
The effect of a novel slow-flow irrigation drainage tube on anastomotic leakage and empyema after the resection of esophageal or gastroesophageal junction cancer
Introduction
Surgical resection is the preferred treatment of the esophageal or gastroesophageal junction (GEJ) cancer in the limited stage (1). Despite the recent improvement in surgical technique, esophagogastric anastomotic leakage is still the most severe postoperative complication. The incidence of intrathoracic anastomotic leakage after esophagectomy ranges from 4% to 44%, and the mortality rate following anastomotic leakage reaches approximately 40% (2). Due to the fact that anastomotic leakage leads to a series of complications, such as severe lung inflammation, empyema, respiratory failure, heart failure, etc., patients' postoperative recovery, subsequent treatment and prognosis would be severely affected with the occurrence and healing of anastomotic leakage (3). Therefore, it is of great clinical value to improve the treatment of the postoperative anastomotic leakage.
Anastomotic leakage could be classified, according to the time of postoperative onset, as early (1–3 days), intermediate (3–14 days), or late (more than 14 days) stage. Currently, the Esophageal Complications Consensus Group (ECCG) has proposed a definition and classification of postoperative complications following esophageal resection, including anastomotic leakage. The anastomotic leakage were grouped into type I, II and III, according to the treatment (4). This study focused on type II anastomotic leakage to figure out the potential improvement of therapy. The treatment of anastomotic leakage depends on the location of the anastomosis, the extent of the leakage and the physical condition of the patients (2). There is no denying that maintaining smooth pleural drainage with pleural drainage tube is the most critical treatment for postoperative anastomotic leakage, besides antibiotics, nutrition support, reoperation, etc. (5). However, the drainage range of traditional pleural drainage tube is limited when the location of peri-anastomotic empyema cavity is too deep to approach. Therefore, the natural drainage with traditional pleural drainage tube alone would be inadequate for the treatment (6). Essentially, the fact that pus accumulates around the fistula, even forms empyema cavities, would directly interfere the healing of the fistula. To solve this problem, Hooper et al. verified that pleural irrigation with normal saline was a useful therapy for empyema (7), which guided us to investigate the value of irrigation in the improvement for the drainage of peri-anastomotic empyema cavity.
Based on our 8-year experience in the application of the slow-flow irrigation drainage tube, we report the application procedure and detect its efficacy and safety in a retrospective study. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-1401).
Methods
Patient data
In this study, we distributed the patients, with postoperative anastomotic leakage, into slow-flow irrigation drainage tube group (I+) or traditional drainage (non-irrigation) tube group (I−), in order to evaluate the effect and safety of the application of slow-flow irrigation drainage tube. From January 2012 to June 2019, all the patients who underwent radical resection for esophageal or GEJ cancer were reviewed. The patients who suffered acute respiratory failure or other severe complication which lead to death in short term (within 2 weeks), with no chance of irrigation, were excluded in this study. Patients with cervical anastomotic leakage were also excluded. In addition, the patients whose postoperative hospital stay were less than 1 month or more than 4 months were excluded. Eventually, totally 42 patients, who suffered postoperative anastomotic leakage with refractory empyema, were enrolled in this study. The operative approach includes left thoracic esophagectomy, right thoracic-abdominal esophagectomy and abdominal gastroesophagectomy. All the patients received digestive tractreconstruction with esophagogastric anastomat. The diagnosis of anastomotic leakage was confirmed with at least one of the following three ways: endoscopy, oral methylene blue being drained through the pleural drainage tube, or oral contrast agent flowing out of the digestive tract detected with CT.
All the patients received the nutritional support with nasal feeding. Irrigation in (I+) group was carried out at least two weeks after primary surgery, for fear of pus would be dispersed in the thorax by irrigation without confinement. In (I+) group, the slow-flow irrigation drainage tube was placed along the primary pleural drainage tube into the empyema cavity. Eleven patients received the first generation slow-flow irrigation drainage tube, and 9 patients received the second one according to time order. And traditional pleural drainage tube was used in (I−) group. No patient received other intervention, including stent, endo-sponge, primary repair, etc. The healing of anastomotic leakage of each patient was confirmed with endoscopy. Thereafter, the drainage tube was drawn out for 2 centimeters per day until it was totally moved out. All the patients were discharged with semi-liquid diet and removal of drainage tube. Reoperation for repairing the fistula was not conducted for the reason that the local chronic inflammatory was prone to interfere the recovery of fistula.
