
Association of acute normovolemic hemodilution with decreased length of hospital stay in rhesus-negative patients undergoing major cancer surgeries: a retrospective study
Introduction
Patients undergoing major cancer surgeries are at an increased risk of massive intraoperative bleeding due to the anatomic features of the surgical area, including the proximity to vasculature and the complexity of resections. Because safety is a major focus of surgical and perioperative care, preoperatively acquired blood and blood products remain a routine safeguard for patients undergoing major cancer surgeries. Based on demographic data, the prevalence of the rhesus (Rh)-negative population is 15% in North America and Europe, 4.8% to 6% in Nigeria, 6.49% in India, and 0.33% in the Han nationality population in China (1-3). Scarcity of Rh-negative donors compounds the blood shortage problem for this patient population. Shortages of allogeneic blood supplies may cause delays in cancer surgeries and prolong length of hospital stay (LOHS), resulting in a failure to achieve optimal timing for these procedures and an adverse effect on prognosis. Therefore, anesthesiologists and surgeons should figure out the appropriate autologous blood transfusion strategies for Rh-negative patients with cancer, and permit major cancer surgeries to be performed safely at the earliest without further delays.
Allogeneic blood transfusion (ABT) and, more specifically, the amount of intraoperative ABT in patients undergoing major cancer surgeries are associated with several adverse clinical outcomes, including increased mortality, recurrence, and complications (4-7). Due to an increasing awareness of the potential complications of ABT, many medical institutions have developed autologous blood transfusion strategies in the perioperative setting. The absolute risk/benefit ratio for intraoperative autologous cell salvage limits its application in patients undergoing cancer surgeries because of the risk of reinfusing cancer cells into the systemic circulation, which theoretically may promote cancer cell proliferation and metastasis (8). Acute normovolemic hemodilution (ANH), another autologous blood transfusion strategy, has been reported to reduce exposure to perioperative ABT in patients undergoing gynecological cancer surgery (9). Meanwhile, ANH use doesn’t increase incidence of post-operative complications in patients undergoing free-flap reconstruction of the head and neck (10). Compared with preoperative autologous donation (PAD) of 400 mL one week before surgery, ANH protocol has similar postoperative hematologic outcomes (11). Furthermore, ANH has been shown to be less costly than PAD (12), equally as efficacious, and to carry less risk of transfusion errors. Given the advantages of ANH, including lower cost, lower risk, less preoperative waiting time, and higher convenience, it can be considered an appropriate blood conservation technique for Rh-negative patients scheduled for major cancer surgeries.
The increasing cost of hospitalization is an important challenge for health policymakers in all countries. Average LOHS, an important and practical indicator, is commonly used to assess the quality of patient care and overall hospital efficiency (13). Preoperative low body weight, syndromic deformity, long period of operation, perioperative fluid administration, and postoperative complications are associated with longer LOHS (14). In addition, it has been suggested as an alternative primary outcome to assess the efficacy of ANH (15). However, there is limited information in the literature about the association between ANH and LOHS in Rh-negative patients scheduled for major cancer surgeries. With the aim of improving hospital efficiency, this retrospective study compared LOHS in Rh-negative patients undergoing major cancer surgeries who did or did not receive ANH. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-1327).
Methods
Setting and subjects
This retrospective study was conducted in the department of anesthesiology and perioperative medicine of the First Affiliated Hospital with Nanjing Medical University, Nanjing, China, from January 2015 and April 2020. We reviewed the electronic medical records of Rh-negative inpatients who underwent major cancer surgeries. The following exclusion criteria were used: preoperative hemoglobin (Hb) level of <100 g/L (9), non-cancer surgery, American Society of Anesthesiologists physical status (ASA-PS) score >3, and emergency surgery. Our institution started performing ANH for Rh-negative patients scheduled for major surgeries for cancer since January, 2019. Therefore, Rh-negative patients who had undergone cancer surgeries between July 1, 2015 and December 31, 2018 were included in the Control group. Therefore, the enrolled patients were distributed into Control group (n=40), and ANH group (n=30) based on whether preoperative ANH protocol was applied.
