
The effect of comfort care based on the collaborative care model on the compliance and self-care ability of patients with coronary heart disease
Introduction
Coronary heart disease (CHD) has gradually developed into one of the causes that seriously threaten people’s life and health, with a high prevalence, long course of illness, and high disease severity. Moreover, relapse of CHD is common (1). CHD causes significant physical, mental, social, and emotional discomfort in patients, resulting in anxiety, depression, and other adverse psychological impacts (1). Some CHD patients lack knowledge about the disease and its treatment, which affects their compliance and self-care ability, and ultimately affects their rehabilitation (2). Therefore, there is a pressing need to strengthen the nursing cooperation with patients during treatment, which can help patients to regulate their psychological status and improve their compliance, thereby promoting successful rehabilitation. However, previous routine care has some limitations, such as the empirical nursing measures and the neglect of individual circumstances. Comfort care based on the collaborative care model (CCM) proposes targeted comfort care according to the specific circumstances of patients, which can not only improve the quality of care, but also improve their physical, mental, and emotional status compared with routine care. However, its clinical application in CHD patients remains controversial. In this study, 104 CHD patients were selected to explore the value of comfort care based on the CCM, and in particular the effect on patient compliance and self-care ability.
We present the following article in accordance with the CONSORT reporting checklist (available at http://dx.doi.org/10.21037/apm-20-2520).
Methods
General data
A total of 104 CHD patients were randomly selected in our hospital between April 2019 and April 2020. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Taizhou People’s Hospital (No.: KY-2020-215-01).The inclusion criteria were as follows: (I) patients that met the diagnostic criteria for CHD according to the Guidelines for the Diagnosis and Treatment of Coronary Heart Disease (3), and confirmed by clinical manifestations, electrocardiography (ECG), and other examinations; (II) patients that were in classes II–IV according to the New York Heart Association (NYHA) Functional Classification (4); (III) patients that signed the informed consent. The exclusion criteria were as follows: (I) patients with visual disturbance, dysaudia, or comprehension obstacles; (II) patients with severe mental illnesses; (III) patients with severe organ diseases or malignant tumors;
Care methods
The control group received routine care (which lasted for 2 weeks), mainly by the on-duty nurses according to the relevant regulations. The specific contents were as follows: nurses closely observed the condition of the patients, assisted them to complete examinations, gave verbal education on the disease, comforted patients that appeared to be struggling with adverse psychological impacts, guided patients to take medicine regularly and quantitatively according to the doctor’s instructions, guided patients to maintain a reasonable diet, and assisted them with exercise.
The study group received comfort care based on the CCM, which also lasted for 2 weeks, while simultaneously receiving routine care. The specific contents were as follows.
Establishing a group for comfort care based on the CCM
The group members included a head nurse, a supervising nurse, a primary nurse, a psychologist, a dietitian, and a rehabilitation therapist. The head nurse, as the group leader, regularly arranged for group members to undergo training on the knowledge of CHD, and the content and process of comfort care based on the CCM, which required proficiency. After the patients were admitted to hospital, the group of healthcare professionals comprehensively understood their basic situation and analyzed the causes of their discomfort, including physical discomfort caused by clinical symptoms; mental discomfort caused by fear of the disease, surgery, and treatment costs; as well as social and emotional discomfort caused by the lack of family members accompanying them, loneliness, decreased self-care ability, and inferiority. The targeted comfort care plan was developed specifically according to these circumstances.
Physical comfort care
The patients were promptly asked whether they were experiencing physical symptoms, in order to help them reduce or eliminate this source of discomfort. The patients were provided with safe and comfortable wards and were allowed to place personal items to create a family atmosphere according to their own preferences without influencing the medical and nursing work. Clean-smelling air freshener was appropriately applied to reduce patient discomfort with the smell of the hospital environment. Personalized diet plans were developed for the patients with the cooperation of the dietitian in order to reduce discomfort caused by an unreasonable diet and ensure adequate nutritional intake to enhance immunity. The patients were helped to perform postural adjustments, limb massage, passive mobilization, as well as ambulation to improve physiological comfort with the cooperation of the rehabilitation therapist.
