
Efficacy and safety of pudendal nerve block for postoperative analgesia of hemorrhoids: a systematic review of 7 randomized controlled trials
Introduction
The incidence of hemorrhoids remains the highest among anorectal diseases, and its prevalence is unclear. Relevant epidemiological studies have reported that the incidence of hemorrhoids in American adults is 4.4% (1). Surgery is one of the effective therapeutic ways of hemorrhoids. Nevertheless, the severe pain caused by hemorrhoid surgery is a difficult postoperative problem to be urgently solved (2).
There are many analgesia methods after hemorrhoidectomy, such as medication of analgesics [e.g., opioid analgesia, non-steroidal anti-inflammatory drugs (NSAIDs)], somatosensory stimulation treatments and narcotic analgesia (3-5). Analgesics are often effective, whilst their side effects should not be neglected. The PROSPECT group recommended the necessary application of PNB in operated hemorrhoid patients, aiming to relieve postoperative pain (6). PNB is widely used in the operation of anorectal diseases. It not only exerts an effective analgesic function, but also successfully reduces the complications after hemorrhoidectomy (7). The pudendal nerve originates from the anterior branch of the spinal nerve from S2 to S4, which is divided into anal nerve, perineal nerve, and penis (pedicle) dorsal nerve (8). Conventional PNB is conducted under the guidance of ultrasound, CT or nerve stimulator (8-10). It is more advantageous than other anesthesia methods in postoperative analgesia of hemorrhoids. Compared with spinal anesthesia, patients receiving PNB after hemorrhoidectomy have longer analgesia and lower incidence of urinary retention (8). Moreover, compared with general anesthesia, patients receiving PNB are less suffer from the painful defecation and they can return to normal work faster (7).Compared with local infiltration anesthesia, application of PNB can reduce the incidences of perianal swelling, hematoma and other complications (11). However, some defects of PNB should be noteworthy, and their effectiveness is still uncertain.
PNB is suitable for hemorrhoidectomy and postoperative relieve of pain, which is an optional pain management strategy. This systematic review aims to compare the effectiveness and safety of PNB with other anesthesia methods under different approaches of guidance. The randomized controlled trial (RCT) meta-analysis was conducted to evaluate the beneficial effects of PNB in analgesia after hemorrhoid surgery.
We present the following article in accordance with the PRISMA reporting checklist (available at http://dx.doi.org/10.21037/apm-20-2109).
Methods
Search strategy
RCTs of the application of PNB in hemorrhoidectomy were searched in PubMed, Embase, Web of Science, the Cochrane Central Register of Controlled Trials (CENTRAL), the China Network Knowledge Infrastructure (CNKI), the Wan Fang Database and Chinese Biomedicine (CBM). Literatures published before 7st September, 2020 were searched. We combined keywords from MeSH headings with self-generated keywords to screen studies, which were limited in Chinese or English language. In addition, relevant reports in online websites, including Clinical Trials (http://www.clinicaltrials.gov) and the Chinese Clinical Trial Registry (http://www.chictr.org.cn/index.aspx) were searched. In brief, a combination of medical subject headings without language limitation were searched online: including hemorrhoids, hemorrhoid, pudendal block, pudendal nerve block, mixed hemorrhoids, hemorrhoidectomy. No limitations were set on the race and gender of subjects. We also uploaded the search strategy as supplementary materials.
Inclusion criteria
After comprehensive searching for clinical studies, two reviewers (Y.L, JC.L) independently screened titles and abstracts, and downloaded the full text when necessary. Inclusion criteria were as follows: (I) patients were diagnosed as hemorrhoids, and there were no limitations on age, gender, race and duration of disease; (II) PNB was the intervention method, and spinal anesthesia or no special application of anesthesia was considered as the control; (III) the primary outcome was the visual analogue scale (VAS) score, and the secondary outcomes were urinary retention, bleeding, the need for analgesics, and side effects (e.g., dizziness, nausea, vomiting, etc.); (IV) RCTs published in Chinese or English language without a limitation on the study year.
Exclusion criteria
Exclusion criteria were as follows: (I) hemorrhoid patients combined with other diseases; (II) intervention/control methods were not eligible; (III) outcome indicators cannot be quantified; (IV) non-RCT studies or non-clinical trial researches; (V) duplicated or incomplete studies; (VI) full-text studies were not obtained. Any disagreements were solved by the third reviewer (KJ.Q). A more comprehensive study was included once there were replicated data in several studies.