Ethics statement
The study was approved by the ethics committee of the First Affiliated Hospital with Nanjing Medical University (No. 2019-SR-235.A1). Our study conformed to the provisions of the Declaration of Helsinki (as revised in 2013). Informed consent was waived because the study was retrospective in design. Individual patient data were anonymized and stored in an encrypted computer.
Treatment
Upon arrival at the operating room, the patient’s Hb was confirmed to ensure the safety of ANH. Under monitoring by electrocardiography, oxygen saturation, and invasive radial artery blood pressure, ANH was conducted by a skilled attending anesthesiologist shortly after induction of anesthesia. The predetermined amount of autologous whole blood was withdrawn, while an equivalent volume of colloids (Voluven®, Fresenius Kabi, Germany) was transfused. ANH blood was collected into 200 or 400 mL Citrate Phosphate Dextrose collection bags (Shandong Weigao Group Medical Polymer Products Co., Ltd., Weihai, China) and stored at room temperature. If the duration of surgery was expected to exceed 4 hours, the blood bags were stored at 4 °C. ANH blood was transfused back into the patient before the end of the surgery or when reaching the transfusion threshold of a Hb of ≤70 g/L. ABT was performed if the Hb level was lower than 70 g/L after the autologous blood transfusion.
Demographic and baseline parameters
Baseline demographic variables were collected, including age, body mass index (BMI), gender, and ASA-PS classification. The presence of comorbid conditions, including hypertension, diabetes, and coronary artery disease, were documented. Types of surgery and baseline laboratory data [levels of Hb, hematocrit (Hct), and platelet (Plt)] were also recorded.
Outcomes
The primary outcome of this retrospective study was the difference in LOHS between the two groups. The secondary outcomes were length of preoperative stay (LOPS), perioperative Hb, Hct, and Plt levels, intraoperative input and blood loss, and perioperative ABT amount. The data of postoperative adverse events, including pulmonary complications, wound seroma/abscess/infection/dehiscence, bleeding requiring reoperation, ischemic events (myocardial/cerebral infarction), acute kidney injury (AKI), unscheduled admission to intensive care unit (ICU), and in-hospital death, were also collected. Meanwhile, relationships between these perioperative variables and LOHS were also examined by both univariate analyses and multiple linear regression analysis. In the univariate analyses, increased perioperative Hct and Plt levels and intraoperative crystalloids and colloids infusion defined as greater than means/medians of these variables, respectively.
Statistical analysis
All data were analyzed using SPSS version 22.0 (SPSS Inc., Chicago, Illinois, USA). Continuous variables were summarized and presented as means ± standard deviation (SD) or medians with 25–75% interquartile ranges (IQR), depending upon whether they were in accordance with the normal distribution. For data with a normal distribution, the unpaired Student’s t-test was used to assess the significance between the two groups. For data with a skewed distribution, the Mann-Whitney test was used. Categorical variables were expressed as frequencies (%) and the chi-square test was used for comparisons. Fisher’s exact test was used when the expected frequency was <5. Statistical significance was set at P<0.05.
Univariate analyses were performed using the unpaired Student’s t-test or one-way analysis of variance. Variables that met statistical significance on univariate analyses at P<0.05 were included in the multiple linear regression analysis. Multiple linear regression analysis was performed with backward elimination of nonsignificant variables, P<0.05 being taken as significant.
Results
Basic patient data and characteristics
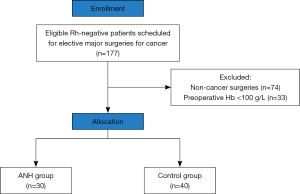
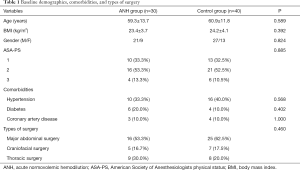
A total of 177 Rh-negative patients were screened for enrollment, with 107 patients excluded for the following reasons: non-cancer surgeries in 74 patients and preoperative Hb levels <100 g/L in 33 patients. The remaining 70 patients were divided into the ANH group (n=30) and the Control group (n=40). The patient flow chart is shown in Figure 1. The two groups were well-matched for baseline demographics, comorbidities, and types of surgery (Table 1).