Mental comfort care
The sense of trust and security of the patients was improved by active communication, skillful technique, methodical nursing, and the mild attitude of the nurses. The mental status of the patients was assessed to analyze the causes of their mental discomfort with the cooperation of the psychologist. For example, patients with mental discomfort caused by a lack of awareness of the disease were flexibly given various forms of health education according to their age, education level, and cognitive level, such as one-on-one education, video education, and education using the WeChat platform. In this way, the health knowledge requirements of patients at different levels were met, and they could correctly understand the disease and its treatment. Patients with mental discomfort due to concerns about rehabilitation were introduced to other rehabilitation patients in addition to providing health education. If necessary, rehabilitation patients with the same disease would share their own experiences.
Emotional comfort care
The personal beliefs and philosophies of life of the patients needed to be respected. They were guided to actively face the disease and adhere to their own beliefs in this process to gain emotional satisfaction. Also, patients that shared the same hobbies or beliefs were encouraged to communicate with each other and to perceive the value of life.
Social comfort care
The nurses communicated with the patients as their families would and provided care services with the cooperation of the psychologist. The staff actively contacted the family members of patients to introduce and guide them in providing physical care correctly so as to relieve the discomfort of the patients. The family members were informed that it was important for the patients to maintain positive emotions, and so the families avoided expressing negative emotions in front of the patients, and refrained from accusing or ignoring them. Furthermore, social volunteers also provided care services to the patients, so that they could feel valued and understood, so as to avoid disconnection with society.
Observation indicators
The following indicators were observed: (I) a self-made questionnaire was used to investigate the health knowledge proficiency in the two groups both before and after intervention (treatment + care). The questionnaire included knowledge of the disease and its treatment, rational drug use, regular diet, psychological adjustment, and exercise, and was scored from 0 to 100, with higher scores indicating a better health knowledge proficiency; (II) the Self-Rating Anxiety Scale (SAS) and Self-Rating Depression Scale (SDS) (5) were used to assess the psychological status in the two groups before and after intervention. Each scale contained 20 items, with each items scored on a scale of 1–4. The final score = the sum of each item score × 1.25. A final score of SAS ≥50 is considered to signify anxiety, with higher scores indicating more severe anxiety. Similarly, a SDS ≥53 is considered to denote depression, with higher scores reflecting more severe depression; (III) a self-made questionnaire was used to investigate the compliance in the two groups following intervention, including drug compliance, reasonable diet, exercise, maintaining emotional stability, and regular examination. A score of ≥90 was considered as complete compliance, ≥65 and <90 as partial compliance, and <65 as non-compliance. The compliance rate = complete compliance rate + partial compliance rate; (IV) the Exercise of Self-Care Agency (ESCA) scale (6) was used to evaluate the self-care ability of the two groups before and after intervention. It included 43 items covering four main aspects: self-care skills, self-care responsibility, self-concept, and health knowledge level. Each item was scored between 1 and 4, with higher scores indicating a better self-care ability; (V) a self-made questionnaire was used to investigate the comfort degree in the two groups after intervention, and involved physical, mental, social, and emotional comfort. Each of these aspects was scored between 0 and 10, with higher scores indicating a higher comfort degree.
Statistical analysis
Statistical analysis was performed using SPSS 25.0 software (IBM Corporation, Amonk, NY, USA). Measurement data were statistically expressed as mean ± standard deviation (SD), and the differences between the groups were compared using the chi-square test. Enumeration data were expressed as frequency (n) and percentage (%), and the differences between the groups were compared using the t-test. P<0.05 was considered statistically significant.
Results
Patient characteristics
A total of 104 CHD patients were randomly divided into a control group (n=52) and a study group (n=52). In the control group, there were 32 males and 20 females aged between 50 and 78 years, with an average age of 63.02±5.24 years. This included 18 cases in the NYHA class II, 20 cases in class III, and 14 cases in class IV. The disease course of patients in this group was between 6 months and 4 years, with an average of 2.04±0.95 years. In the study group, there were 30 males and 22 females aged between 51 and 79 years, with an average age of 63.15±5.31 years. This included 19 cases in the NYHA class II, 22 cases in class III, and 11 cases in class IV. The disease course of patients in this group was between 6 months and 4 years, with an average of 2.08±0.91 years. The baseline data of the two groups exhibited homogeneity (P>0.05) (Table 1).