A total 42 patients’ clinicopathological data was collected in details, including sex, age, tumor pathology, tumor size, tumor depth, lymph node metastasis, operative approach, neoadjuvant therapy, tumor location, tumor-node-metastasis (TNM) stage (according to American Joint Committee on Cancer, eighth edition) (8). The detailed clinicopathological and hospitalization information of each patient was available in the database of the department (Table S1). The written informed consent was obtained from each patient. This study conformed to the provisions of the Declaration of Helsinki (as revised in 2013). This study was approved by the ethics committee on human research of Zhongshan Hospital, Fudan University.
The structure of slow-flow irrigation drainage tube
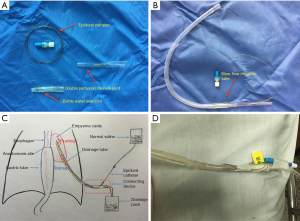
The first generation slow-flow irrigation drainage tube is made up of an anaesthesia epidural catheter, a double perfusion cannula joint, a water-sealed drainage bottle joint and a traditional pleural drainage tube (Figure 1A). The structure of the slow-flow irrigation drainage tube after assemble is shown in Figure 1B. A little pinhole is made in the double perfusion cannula joint, through which the epidural catheter is placed into the empyema cavity directly along with the primary pleural drainage tube and saline solution is irrigated through the epidural catheter into the empyema cavity at bedside (Figure 1C). However, the first generation slow-flow irrigation drainage tube showed some inevitable disadvantage, such as fluid leakage from the pinhole, trouble in fixation and limited irrigating speed, since the irrigation drainage tube was temporarily assembled (Figure 1D). Thus, we got down to designing the second generation slow-flow irrigation drainage tube, which would serve the irrigation and drainage function as an all-in-one device.
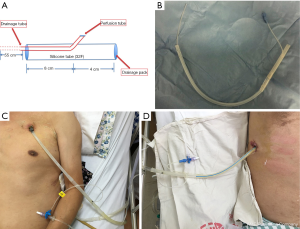
In the second generation slow-flow irrigation drainage tube, multiple components were integrated as an entirety to solve the above disadvantages. Using silica gel materials, a second-generation tube was divided into two parts: the outer tube and the inner irrigation tube. The special joint design could adjust the irrigation tube depth in the empyema cavity and prevent fluid leakage with a silica gel spacer at the pinhole for inner irrigation tube to insert in (Figure 2A,B). This construction of the second-generation irrigation drainage tube could be well fixed outside the body (Figure 2C,D). Compared with epidural catheter, the diameter of the inner irrigation tube was widened significantly. This improvement could increase the irrigation speed, which offers multiple option for the irrigation volume and speed. We used traditional infusion pump to control the speed and volume. At early stage, the pus was relatively thick and hard to be drained. Then, we kept the irrigation at the largest speed and maintained the irrigation throughout the day. Once the drainage fluids become relative clean, we adjust the irrigation speed to 120–150 mL/h and reduce the irrigation volume to 1,000 mL/day.
The design of the second-generation irrigation drainage tube was awarded a national patent (No. ZL 201520007804.4) in 2015. The allocation sequence was generated by F Xu. J Gu enrolled the participants and C Lu assigned participants to interventions.
Statistical analysis
Statistical analysis was undertaken with SPSS software (version 17.0). Variables were compared the Student’s t-test, and chi-square test according to the type of variables. A two-sided P value less than 0.05 was considered statistically significant.
Results
General condition of the patients
Among the 42 patients enrolled in this study, there was a male predominance in the cohort of 32 men and 10 women. The average age of the total patients was 65±8 years. There was no significant difference in age (P=1.000) or gender (P=0.723) between (I+) group and (I−) group. The features of tumor pathology, including tumor histology, location, size, differentiation, invasion depth, lymph node metastasis, tumor stage were all similar between the two groups (Table 1). No patient suffered diabetes, chronic liver diseases, using of steroid or malnutrition.