Full table
Comparison of clinical indicators between the two groups
As shown in Figure 2, LOHS and LOPS were both significantly shorter in the Rh-negative patients who received ANH (P=0.004, P=0.009, respectively). Group sample size of 30 and 40 achieve 86.17% power to reject the null hypothesis of equal means when mean difference of LOHS is −4.0 with a standard deviation for both groups of 6.0 and with a significance level of 0.05 using a one-sided two-sample equal-variance t-test.

Rh-negative patients who underwent ANH had a median withdrawal amount of 400 mL of autologous blood. Levels of Hb and Hct in the ANH group and Plt counts in the Control group were lower on postoperative day (POD) 1 than during the preoperative evaluation (Figure 3, P=0.023, P=0.012, P=0.042, respectively).

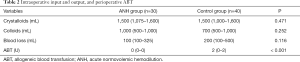
As shown in Table 2, the amount of perioperative ABT was lower in the Rh-negative patients treated with ANH [0 U (IQR, 0–0) vs. 2 U (IQR, 0–2), P<0.001]. There were no significant differences between the two groups in the volumes of intraoperative crystalloids and colloids infusion as well as intraoperative blood loss.
Full table
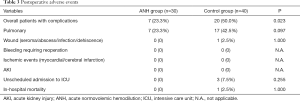
As shown in Table 3, the overall rate of postoperative adverse events during the hospital stay was significantly lower in the ANH group (23.3%) than in the Control group (50.0%) (P=0.023). The most reported adverse event was pulmonary complication occurring in seven patients in the ANH group and seventeen patients in the Control group (23.3% vs. 42.5%, P=0.097), respectively. In the Control group, one patient (2.5%), three patients (7.5%), and one patient (2.5%) suffered from wound infection, unscheduled admission to ICU, and in-hospital death, respectively. None of the patients were reported to experience the following postoperative complications: bleeding requiring reoperation, ischemic events, and AKI.
Full table
Association between ANH and LOHS
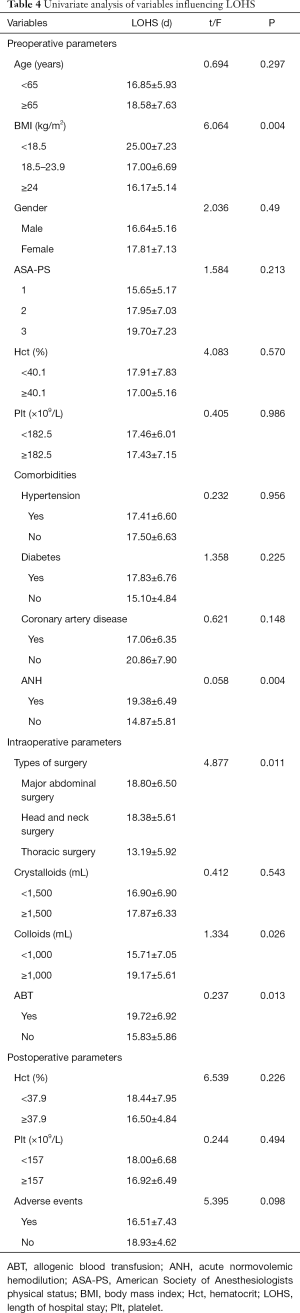
The distribution of LOHS was displayed in Figure 4. Univariate analyses of the relationships between the perioperative variables and LOHS were presented in Table 4. On univariate analyses, ANH (P=0.004), BMI (P=0.004), types of surgery (P=0.011), intraoperative colloids infusion (P=0.026), and perioperative ABT (P=0.013) were significantly associated with LOHS.
Full table
As shown in Table 5, multiple linear regression analysis with correction for diagnosis identified ANH (P=0.018), intraoperative colloids infusion (P<0.001), and perioperative ABT (P=0.001) as independent predictors. The overall r2 for the model was 0.425. ANH protocol was more likely to shorten LOHS (B=−3.378). On the contrary, Rh-negative patients with increased intraoperative colloids infusion and perioperative ABT were more likely to have prolonged LOHS (B=0.007, B=1.369, respectively).