Data extraction
Two reviewers (KJ.Q, JC.L) were responsible for extracting data, including first author, publication year, sample size (the treatment group and control group), infiltration technique, hemorrhoid grade, VAS scores, urinary retention, bleeding, antalgesic need and side effects (SEs). Any disagreement was solved by the third reviewer (MJ.L).
Assessment of bias
Two reviewers (CJ.L, Y.L) independently analyzed the risk of bias by using the Cochrane Handbook. The risk of bias was divided into low risk, high risk, and unclear risk based on the following criteria: (I) random sequence generation, (II) allocation concealment, (III) blinding of participants and personnel, (IV) blinding of outcome assessment, (V) incomplete outcome data, (VI) selective reporting, and (VII) other bias. If there was a disagreement, the third reviewer (H.L) was responsible for achieving a consensus after discussion. Since the number of trials was less than 10, we did not conduct reporting bias assessment.
Data analysis
ReviewManager 5.3 software, provided by the Cochrane Collaboration, was used to evaluate data. Odds ratio (OR) of dichotomous data, as well as the mean difference (MD) and standard mean difference (SMD) with a 95% confidence interval (CI) were calculated. The heterogeneity test was conducted by analyzing I2 statistics. A fixed-effect model was adopted if there was homogeneity (P>0.1, I2<50%); Otherwise, a random-effects model was used. Subgroup analysis was conducted to avoid heterogeneity. A sensitivity analysis was conducted if the heterogeneity was affected by a single study or the incomplete data of included study.
Results
Study inclusion
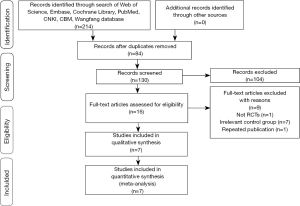
According to the retrieval strategy, a total of 214 studies were initially included, from which 84 were duplicate ones. After reviewing the abstract and full text, 104 non-eligible studies were excluded. Then, 9/16 studies were further excluded, including 1 non-RCT, 7 studies with irrelevant control methods, and 1 republished study. Finally, 7 eligible studies were included in the present study. The flow chart of screen strategy was listed in Figure 1.
Study characteristics and quality assessment
Included 7 RCTs involved a total of 560 participants. Baseline characteristics between the experimental group and the control group were comparable. Among them, control check was performed in the control group of 4 studies, and spinal anesthesia was conducted in the control group of remaining ones. VAS score was graded in all studies as the observed outcome. Characteristics of the included studies were shown in Table 1.
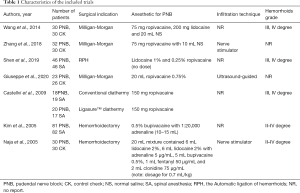
Full table
The 7 included studies all reported random sequence generation. One of the studies adopted the double-blinding way. Complete outcomes were reported in all studies. Due to the small sample size and limited data, we were unable determine whether there were other bias factors (Figure 2).
Primary outcomes
VAS score
In each study, VAS score in the experimental group and control group was assessed. In particular, we compared VAS score at different time points between groups.
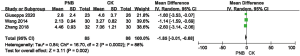
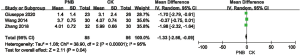
In the studies of conducted by Di Giuseppe (12), Zhang (13) and Wang (14), VAS score at 6 h after hemorrhoidectomy in the experimental group was lower than that of the control group that was lack of any intervention (MD, −2.84; 95% CI, −3.56 to −2.12; P<0.00001) (Figure 3).
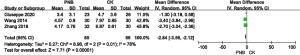
Similarly, VAS score at 12 h after hemorrhoidectomy in the experimental group was lower than that of the control group (MD, −1.85; 95% CI, −3.01 to −0.68; P=0.002) (Figure 4).
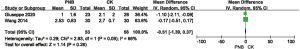
In Di Giuseppe (12), Zhang (13) and Wang (14)’s studies, VAS score at 24 h after hemorrhoidectomy in the experimental group was comparable with that of the control group (MD, −0.51; 95% CI, −1.39–0.37; P=0.26) (Figure 5).