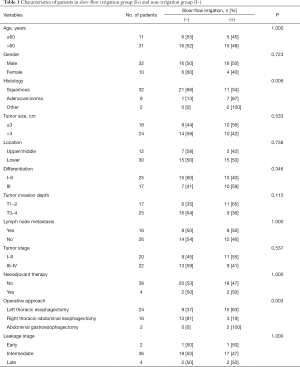
Full table
In histology, 32 cases of squamous cell carcinoma occupied a majority proportion, compared with 8 cases of adenocarcinoma, 1 case of stromal tumor and 1 case of squamous cell carcinomas mixed with small cell carcinoma. 2 patients undertook neoadjuvant chemotherapy or radio-chemotherapy in each group, respectively. The operative approach includes 24 cases of left thoracic esophagectomy, 16 cases of right thoracic-abdominal esophagectomy and 2 cases of abdominal gastroesophagectomy. There were significantly more instances of application of the left thoracic approach in (I+) group, more instances of application of the right thoracic-abdominal approach in (I−) group, and only 2 cases of abdominal approach in (I+) group (P=0.003). In addition, the leakage stage (early, intermediate, or late) was parallel between two groups (Table 1).
Management and outcome of anastomotic leakage
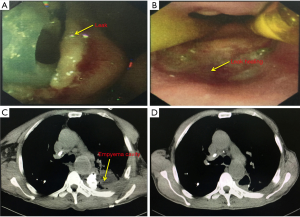
There were 22 patients in (I−) group and 20 patients in (I+) group. In the analysis of curative efficacy, we found that 1 patient in (I−) group suffered the postoperative bleeding drained from the tube, while none in (I+) group. Meanwhile, patients in (I−) group were more likely to encounter pulmonary complications (including pneumonia, hypoxemia, respiratory failure, etc.) (18 vs. 9, P=0.023), reoperation for bleeding or severe thorax infection (5 vs. 0, P=0.049), readmission into ICU (8 vs. 5, P=0.514) than the ones in (I+) group. These data indicated that the application of slow-flow irrigation-drainage tube had a significant advantage in the recovery period of anastomotic leakage, compared with traditional group (Table 2). With the application of slow-flow irrigation-drainage tube, the fistula was prone to be healed together with the elimination of pus cavity (Figure 3).
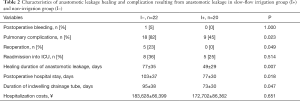
Full table
In the analysis of patients’ burden and life quality, we found that patients in (I−) group underwent longer healing duration of anastomotic leakage (77±35 vs. 49±29, P=0.007), longer postoperative hospital stay (103±37 vs. 77±30, P=0.018), and longer duration of indwelling drainage tube (95±38 vs. 73±30, P=0.047) than the ones in (I+) group. Meanwhile, the application of the novel slow-flow irrigation drainage tube caused no more economic losses at hospitalization cost. These results suggested that slow-flow irrigation-drainage tube would be an economical curative way for anastomotic leakage (Table 2).
Moreover, during the process of irrigation-drainage, only cough and reflux were observed in 3 patients. No other severe complication occurred during the irrigation in both groups.
Discussion
As one of the most severe complications following esophageal surgery, anastomotic leakage remains unavoidable during the clinical process. Up till now, there is no treatment standard for postoperative anastomotic leakage (2). We introduced our design of a type of slow-flow irrigation drainage tube, which facilitates the clean of empyema cavity and healing of the fistula.
Whether the past or present, smooth drainage is the most vital prerequisite of the treatment for anastomotic leakage (9). However, some empyema cavity in deep site is hard to be drained thoroughly through the traditional pleural drainage tube. Numerous surgeons have employed a nasogastric tube to reach the deep empyema cavity through the anastomotic defect, which served as an internal drainage system (10,11). This technique, on the other hand, also risks further injury of the anastomosis and prolongs the healing duration (5). Meanwhile, the location of empyema cavity might be so elusive that traditional drainage tube fails to approach, even if the tube placement is guided with CT, ultrasound, or endoscopy. Inspired by the idea that irrigation facilitates the rapid disinfection and closure of the empyema space by Nakamoto et al. (12), we attempted to ameliorate this system in the treatment of anastomotic leakage with peri-anastomotic empyema cavity.