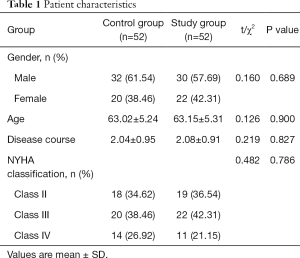
Full table
Health knowledge proficiency
Health knowledge proficiency was compared between the two groups following intervention (Table 2). The post-intervention scores were higher in both groups compared to the pre-intervention scores (P<0.05). Meanwhile, the score in the study group was significantly higher than that of the control group after intervention (P<0.05).
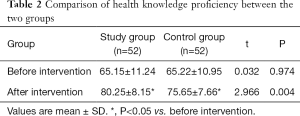
Full table
Psychological status
SAS and SDS scales were used to assess the psychological status of the two groups before and after intervention (Table 3). The post-intervention scores of both groups were lower compared to the pre-intervention scores (P<0.05). Meanwhile, the score in the study group was markedly lower than that of the control group after intervention (P<0.05).
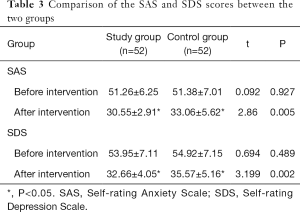
Full table
Compliance of the patients
The compliance of the CHD patients was compared between the two groups before and after intervention (Table 4). The compliance in the study group was 96.15%, which was significantly higher than the control group (82.69%) (P<0.05).
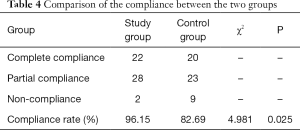
Full table
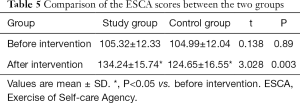
Self-care ability
The ESCA scale was used to evaluate the self-care ability of the two groups before and after intervention (Table 5). The post-intervention ESCA scores of both groups were higher compared to the pre-intervention scores (P<0.05). Meanwhile, the score in the study group was higher than that of the control group (P<0.05).
Full table
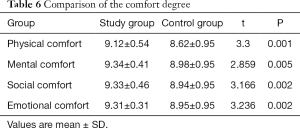
Comfort degree
After intervention, the physical, mental, social, and emotional comfort scores in the study group were higher than those of the control group (P<0.05) (Table 6).
Full table
Discussion
CHD is a common cardiovascular disease with a high mortality rate. Without timely treatment, CHD will cause complications such as arrhythmia and angina pectoris (7). This disease, which has a long course as well as complex and severe symptoms, brings significant physical and mental discomfort to patients (8). Moreover, recurrence of CHD is common. Most CHD patients are middle-aged and elderly, and lack knowledge about the disease and its treatment, as well as the ability for self-care. In addition, fear of the disease, surgery, and treatment costs often leads to psychological impacts including anxiety, dysphoria, and depression, which ultimately affect patient compliance and rehabilitation (9).
At present, it is believed that strengthening nursing cooperation with CHD patients during clinical treatment is important for improving prognosis and rehabilitation (10,11). In the past, routine care was often applied in a clinical setting primarily by a nurse and according to a doctor’s instructions. However, this mode of care has limitations, including the limited ability of nurses, empirical measures, and neglect of the patient’s psychological state. Compared with routine care, CCM gives considerable weight to the synergistic effect of nurses, psychologists, dietitians, and rehabilitation therapists to provide more comprehensive and objective nursing services for patients (12,13). Comfort care emphasizes the importance of improving the patients’ physical, mental, and emotional states, in addition to other aspects, in order to enhance the prognosis (14,15). In recent years, comfort care based on the CCM has gradually attracted attention, however there are only few clinical studies regarding its application in CHD patients. In this study, comfort care based on the CCM was applied in the study group, and the following values were identified.