As expected, VAS score at 48 h after hemorrhoidectomy in the experimental group was also lower than that of the control group (MD, −1.33; 95% CI, −2.56 to −0.09; P=0.04) (Figure 6).
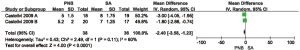
Two RCTs reported VAS score at the first time of defecation. Patients receiving PNB postoperatively had a lower VAS score at the first time of defecation than those treated with spinal anesthesia (MD, −2.40; 95% CI, −3.58 to −1.23; P<0.00001) (Figure 7).
Secondary outcomes
Urinary retention
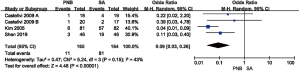
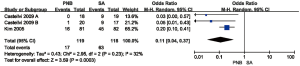
Urinary retention is one of the common complications after hemorrhoidectomy. In comparison with the control group, the urinary retention incidence in the PNB group was of no significant difference (OR, 0.45; 95% CI, 0.13–1.56; P=0.21) (Figure 8). On the contrary, the incidence in the PNB group was lower than that in the spinal anesthesia group (OR, 0.09; 95% CI, 0.03–0.26; P<0.00001) (Figure 9).
Bleeding
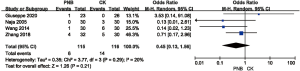
Three studies reported the incidence of postoperative bleeding. The results showed that there was no significant difference in the incidence of bleeding between PNB group and control group (OR, 0.08; 95% CI, 0.09–7.45; P=0.84) (Figure 10).
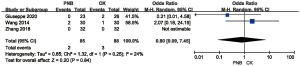
Analgesics need
Postoperative pain is the most difficult problem to be solved after hemorrhoidectomy. Analgesics are usually required to be applied. Our results showed that the use of analgesics was less frequent in patients receiving PNB compared with that of controls (OR, 0.11; 95% CI, 0.04–0.37; P=0.0003) (Figure 11).
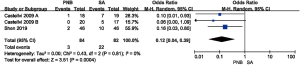
Side effects
SEs included dizziness, vomiting, and nausea. PNB intervention caused less SEs than that of controls (OR, 0.12; 95% CI, 0.04–0.39; P=0.004) (Figure 12).
Publication bias
Publication bias could not be assessed since fewer than 10 studies were included.
Discussion
A systematic review involving seven studies was conducted to evaluate the efficacy and safety of PNB on postoperative analgesia of hemorrhoids. Although there is no guideline or international standard about the application of PNB in hemorrhoid surgery, a considerable number of clinical trials demonstrated its effectiveness as assessed by VAS (12). Therefore, VAS score was used in this systematic review to reflect the efficacy of PNB or control. It is found that PNB has a certain effect on analgesia after hemorrhoidectomy. Furthermore, VAS score was better in patients receiving PNB than that of controls regardless of the postoperative time point, and the incidence of urinary retention was reduced. In addition, the incidence of side effects was less frequently observed in the PNB group.
Hemorrhoids is a kind of multiple anorectal diseases. Although surgery is the most effective treatment for hemorrhoids, postoperative pain is considered to be one of the main reasons for the refusal of patients to be operated (15). Perioperative analgesia mainly relies on local anesthesia and analgesics (2), in addition to topical diltiazem (16) or metronidazole (17), acupoint stimulation (18) and ischiorectal block (17). Nevertheless, their analgesic efficacy is still not satisfactory. PNB is mainly employed for anorectal diseases by blocking the anal nerve in the pudendal nerve bifurcation to relieve pain. Due to the anatomical structure, PNB can be used as an effective analgesic method after hemorrhoid surgery, which also reduces the occurrence of complications (19-22).
In the present study, PNB was identified to be better than spinal anesthesia or no treatment of anesthesia. A previous study reported that patients receiving PNB have fewer side effects and they can be discharged as soon as possible (23). A randomized study concluded that patients receiving PNB have less demand for opioids, which is consistent with our results (24). With the development of new technologies, more and more instruments have emerged, such as ultrasound, neurostimulator, CT, etc. (25-27). These instruments can be selected based on individualized conditions to locate the nerve and improve the safety of the operation. Naja et al. (28) suggested that PNB can significantly relieve postoperative pain, so that the patient can return to normal work as soon as possible. Although PNB is rarely used in anorectal surgery, it is a new option for postoperative analgesia of hemorrhoids.