We designed the first generation slow-flowing irrigation drainage tube by assembling an epidural catheter, a double cannula and a series of connective device (Figure 1A,B). The irrigation drainage tube got access to the deep abscess cavity along with the previous traditional drainage tube and effectively diluted the pus with irrigated normal saline. Hooper et al. proved that the patients receiving normal saline irrigation had a significantly greater reduction in pleural collection volume on CT compared to those receiving standard care and significantly fewer patients in the irrigation group were referred for surgery (7). Rosenfeldt et al. verified cyclical irrigation resulted in a shorter hospital stay and a shorter period of wound drainage than other methods for empyema and pneumonectomy space infection (13). We wondered whether irrigation through the slow-flowing irrigation drainage tube produced the similar effects.
In the clinical practice of irrigation drainage tube, the patients using the irrigation-drainage tube benefited from decreasing the rate of multiple complications secondary to anastomotic leakage, such as postoperative bleeding, pulmonary complications [including pneumonia, hypoxemia, respiratory failure, etc. (14)], reoperation for bleeding or severe thorax infection, compared with the patients using traditional drainage tube (Table 2). Meanwhile, the effective reduction of these complications accelerated the healing of anastomotic leakage, and shortened the duration of postoperative hospital stay and indwelling drainage tube (Table 2). These achievements were quite inspiring.
During the clinical practice, we also figured out some deficiencies in the structure of the first generation slow-flowing irrigation drainage tube, including fluid leak through the connective device, limitation in irrigating speed and block in the epidural catheter. To fix these problems, we altered the primary structure and design the second generation slow-flowing irrigation drainage tube. The new designed tube is an integrated and non-invasive device, which improves patient's quality of life and reduced nurses’ workload.
The solution chosen for irrigation in this study was normal saline. Other choice, such as antimicrobial, is also applicable through the slow-flowing irrigation drainage tube. Irrigation with arbekacin into the empyema cavity was proved to be an effective and safe way for treating MRSA following lung resection (15). Intrapleural vancomycin irrigation was reported effective and well tolerated in postpneumonectomy empyema (6). Hence, the fluid used for irrigation could be adjusted based on drug sensitivity test or experience. During the process of irrigation, only cough and reflux were observed in 3 patients and no severe complication occurred. Hence, our designed slow-flow irrigation drainage tube is an effective and safe way for the treatment of anastomotic leakage with peri-anastomotic empyema cavity.
However, there existed some limitations in our study. First, since it was a retrospective study, certain defects of this study were uncontrollable, including the exact proportion of the two groups, limited number of cases, nutritional status of the patient and the size of the fistula could not be matched precisely. Besides, the design of the irrigation drainage tube still need improvement in the course of clinical practice. Thus, in the future, we will carry out a prospective study in multicenter to analyse the value of slow-flow irrigation drainage tube in the treatment of anastomotic leakage with peri-anastomotic empyema.
Conclusions
The anastomotic leakage with peri-anastomotic empyema after esophagectomy remains an intractable problem for thoracic surgeons. We designed a slow-flow irrigation drainage tube, which is easily placed into the deep empyema cavity along the primary pleural drainage tube to drain and flush the thick pus. This curative method has been proved non-invasive, safe, and effective during the clinical practice, which is worthy of promotion and widen application in the treatment of empyema or deep localized infections. Given the small number of people in this study, additional prospective study is also required to furtherly investigate the virtue of slow-flow irrigation drainage and its extended application in deep infections in thorax.
Acknowledgments
We appreciated all the investigators who take part in this study. We are especially thankful to Mr. Xu for his help in design of this new type irrigation drainage tube.
