
A novel method using a single lumen tube and extraluminal bronchial blocker for one-lung ventilation in severe tracheal stenosis: a case report
Introduction
The two principal devices used to establish lung isolation and one lung ventilation (OLV) include double-lumen tubes (DLT) (1) and bronchial blockers (BB), which were inserted through a conventional single-lumen tube (SLT) (2). However, when the airway is extremely narrowed, the appropriate DLT is difficult to insert. Meanwhile, it is difficult to simultaneously place BB and fiberoptic bronchoscopy in the narrow entrance of small SLT. In previous reports, a small SLT with pediatric wire-guided Arndt endobronchial blockers showed successful OLV in an adult patient with tracheal stenosis (3). The small SLT was inserted along with the detached blocker of a uninvent tube in a patient with tracheal stenosis for lung isolation (4). Nonintubated tracheal was used to maintain ventilation during stenosis tracheal resection surgery (5) and surgical pneumothorax may be an alternative method to achieve OLV in patients with more complicated airways (6). In this study, we describe an extraluminal technique for BB placement with minor SLT, which may be suitable for patients exhibiting airway stenosis during thoracic surgery. We present the following article in accordance with the CARE checklist (available at http://dx.doi.org/10.21037/apm-20-1676).
Case presentation
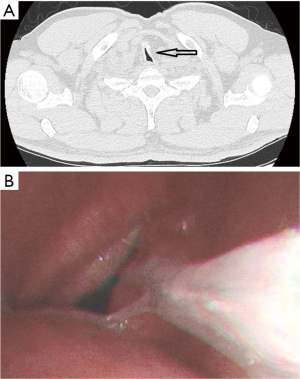
A 65-year-old man, 167 cm tall and weighing 80 kg, had a history of temporary tracheotomy due to traumatic brain hemorrhage eight years ago. He was found an upper left lobe nodule in the lung. However, a neck and chest computed tomography (CT) scan revealed serious tracheostenosis between cervical spine 7 and thoracic spine 1, the narrowest area measured 2.9 mm × 6.7 mm (Figure 1A). A bronchoscopy further confirmed that the middle of the trachea was narrowed (Figure 1B). The patient was diagnosed as tracheostenosis and an upper left lung lobe nodule. The patient was scheduled for video-assisted thoracoscopic lobectomy of an upper left lobe.
Standard monitoring systems were used to detect vital signs, including the measurement of invasive arterial blood pressure, heart rate, electrocardiogram, spectral entropy, and peripheral oxygen saturation.
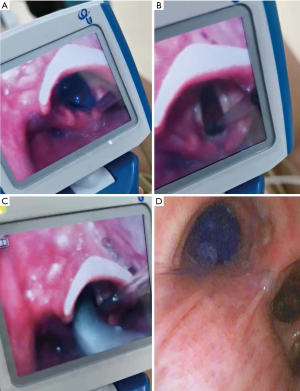
Anesthesia was administered using midazolam (0.025 mg/kg), lidocaine (1 mg/kg), etomidate (0.3 mg/kg) and sufentanil (0.3 µg/kg). After confirming mask ventilation, cistracurium (0.2 mg/kg) was administered for tracheal intubation. The glottis was exposed using video laryngoscopy. A BB (9 French, lubricated with silicone oil) was first inserted into the glottis and turned forward, to the left (Figure 2A,B). Next, a small SLT (5.5 mm inner diameter, lubricated by silicone oil) was inserted into the glottis and passed through the tracheal stenosis without resistance until the cuff passed the glottis (Figure 2C). Last, fiberoptic bronchoscopy was inserted into the SLT to adjust the BB to the left main stem bronchus (Figure 2D), ensuring that only right lung ventilation was occurring (Videos 1,2).
Collapse of the left lung using BB achieved optimal exposure for the operative field. Parameters for right-lung ventilation included a tidal volume of 6 mL/kg, respiratory frequency of 12 breaths/min, airway pressure of 17–20 cmH2O, pulse oximetry oxygen saturation of over 95% and end-tidal carbon dioxide 35–45 mmHg.
The intraoperative pathological diagnosis was confirmed to be adenocarcinoma and the patient underwent video-assisted thoracoscopic lobectomy of an upper left lobe. Both BB and SLT were removed after the surgery, no dyspnea, airway injury or edema were found. The postoperative pathologic diagnosis was adenocarcinoma in situ (pTaisN0M0). The patient recovered well and was discharged from the hospital a week after surgery.
The patient reported a comfortable experience from the start of anesthesia to extubation and showed no awareness. In addition, no dyspnea, sore throat, or hoarseness presented during the surgery.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient.
Discussion
The management of OLV in patients with tracheal stenosis requires both careful assessment and skilled manipulation. In this case, surgery of the left lobe of the lung was a good indication for BB. The pre-surgery evaluation suggested that the minor diameter of SLT could pass through the stenosed area. After confirming that mask ventilation was properly prepared, muscle relaxants were used for tracheal intubation. The standard approach for the placement of BB requires that the fiberoptic bronchoscopy is inserted into the lumen of the SLT. In small children, it is not feasible to place both the fiberoptic bronchoscopy and BB through the narrow lumen of SLT, therefore, extraluminal placement of BB is a viable alternative. The most significant advantage of extraluminal placement of BB is the absence of coupling between fiberoptic bronchoscopy and BB within SLT. Meanwhile, larger diameter of fiberoptic bronchoscopy provides optimal optics and visualization (7).