This systematic review showed that PNB has certain advantages in analgesia and relevant indicators after hemorrhoidectomy. However, it still has several limitations. First of all, the quality of the included studies was not very well. Only four studies reported random sequence generation based on random number tables or computer. The remaining only mentioned the word “random”. Secondly, the sample size of included studies was small, which may cause biases. Thirdly, only 1/7 studies reported postoperative bleeding, which may influence the judgment on postoperative indicators. Consequently, selection and detection biases in the included studies could be pronounced.
Taken together, PNB is a common efficient analgesic strategy used after hemorrhoidectomy. In comparison with other recent studies, our perspective focuses on the three main aspects of PNB anesthesia in analgesia, alleviation of complications and reduction of side effects after hemorrhoid surgery (29,30). PNB has its unique advantages due to the special anatomical structure. In addition, the time point of other analgesic methods to be conducted after PNB requires to be further analyzed. Our results about the effectiveness and safety of PNB after hemorrhoidectomy should be validated in large sample-size and high-quality RCTs in the future.
Acknowledgments
Funding: This study was supported by Shanghai Municipal Health Commission (Youth) Project, China (20174Y0233) and Graduate Student Innovation Ability Project of Shanghai University of Traditional Chinese Medicine, China (Y2020071).
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-2109
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-2109). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Johanson JF, Sonnenberg A. The prevalence of hemorrhoids and chronic constipation. An epidemiologic study. Gastroenterology 1990;98:380-6. [Crossref] [PubMed]
- Acheson AG, Scholefield JH. Management of haemorrhoids. Bmj 2008;336:380-3. [Crossref] [PubMed]
- Lu PW, Fields AC, Andriotti T, et al. Opioid Prescriptions After Hemorrhoidectomy. Dis Colon Rectum 2020;63:1118-26. [Crossref] [PubMed]
- Gupta A, Bah M. NSAIDs in the Treatment of Postoperative Pain. Curr Pain Headache Rep 2016;20:62. [Crossref] [PubMed]
- Zhang AM, Chen M, Tang TC, et al. Somatosensory stimulation treatments for postoperative analgesia of mixed hemorrhoids: Protocol for a systematic review and network meta-analysis. Medicine (Baltimore) 2019;98:e14441. [Crossref] [PubMed]
- Sammour T, Barazanchi AW, Hill AG. Evidence-Based Management of Pain After Excisional Haemorrhoidectomy Surgery: A PROSPECT Review Update. World J Surg 2017;41:603-14. [Crossref] [PubMed]
- Naja Z, El-Rajab M, Al-Tannir M, et al. Nerve stimulator guided pudendal nerve block versus general anesthesia for hemorrhoidectomy. Can J Anaesth 2006;53:579-85. [Crossref] [PubMed]
- Kim J, Lee DS, Jang SM, et al. The effect of pudendal block on voiding after hemorrhoidectomy. Dis Colon Rectum 2005;48:518-23. [Crossref] [PubMed]
- Gruber H, Kovacs P, Piegger J, et al. New, simple, ultrasound-guided infiltration of the pudendal nerve: topographic basics. Dis Colon Rectum 2001;44:1376-80. [Crossref] [PubMed]
- Labat JJ, Riant T, Lassaux A, et al. Adding corticosteroids to the pudendal nerve block for pudendal neuralgia: a randomised, double-blind, controlled trial. Bjog 2017;124:251-60. [Crossref] [PubMed]
- Tepetes K, Symeonidis D, Christodoulidis G, et al. Pudendal nerve block versus local anesthesia for harmonic scalpel hemorrhoidectomy: a prospective randomized study. Tech Coloproctol 2010;14 Suppl 1:S1-3. [Crossref] [PubMed]
- Di Giuseppe M, Saporito A, La Regina D, et al. Ultrasound-guided pudendal nerve block in patients undergoing open hemorrhoidectomy: a double-blind randomized controlled trial. Int J Colorectal Dis 2020;35:1741-7. [Crossref] [PubMed]
- Zhang JR, Liu XH, Zeng J. Observation on the effect of pudendal nerve detector positioning + block for relieving postoperative pain of circular mixed hemorrhoids. Henan Journal of Surgery 2018;24:88-9.