Full table
Discussion
LOHS has been suggested as an alternative primary outcome to assess the efficacy of ANH (16). During the coronavirus disease 2019 pandemic, ANH has been confirmed to permit major cancer surgeries to be performed safely and at the earliest in a situation of insufficient allogenic blood supplies (17). This retrospective study showed that ANH, performed shortly after induction of anesthesia, was associated with the decreased LOHS in Rh-negative patients undergoing major cancer surgeries. The model obtained after multiple linear regression analysis using those perioperative variables, with correction for diagnosis, revealed that ANH is an independent predictor of LOHS in this patient population.
With a global movement toward minimally invasive laparoscopic procedures, rates of intraoperative massive bleeding have declined. For example, only 1 in 800 patients who underwent robotic prostatectomies at the Johns Hopkins Medical Institutions received ABTs in 2012 (18). However, preoperatively acquired blood and blood products remain a routine scheme for perioperative safety in patients undergoing major cancer surgeries. Despite the modest ABT requirements for hip surgeries currently, the use of ANH may reduce postoperative complications and decrease postoperative hospital stay (19). In the present study, the overall rate of postoperative adverse events during the hospital stay was significantly lower in the Rh-negative patients treated with ANH. Although there are now several alternative methods for blood conservation, cancer surgery may be the ideal setting for the specific use of ANH, especially when Rh-negative patients present with a high Hct and undergo a substantial blood loss, a situation in which the hemostatic benefits of fresh whole blood are readily apparent (20).
ANH improved microcirculation and oxygenation in ischemic and hypoxic flap tissue in adult minipigs (21). Using multiple-plane transesophageal echocardiography, moderate ANH was found to maintain left ventricular systolic and diastolic function in anaesthetized patients with coronary artery disease. ANH-induced decreases in blood viscosity led to an increased stroke volume that was primarily related to increased venous return and higher cardiac preload (22). Therefore, although ANH induced slight decreases in Hb and Hct levels at POD 1, it would not induce or clinically worsen relevant ischemic diseases such as myocardial/cerebral infarction.
ANH-induced administration of 2 L or more of intraoperative fluid was associated with increased occurrence of postoperative pancreatic anastomoses (leak/fistula/abscess) in patients undergoing pancreaticoduodenectomies (23). Colloids replacement has been shown to lead to less renal edema and unimpaired renal microvascular oxygenation in pigs treated with ANH to a hematocrit of 15% (24). Administration of Hydroxyethyl Starch as the replacement fluid during ANH is associated with a more stable mean arterial pressure (25). A recently published retrospective study showed that ANH did not increase the risk of AKI, even though ANH increased occurrences of anemia, hyperchloremia, and metabolic acidosis during surgery (26). We concurrently administered equivalent volumes of colloid, without larger volumes of crystalloids, to maintain normovolemia during ANH procedure in our hospital. We found that none of Rh-negative patients with ANH use were reported to experience AKI or wound complications by using ANH protocol.
A retrospective cohort study revealed that the use of colloids and erythrocyte transfusion are associated with prolonged duration of recovery after colorectal surgery (27). Therefore, the shortened LOHS may be partially due to ANH-related decrease in the perioperative ABT use in our present study. Intraoperative colloids administration is a significant predictor of increased LOHS in patients undergoing 1 level minimally invasive transforaminal lumbar interbody fusions (28). In the present study, we found that intraoperative colloids infusion predicts longer LOHS in Rh-negative patients scheduled for major cancer surgeries. Although equivalent volumes of colloids replacement for ANH use were administered in our hospital, it did not lead to increase in the amount of intraoperative colloids infusion. In other words, ANH-induced additional colloids infusion might not be associated with the prolonged LOHS.