Thus, we were inspired to choose minor diameter tracheal tube ventilation combined with extraluminal placement of the BB to achieve left lung isolation. This also reduces intraluminal resistance and is easier to perform suctioning during ventilation. Studies showed that the extraluminal placement of BB was quicker than the well-accepted intraluminal approach (8).
However, extraluminal placement of BB remains some limitations. For example, it is unable to insert BB into the glottis in some cases with more difficult airways (9). In addition, it is difficult to assess damage of the trachea that might be caused by BB movement. If the patient has abnormal opening of right main bronchus, the right positioning of BB may be not feasible. The balloon dilatation or nitinol stent implantation prior to surgery may be an optional method. However, postoperative dyspnea after extubation was reported in a patient with balloon dilatation (10) and sputum retention is a significant complication related to stent implantation (11). A laryngeal mask combined with BB is another technique (12) but anesthesia management is complex. In this case, early extubation is helpful to reduce airway edema and the tracheotomy is prepared for possible postoperative dyspnea. Anyhow, extraluminal or intraluminal placement of BB should be the necessary techniques mastered by every thoracic anesthesiologist (13).
In summary, in cases of severe tracheal stenosis, minor SLT combined with extraluminal BB is a feasible method to obtain OLV during thoracic surgery, which is convenient for sputum suction and fiber optic bronchoscope examination. However, it is difficult to insert BB in patients with more complicated airways such as invisible glottis, and it is difficult to assess narrow airway edema and injury caused by BB and tracheal tubes while supraglottic airway devices and nonintubated methods may avoid these issues.
Acknowledgments
The authors would like to thank colleagues of the Department of Anesthesiology in First Hospital of China Medical University for technical support and helpful discussions.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-1676
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-1676). The authors have no conflicts of interest to declare.
Ethical Statement: Authors are accountable for all aspects of the work ensuring that questions related to the accuracy or integrity are appropriately investigated and resolved. Consent for publication and any accompanying images were obtained from the patient. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Campos JH. Which device should be considered the best for lung isolation: double-lumen endotracheal tube versus bronchial blockers. Curr Opin Anaesthesiol 2007;20:27-31. [Crossref] [PubMed]
- Zhang Y, Chen L, Ji H, et al. Anesthesia for aortic surgery with circulatory arrest in children with Loeys-Dietz syndrome. J Thorac Cardiovasc Surg 2019;157:e53-5. [Crossref] [PubMed]
- Lee DW, Hong JM, Park JH, et al. One-lung ventilation with pediatric Arndt endobronchial blocker in an adult patient with tracheal stenosis: A case report. Anesth Pain Med 2011;9:353-6.
- Asai T, Shingu K. One-lung ventilation in the patient with laryngeal or tracheal stenosis. Anesth Analg 2000;90:1000-1. [Crossref] [PubMed]
- Akopov A, Kovalev M. Nonintubated Tracheal Surgery. Thorac Surg Clin 2020;30:91-9. [Crossref] [PubMed]
- Yeh PH, Hsu PK. An alternative method to achieve one-lung ventilation by surgical pneumothorax in difficult lung isolation patient: a case report. J Anesth 2016;30:328-30. [Crossref] [PubMed]
- Adler AC. Extraluminal Use of a Pediatric Bronchial Blocker With Confirmation by Point-of-Care Ultrasound: A Case Report. A A Pract 2019;13:13-6. [Crossref] [PubMed]
- Templeton TW, Morris BN, Goenaga-Diaz EJ, et al. A Prospective Comparison of Intraluminal and Extraluminal Placement of the 9-French Arndt Bronchial Blocker in Adult Thoracic Surgery Patients. J Cardiothorac Vasc Anesth 2017;31:1335-40. [Crossref] [PubMed]
- Brodsky JB. Lung separation and the difficult airway. Br J Anaesth 2009;103 Suppl 1:i66-75. [Crossref] [PubMed]
- Li N, Zhu L, Sun J, et al. Difficulty in tracheal extubation followed by tracheal collapse after balloon dilatation for tracheal stenosis therapy: A case report. Medicine (Baltimore) 2018;97:e10907. [Crossref] [PubMed]
- Dahlqvist C, Ocak S, Gourdin M, et al. Corrigendum to "Fully Covered Metallic Stents for the Treatment of Benign Airway Stenosis". Can Respir J 2018;2018:6202750. [Crossref] [PubMed]
- Xu Z, Wang J, Yu J, et al. Report on the First Nonintubated Robotic-Assisted Thoracic Surgery. J Cardiothorac Vasc Anesth 2020;34:458-60. [Crossref] [PubMed]
- Valentine EA, Ochroch EA. Thinking Outside the Tube: Expanding the Armamentarium of the Thoracic Anesthesiologist. J Cardiothorac Vasc Anesth 2017;31:1341-2. [Crossref] [PubMed]