- Wang T, Luo M, Chen S, et al. Clinical observation of pudendal nerve block for postoperative analgesia of mixed hemorrhoids. Chinese Electronic Journal of Colorectal Diseases 2014;3:99-101.
- Engel AF, Eijsbouts QA. Haemorrhoidectomy: painful choice. Lancet 2000;355:2253-4. [Crossref] [PubMed]
- Huang YJ, Chen CY, Chen RJ, et al. Topical diltiazem ointment in post-hemorrhoidectomy pain relief: A meta-analysis of randomized controlled trials. Asian Journal of Surgery 2018;41:431-7. [Crossref] [PubMed]
- Abbas ST, Raza A, Muhammad Ch I, et al. Comparison of mean pain score using topical and oral metronidazole in post milligan morgan hemorrhoidectomy patient; A randomized controlled trial. Pak J Med Sci 2020;36:867-71. [Crossref] [PubMed]
- Wang X, Yin X, Guo XT, et al. Effects of the pestle needle therapy, a type of acupoint stimulation, on post-hemorrhoidectomy pain: A randomized controlled trial. J Integr Med 2020;18:492-8. [Crossref] [PubMed]
- Nadri S, Mahmoudvand H, Rokrok S, et al. Comparison of Two Methods: Spinal Anesthesia and Ischiorectal Block on Post Hemorrhoidectomy Pain and Hospital Stay: A Randomized Control Trial. J Invest Surg 2018;31:420-4. [Crossref] [PubMed]
- Gabrielli F, Cioffi U, Chiarelli M, et al. Hemorrhoidectomy with posterior perineal block: experience with 400 cases. Dis Colon Rectum 2000;43:809-12. [Crossref] [PubMed]
- Luck AJ, Hewett PJ. Ischiorectal fossa block decreases posthemorrhoidectomy pain: randomized, prospective, double-blind clinical trial. Dis Colon Rectum 2000;43:142-5. [Crossref] [PubMed]
- Rajabi M, Hosseinpour M, Jalalvand F, et al. Ischiorectal block with bupivacaine for post hemorrhoidectomy pain. Korean J Pain 2012;25:89-93. [Crossref] [PubMed]
- Bessa SS, Katri KM, Abdel-Salam WN, et al. Spinal versus general anesthesia for day-case laparoscopic cholecystectomy: a prospective randomized study. J Laparoendosc Adv Surg Tech A 2012;22:550-5. [Crossref] [PubMed]
- Imbelloni LE, Vieira EM, Gouveia MA, et al. Pudendal block with bupivacaine for postoperative pain relief. Dis Colon Rectum 2007;50:1656-61. [Crossref] [PubMed]
- Rofaeel A, Peng P, Louis I, et al. Feasibility of real-time ultrasound for pudendal nerve block in patients with chronic perineal pain. Reg Anesth Pain Med 2008;33:139-45. [Crossref] [PubMed]
- Aksu C, Akay MA, Şen MC, et al. Ultrasound-guided dorsal penile nerve block vs neurostimulator-guided pudendal nerve block in children undergoing hypospadias surgery: A prospective, randomized, double-blinded trial. Paediatr Anaesth 2019;29:1046-52. [Crossref] [PubMed]
- Aoun F, Mjaess G, Assaf J, et al. Clinical effect of computed guided pudendal nerve block for patients with premature ejaculation: a pilot study. Scand J Urol 2020;54:258-62. [Crossref] [PubMed]
- Naja Z, Ziade MF, Lönnqvist PA. Nerve stimulator guided pudendal nerve block decreases posthemorrhoidectomy pain. Can J Anaesth 2005;52:62-8. [Crossref] [PubMed]
- Xia W, MacFater HS, MacFater WS, et al. Local Anaesthesia Alone Versus Regional or General Anaesthesia in Excisional Haemorrhoidectomy: A Systematic Review and Meta-Analysis. World J Surg 2020;44:3119-29. [Crossref] [PubMed]
- Mohamedahmed AYY, Stonelake S, Mohammed SSS, et al. Haemorrhoidectomy under local anaesthesia versus spinal anaesthesia: a systematic review and meta-analysis. Int J Colorectal Dis 2020;35:2171-83. [Crossref] [PubMed]