The limitations of the present study include its retrospective design with its lack of randomization and inherent inability to identify all confounding variables. A well-designed prospective study is needed to better evaluate the overall efficiency of ANH in this patient population. Second, despite of heterogeneity in the types of enrolled surgery, these patients face the common problem of scarcity of Rh-negative allogeneic blood supplies during the perioperative stage. We mainly investigated the perioperative ANH-related outcomes in the present study. ANH was shown to be associated with the decreased LOHS and LOPS without increasing postoperative adverse events in Rh-negative patients undergoing major cancer surgeries. Finally, the prevalence of the Rh-negative population is 0.33% in the Han nationality population in China. The total number of Rh-negative patients scheduled for major cancer surgeries is limited. In the present study, we only enrolled the electronic medical records of seventy appropriate Rh-negative cancer patients. However, the two groups were well-matched for baseline demographics, comorbidities, and types of surgery, which guarantee the reliability of results.
Conclusions
In Rh-negative patients, ANH facilitates major cancer surgeries to be performed safely at the earliest without further delays, resulting in a decreased LOPS. ANH is also associated with the decreased perioperative ABT and occurrence of postoperative adverse events. Taken together, these beneficial factors contribute to ANH-related decrease in LOHS in this patient population.
Acknowledgments
We would like to thank Editage (www.editage.com) for English language editing.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-1327
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-1327
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-1327). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the Institutional Ethics Committee of the 1st Affiliated Hospital of Nanjing Medical University, Nanjing, China (No. 2019-SR-235.A1). Our study conformed to the provisions of the Declaration of Helsinki (as revised in 2013). Informed consent was waived because the study was retrospective in design.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zipursky A, Paul VK. The global burden of Rh disease. Arch Dis Child Fetal Neonatal Ed 2011;96:F84-5. [Crossref] [PubMed]
- Pan QR, Zhong J, Yang Y, et al. The investigation and analysis of the Rh blood type distribution in four kinds of the minority nationalities (Miao, Buyi, Dong and Shui) in Guizhou, China. Zhonghua Yi Xue Yi Chuan Xue Za Zhi 2006;23:571-3. [PubMed]
- Kumar S, Modak PK, Ali SH, et al. A retrospective study: ABO and Rh phenotype blood group distribution among blood donors in H.N.B. Base Hospital, Srinagar, Uttarakhand, India. J Family Med Prim Care 2018;7:34-8. [Crossref] [PubMed]
- Acheson AG, Brookes MJ, Spahn DR. Effects of allogeneic red blood cell transfusions on clinical outcomes in patients undergoing colorectal cancer surgery: a systematic review and meta-analysis. Ann Surg 2012;256:235-44. [Crossref] [PubMed]
- Sun C, Wang Y, Yao HS, et al. Allogeneic blood transfusion and the prognosis of gastric cancer patients: Systematic review and meta-analysis. Int J Surg 2015;13:102-10. [Crossref] [PubMed]
- Wada H, Eguchi H, Nagano H, et al. Perioperative allogenic blood transfusion is a poor prognostic factor after hepatocellular carcinoma surgery: A multi-center analysis. Surg Today 2018;48:73-9. [Crossref] [PubMed]
- Yao HS, Wang Q, Wang WJ, et al. Intraoperative allogeneic red blood cell transfusion in ampullary cancer outcome after curative pancreatoduodenectomy: A clinical study and meta-analysis. World J Surg 2008;32:2038-46. [Crossref] [PubMed]
- Sikorski RA, Rizkalla NA, Yang WW, et al. Autologous blood salvage in the era of patient blood management. Vox Sang 2017;112:499-510. [Crossref] [PubMed]
- Saito J, Masui K, Noguchi S, et al. The efficacy of acute normovolemic hemodilution for preventing perioperative allogeneic blood transfusion in gynecological cancer patients. J Clin Anesth 2020;60:42-3. [Crossref] [PubMed]