Funding: We paid sincerely thanks for the support and funds, including the New Technique Project of Shanghai Science and Technology Commission (19441908800), the Youth Project of Zhongshan Hospital Foundation (2020ZSQN15), National Natural Science Foundation (81872291), the Industry-University-Research Project of Shanghai Science and Technology committee (19441908800) in the experiment materials, and the Outstanding Study Plan of Fudan University in the data analysis.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-1401
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-1401
Peer Review File: Available at http://dx.doi.org/10.21037/apm-20-1401
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-1401). CL has a patent a novel slow-flow irrigation drainage tube licensed to ZL 201520007804.4. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The written informed consent was obtained from each patient. This study was approved by the ethics committee of Zhongshan Hospital, Fudan University. According to the policy of ethical committee, the registration number is unfit to a retrospective study on a novel technology and material.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Klevebro F, Ekman S, Nilsson M. Current trends in multimodality treatment of esophageal and gastroesophageal junction cancer - Review article. Surg Oncol 2017;26:290-5. [Crossref] [PubMed]
- Hagens ERC, Anderegg MCJ, van Berge Henegouwen MI, et al. International Survey on the Management of Anastomotic Leakage After Esophageal Resection. Ann Thorac Surg 2018;106:1702-8. [Crossref] [PubMed]
- Markar S, Gronnier C, Duhamel A, et al. The Impact of Severe Anastomotic Leak on Long-term Survival and Cancer Recurrence After Surgical Resection for Esophageal Malignancy. Ann Surg 2015;262:972-80. [Crossref] [PubMed]
- Low DE, Alderson D, Cecconello I, et al. International Consensus on Standardization of Data Collection for Complications Associated With Esophagectomy: Esophagectomy Complications Consensus Group (ECCG). Ann Surg 2015;262:286-94. [Crossref] [PubMed]
- Mitchell JD. Anastomotic leak after esophagectomy. Thorac Surg Clin 2006;16:1-9. [Crossref] [PubMed]
- Torbic H, Glasser N, Rostas SE, et al. Intrapleural Antimicrobial Irrigation for Postpneumonectomy Empyema in Patients With Lung Cancer. J Pharm Pract 2015;28:469-72. [Crossref] [PubMed]
- Hooper CE, Edey AJ, Wallis A, et al. Pleural irrigation trial (PIT): a randomised controlled trial of pleural irrigation with normal saline versus standard care in patients with pleural infection. Eur Respir J 2015;46:456-63. [Crossref] [PubMed]
- Rice TW, Ishwaran H, Ferguson MK, et al. Cancer of the Esophagus and Esophagogastric Junction: An Eighth Edition Staging Primer. J Thorac Oncol 2017;12:36-42.
- Plum PS, Herbold T, Berlth F, et al. Outcome of Self-Expanding Metal Stents in the Treatment of Anastomotic Leaks After Ivor Lewis Esophagectomy. World J Surg 2019;43:862-9. [Crossref] [PubMed]
- Jorgensen JO, Hunt DR. Endoscopic drainage of esophageal suture line leaks. Am J Surg 1993;165:362-4. [Crossref] [PubMed]
- Wehrmann T, Stergiou N, Vogel B, et al. Endoscopic debridement of paraesophageal, mediastinal abscesses: a prospective case series. Gastrointest Endosc 2005;62:344-9. [Crossref] [PubMed]
- Nakamoto K, Takeshige M, Fujii T, et al. Electrolyzed Saline Irrigation for Elimination of Bacterial Colonization in the Empyema Space. Surg Infect (Larchmt) 2016;17:724-9. [Crossref] [PubMed]
- Rosenfeldt FL, McGibney D, Braimbridge MV, et al. Comparison between irrigation and conventional treatment for empyema and pneumonectomy space infection. Thorax 1981;36:272-7. [Crossref] [PubMed]
- Kamarajah SK, Navidi M, Wahed S, et al. Anastomotic Leak Does Not Impact on Long-Term Outcomes in Esophageal Cancer Patients. Ann Surg Oncol 2020;27:2414-24. [Crossref] [PubMed]
- Ueno T, Toyooka S, Soh J, et al. Intrathoracic irrigation with arbekacin for methicillin-resistant Staphylococcus aureus empyema following lung resection. Interact Cardiovasc Thorac Surg 2012;15:437-41. [Crossref] [PubMed]


