 36–38 weeks and repeatedly conducted the catheterization at 11–13 weeks postpartum in 10 pregnant women. They identified no significant changes in terms of the central venous pressure and pulmonary capillary wedge pressure (4).
It has been widely recognized that the pregnant women who are diagnosed with PAH should be contraindicated due to the relatively high mortality rate (5-7). During the gestational period, the blood volume of the pregnant women can be increased by 30–50% and the cardiac output can be elevated even by 50% because of a decline in the systemic vascular resistance (8). In pregnant women with PAH, the enlarged blood volume and elevated cardiac output can cause life-threatening damage due to the right heart failure (9). Moreover, during the labor process, each movement of the contraction can increase approximately 300–500 mL of the blood volume and simultaneously lead to a 50% elevation in the cardiac output. Even after the delivery, the blood volume of the pregnant woman will be further increased by roughly 500 mL. The cardiac output is maintained at a relatively high level within 48 h after delivery.
Consequently, the mortality rate of pregnant women with severe PAH remains relatively high. In this clinical trial, five mothers with severe PAH died postoperatively. Among them, 4 patients died within 24 h after the delivery due to PH crisis and heart failure (10). The remaining one patient died after 7-d ICU stay due to multiple organ failure. These outcomes suggest that extensive and intensive monitoring and attentions should be paid to those with severe PAH within 48 h after the delivery, and effective measures and interventions should be carried out to reduce the postoperative mortality rate as possible.
The timing and mode of delivery play vital roles in the maternal and neonatal outcomes. However, there is no consensus on the optimal mode of delivery for pregnant women with PAH (11). Vaginal delivery may be preferred because of the reduction of the risk of general anesthesia. If the vaginal route was chosen for delivery, it must be performed under intensive care. However, prolonged second-phase delivery, uncontrolled risk of vaginal hemorrhage as well as the hemodynamic disturbances caused by pushing down and contractions during vaginal delivery can be properly avoided by using cesarean section (12). Consequently, a majority of pregnant women with PAH who were enrolled in this investigation underwent a cesarean section, which yielded no death case in the mild and moderate PAH groups, suggesting that cesarean section might be a much safer choice for pregnant women with mild and moderate degrees of PAH.
A multidisciplinary team should be established to carry out the postoperative follow-up of pregnant women with PAH (13). The team should consist of anesthesiologist, obstetrician, neonatologist cardiologist, and hematologist for the effective and safe management of the patients. Hospital stay is essential during the second trimester because of the high risk of blood complications and preterm delivery (14). They should receive echocardiography and the inferior vena cava compression. Oxygen treatment should be delivered to keep the PaO2 above the level of 70 mmHg. Pulmonary arterial hypoxemia is a serious hemodynamic complication, which should be properly handled. Furosemide, combined with torsemide, can be administered in the treatment of right heart failure. Low molecular-weight heparin prophylaxis can be considered to lower the risk of thromboembolism (15).
However, several limitations should be noted in this clinical trial. First, the sample size is limited, and the conclusion remains to be validated by subsequent investigations with larger sample size. Moreover, this is a retrospective analysis, and the obtained outcomes should be assessed in a prospective investigation. Finally, the long-term follow-up is absence, and the conclusion remains to be confirmed by long-term observation.
Conclusions
In conclusion, the blood parameters, PAH, and NYHA cardiac functional classification grade were significantly changed before and after surgery. We found that the severity of PAH was a major factor of maternal and fetal outcomes. Strengthening the nursing care for pregnant women with PAH is of great clinical significance.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE Reporting Checklist. Available at http://dx.doi.org/10.21037/apm-20-551
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-551
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-551). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of Peking Union Medical College Hospital (No. s-k 1334). Written informed consent was obtained from all individual participants included in the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, et al. 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J 2018;39:3165-241. [Crossref] [PubMed]
- Hemnes AR, Kiely DG, Cockrill BA, et al. Statement on pregnancy in pulmonary hypertension from the Pulmonary Vascular Research Institute. Pulm Circ 2015;5:435-65. [Crossref] [PubMed]
- Chin KM, Rubin LJ. Pulmonary arterial hypertension. J Am Coll Cardiol 2008;51:1527-38. [Crossref] [PubMed]
- Clark SL, Cotton DB, Lee W, et al. Central hemodynamic assessment of normal term pregnancy. Am J Obstet Gynecol 1989;161:1439-42. [Crossref] [PubMed]
- Galiè N, Hoeper MM, Humbert M, et al. Guidelines for the diagnosis and treatment of pulmonary hypertension: the Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS), endorsed by the International Society of Heart and Lung Transplantation (ISHLT). Eur Heart J 2009;30:2493-537. [Crossref] [PubMed]
- Olsson KM, Jais X. Birth control and pregnancy management in pulmonary hypertension. Semin Respir Crit Care Med 2013;34:681-8. [Crossref] [PubMed]
- Grünig E, Benjamin N, Krüger U, et al. General measures and supportive therapy for pulmonary arterial hypertension: Updated recommendations from the Cologne Consensus Conference 2018. Int J Cardiol 2018;272S:30-6. [Crossref] [PubMed]
- Bendayan D, Hod M, Oron G, et al. Pregnancy outcome in patients with pulmonary arterial hypertension receiving prostacyclin therapy. Obstet Gynecol 2005;106:1206-10. [Crossref] [PubMed]
- Kiely DG, Condliffe R, Webster V, et al. Improved survival in pregnancy and pulmonary hypertension using a multiprofessional approach. BJOG 2010;117:565-74. [Crossref] [PubMed]
- Hoeper MM, Bogaard HJ, Condliffe R, et al. Definitions and diagnosis of pulmonary hypertension. J Am Coll Cardiol 2013;62:D42-50. [Crossref] [PubMed]
- Galiè N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J 2016;37:67-119. [Crossref] [PubMed]
- Lopes AA, Barst RJ, Haworth SG, et al. Repair of congenital heart disease with associated pulmonary hypertension in children: what are the minimal investigative procedures? Consensus statement from the Congenital Heart Disease and Pediatric Task Forces, Pulmonary Vascular Research Institute (PVRI). Pulm Circ 2014;4:330-41. [Crossref] [PubMed]
- Manes A, Palazzini M, Leci E, et al. Current era survival of patients with pulmonary arterial hypertension associated with congenital heart disease: a comparison between clinical subgroups. Eur Heart J 2014;35:716-24. [Crossref] [PubMed]
- Seckel MA, Gray C, Farraj MB, et al. Undiagnosed pulmonary arterial hypertension at 33 weeks' gestation: a case report. Crit Care Nurse 2010;30:45-52. [Crossref] [PubMed]
- Kaemmerer H, Apitz C, Brockmeier K, et al. Pulmonary hypertension in adults with congenital heart disease: Updated recommendations from the Cologne Consensus Conference 2018. Int J Cardiol 2018;272S:79-88. [Crossref] [PubMed]