- Takekawa D, Saito J, Kinoshita H, et al. Acute normovolemic hemodilution reduced allogeneic blood transfusion without increasing perioperative complications in patients undergoing free-flap reconstruction of the head and neck. J Anesth 2020;34:187-94. [Crossref] [PubMed]
- Terada N, Arai Y, Matsuta Y, et al. Acute normovolemic hemodilution for radical prostatectomy: Can it replace preoperative autologous blood transfusion? Int J Urol 2001;8:149-52. [Crossref] [PubMed]
- Goodnough LT, Despotis GJ, Merkel K, et al. A randomized trial comparing acute normovolemic hemodilution and preoperative autologous blood donation in total hip arthroplasty. Transfusion 2000;40:1054-7. [Crossref] [PubMed]
- Mohammadkarim B, Jamil S, Pejman H, et al. Combining multiple indicators to assess hospital performance in Iran using the Pabon Lasso Model. Australas Med J 2011;4:175-9. [Crossref] [PubMed]
- Kato S, Dear T, Lewis SJ. Factors affecting length of stay following 3-column spinal osteotomies in pediatric patients. Global Spine J 2021;11:154-60. [Crossref] [PubMed]
- Rekman J, Wherrett C, Bennett S, et al. Safety and feasibility of phlebotomy with controlled hypovolemia to minimize blood loss in liver resections. Surgery 2017;161:650-7. [Crossref] [PubMed]
- Grant MC, Resar LMS, Frank SM. The efficacy and utility of acute normovolemic hemodilution. Anesth Analg 2015;121:1412-4. [Crossref] [PubMed]
- Ni Y, Xu ZJ, Zhang ZF, et al. Acute normovolemic hemodilution for major cancer surgeries during the COVID-19 pandemic: A beacon of hope. J Clin Anesth 2020;65:109871. [Crossref] [PubMed]
- Frank SM, Rothschild JA, Masear CG, et al. Optimizing preoperative blood ordering with data acquired from an anesthesia information management system. Anesthesiology 2013;118:1286-97. [Crossref] [PubMed]
- Bennett J, Haynes S, Torella F, et al. Acute normovolemic hemodilution in moderate blood loss surgery: A randomized controlled trial. Transfusion 2006;46:1097-103. [Crossref] [PubMed]
- Triulzi DJ, Ness PM. Intraoperative hemodilution and autologous platelet rich plasma collection: Two techniques for collecting fresh autologous blood. Transfus Sci 1995;16:33-44. [Crossref] [PubMed]
- Schramm S, Wettstein R, Wessendorf R, et al. Acute normovolemic hemodilution improves oxygenation in ischemic flap tissue. Anesthesiology 2002;96:1478-84. [Crossref] [PubMed]
- Licker M, Ellenberger C, Sierra J, et al. Cardiovascular response to acute normovolemic hemodilution in patients with coronary artery diseases: Assessment with transesophageal echocardiography. Crit Care Med 2005;33:591-7. [Crossref] [PubMed]
- Fischer M, Matsuo K, Gonen M, et al. Relationship between intraoperative fluid administration and perioperative outcome after pancreaticoduodenectomy: Results of a prospective randomized trial of acute normovolemic hemodilution compared with standard intraoperative management. Ann Surg 2010;252:952-8. [Crossref] [PubMed]
- Konrad FM, Mik EG, Bodmer SIA, et al. Acute normovolemic hemodilution in the pig is associated with renal tissue edema, impaired renal microvascular oxygenation, and functional loss. Anesthesiology 2013;119:256-69. [Crossref] [PubMed]
- Jones SB, Whitten CW, Monk TG. Influence of crystalloid and colloid replacement solutions on hemodynamic variables during acute normovolemic hemodilution. J Clin Anesth 2004;16:11-7. [Crossref] [PubMed]
- Mikami N, Saito J, Ohyama T, et al. Acute normovolemic hemodilution and acute kidney injury after open abdominal cancer surgery. J Clin Anesth 2020;61:109657. [Crossref] [PubMed]
- Aga Z, Machina M, McCluskey SA. Greater intravenous fluid volumes are associated with prolonged recovery after colorectal surgery: A retrospective cohort study. Br J Anaesth 2016;116:804-10. [Crossref] [PubMed]
- Siemionow K, Pelton MA, Hoskins JA, et al. Predictive factors of hospital stay in patients undergoing minimally invasive transforaminal lumbar interbody fusion and instrumentation. Spine (Phila Pa 1976) 2012;37:2046-54. [Crossref] [PubMed]