Comfort care based on the CCM improved the health knowledge proficiency of CHD patients
In this study, the proficiency in the study group was significantly higher after intervention, which indicated that the application of this care approach was beneficial to improving the health knowledge proficiency of the patients. The reasons for this outcome are as follows. Firstly, comfort care based on the CCM embraces collaborative nursing on the basis of a comprehensive analysis of the influencing factors of patient discomfort, and thus, the nursing measures were more targeted. Secondly, it applies various forms of health education to meet the needs of patients at different levels, thereby improving their health knowledge proficiency. In contrast, routine care only applies verbal education.
Comfort care based on CCM improves the psychological status of CHD patients
In this study, the SAS and SDS scores in the study group were lower than those of the control group after intervention, which is consistent with the results reported by Qian (16), indicating that the application of this care regulated the psychological status of the patients. This is because comfort care based on the CCM not only focuses on physical comfort, but also on the mental, emotional, and social comfort of patients. Firstly, with the participation of psychologists, nurses have a deeper understanding of the psychological needs and mental discomfort of patients, and are therefore able to implement targeted measures. Secondly, the emotional and social supports are strengthened using this approach, which helps patients regulate their psychological status and enhance their confidence (17,18).
Comfort care based on the CCM improves the compliance of CHD patients
In this study, the compliance rate in the study group was 96.15%, which was higher than that of the control group (82.69%), indicating that the application of this mode of care improved the compliance of CHD patients. This is because it helps patients correctly understand the disease and improve their health knowledge. It also regulates their psychological status and changes their attitude to consciously standardize their behavior, so as to effectively improve compliance.
Comfort care based on CCM improves the self-care ability of CHD patients
In this study, the ESCA score in the study group was higher than that of the control group after intervention, which indicated that the comfort care approach improved the self-care ability of CHD patients. This is because it promotes correct understanding of the disease, as well as its treatment and nursing; reduces the physical, mental, social, and emotional discomforts in patients; and improves their compliance. Therefore, patients consciously develop healthy behaviors and participate in the treatment and nursing, thereby effectively improving their self-care ability.
Comfort care based on CCM improves the comfort of CHD patients
In this study, the physical, mental, social, and emotional comfort scores in the study group were higher than those of the control group after intervention, which indicated that this mode of care improved the comfort of CHD patients. This is because it includes various nursing services and strengthens physical, mental, emotional, and social comfort care on the basis of a comprehensive analysis of the discomforts of individual patients and their causes. Therefore, it can better meet the needs of patients and reduce or eliminate the factors causing discomfort, thus effectively improving their overall comfort (19-21).
In summary, comfort care based on the CCM can improve patients’ health knowledge proficiency, regulate their psychological status, and improve their compliance, self-care ability, and comfort. Its application in CHD patients is important and is worthy of in-depth study. However, there are still some shortcomings in this study. The sample size of the study is small and insufficient. It needs to be promoted on a larger scale, as well as large-scale investigation and analysis. How to apply the CCM model to practical work needs further research.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-2520
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-2520
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-2520). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Taizhou People’s Hospital (No.: KY-2020-215-01). Written informed consent was obtained from the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kurniawati ND, Nursalam N, Suharto S, et al. Development of the Mind-Body-Spiritual (MBS) Nursing Care Model for Coronary Heart Disease Patients. 2019.
- Duan X. Analysis of the comprehensive nursing care effect for patients with coronary heart disease undergoing selective coronary angiography and stent implantation by radial artery. Chinese Community Doctors, 2018. Available online: http://en.cnki.com.cn/Article_en/CJFDTotal-XCYS201813089.htm
- Jin K, Khonsari S, Gallagher R, et al. Telehealth interventions for the secondary prevention of coronary heart disease: A systematic review and meta-analysis. Eur J Cardiovasc Nurs 2019;18:260-71. [Crossref] [PubMed]
- Coronary Heart Disease (CHD). In: Gellman MD, Turner JR, editors. Encyclopedia of Behavioral Medicine. New York, NY: Springer New York, 2013.
- Jokanovic N, Kautiainen H, Bell JS, et al. Change in Prescribing for Secondary Prevention of Stroke and Coronary Heart Disease in Finnish Nursing Homes and Assisted Living Facilities. Drugs Aging 2019;36:571-9. [Crossref] [PubMed]
- Bayrak B, Oğuz S. Validity and reliability of the Turkish version of the Self-Care of Coronary Heart Disease Inventory. Int J Nurs Pract 2020;e12847. [Crossref] [PubMed]
- Brown CW, Alexander DS, Cummins K, et al. STEPS to a Healthier Heart: Improving Coronary Heart Disease (CHD) Knowledge Among African American Women. Am J Health Edu 2018;49:57-65. [Crossref]
- Ammouri AA, Abu Raddaha AH, Tailakh A, et al. Risk Knowledge and Awareness of Coronary Heart Disease, and Health Promotion Behaviors Among Adults in Oman. Res Theory Nurs Pract 2018;32:46-62. [Crossref] [PubMed]
- Kähkönen O, Saaranen T, Kankkunen P, et al. Predictors of adherence to treatment by patients with coronary heart disease after percutaneous coronary intervention. J Clin Nurs 2018;27:989-1003. [Crossref] [PubMed]
- Wu D, Wang Z, Ni W. Information technology based transitional care for patients with coronary heart disease after PCI. Available online: http://en.cnki.com.cn/Article_en/CJFDTotal-HLXZ201801007.htm
- Haq N, Sajjad B, Nasim A, et al. Determination of Health Related Quality of Life in Coronary Heart Disease (CHD) Patients Attending Different Hospitals in Quetta, Pakistan. Value Health 2017;20:274.
- Yan J. Value of Cognitive Behavioral Intervention in Nursing Patients with Coronary Heart Disease. Available online: http://en.cnki.com.cn/Article_en/CJFDTotal-YJZY201935029.htm
- Wang F. Application effect of personalized nursing intervention in the nursing of elderly patients with coronary heart disease. Available online: http://www.en.cnki.com.cn/Article_en/CJFDTotal-ZGUD201828063.htm
- Lu Z. Analysis of the Nursing Methods and Effect of Patients with Coronary Heart Disease in Intensive Care Unit. Available online: http://en.cnki.com.cn/Article_en/CJFDTotal-SLYY201903069.htm
- Ding Y, Tian M. The Effect of Diversity Nursing on the Nursing of Patients with Diabetes Mellitus Complicated with Coronary Heart Disease. Available online: http://en.cnki.com.cn/Article_en/CJFDTotal-ZHJK201913072.htm
- Qian J. Effect of Time Nursing on Coronary Heart Disease Complicated With Hypertension. China health standard management, 2019. Available online: http://en.cnki.com.cn/Article_en/CJFDTotal-WSBZ201908069.htm
- Tang Z. Application of Seamless Nursing Care in Senile Patients with Coronary Heart Disease and its Influence on Angina Pectoris and Disease Cognition. Available online: http://en.cnki.com.cn/Article_en/CJFDTotal-LCYN201901094.htm
- Kang L. Application Effect of SeamLess Nursing in Elderly Patients with Coronary Heart Disease. Available online: http://en.cnki.com.cn/Article_en/CJFDTotal-ZHJK201928059.htm
- Yu T, Tan Y, Shi L, et al. Effect of Comfortable Nursing on Anxiety and Quality of Life in Patients with Coronary Heart Disease after Stent Implantation. Available online: www.en.cnki.com.cn/Article_en/CJFDTotal-HZZZ201803057.htm
- Tian M, Ding Y. Application Analysis of Humanized Nursing Intervention in Patients with Coronary Heart Disease. Available online: http://en.cnki.com.cn/Article_en/CJFDTotal-ZHJK201914072.htm
- Li L, Jiang Y, Zhou Y, et al. Impact of Continuous Nursing on Angina Pectoris for Patients with Coronary Heart Disease: A Meta-analysis. Available online: http://en.cnki.com.cn/Article_en/CJFDTotal-WMIA201986009.htm
(English Language Editor: A. Kassem Kassem)


