
The effect of the integrated delivery system on managing hypertension in rural areas of China
Introduction
Managing the high incidence, high disability, and high cost of chronic diseases has become a global problem. Hypertension is an important chronic disease, which has always attracted attention from specialists. The development of the social economy in China, along with changes in lifestyle, especially the rate of aging and urbanization, have led to a continuous rise in hypertensive patients in China. Moreover, the direct medical costs for high blood pressure and treatment costs of cardiovascular disease, which is the complication caused by hypertension, have rapidly increased. Research has found that approximately one-third of the adult population has hypertension, and the prevalence increases steeply with age. Furthermore, the control of blood pressure has been shown to be lower among patients with lower levels of education and income (1). The medical service provided by the clinic does not meet the national health requirements, and the lack of primary health care pharmacy impacts the health of patients (2). Therefore, the emergence of a new medical service system provides an essential contribution to chronic disease management in China’s rural areas.
China’s new medical reform puts forward the short-term goal of “effectively reducing the burden of residents’ medical expenses, effectively alleviating the difficulty and cost of medical treatment”, and the long-term goal of “establishing and improving the basic medical and health system covering urban and rural residents, and providing safe, effective, convenient and cheap medical and health services for the masses.” Since the new medical reform began in 2009, China has established a unified basic medical insurance system covering urban and rural residents, dynamically revising the catalog of basic drugs, improving the basic medical and health care service system, and gradually promoting equalization of essential public health services.
At the national level, it has been repeatedly highlighted that the construction of medical consortia based on the four categories is a specific exploration into the integration of medical services in China, and forms an important part of promoting the establishment of a reasonable and orderly hierarchical diagnosis and treatment mode (3). The integrated delivery system plays an essential role in the medical reform of China. It is an important research topic and trend in health reform across the world to establish an integrated medical service system aimed at improving the quality of medical service and reducing the cost of medical treatment. Previous research has demonstrated that integrated delivery systems can be a source for assessing opportunities to improve patient outcomes, and lower costs for chronic pain patients (4).
Huzhou No.1 Hospital (the Affiliated Hospital of Huzhou University) stands on the South Bank of the Taihu Lake. Founded in 1923, it is the earliest Western Hospital in Huzhou City, and is a comprehensive tertiary hospital integrating medical treatment, prevention, scientific research, teaching, and rehabilitation in Northern Zhejiang Province. It has realized an integrated medical service system of “first-line direct access, full-coverage, and continuity of service” at the city, district, and township levels.
At the same time of the new national medical reform, the medical community was established in Huzhou No.1 Hospital in July 2014. We established an integrated medical and health service system with “Regional Medical Center + basic medical group” as the main body. The city’s tertiary hospitals take the lead in setting up a city medical community covering the district’s secondary hospitals and six township hospitals, to realize the unified management of people and property. We aimed to establish different types of district medical and health institutions, and vertically integrate and coordinate all kinds of medical institutions at all levels to provide all-around life-cycle services for patients’ health needs. Among them, the matrix chronic disease management platform is our primary tool for managing chronic non-infectious diseases, forming a “tertiary hospital—secondary hospital—community health service center” patient hierarchical management mode and a professional team of “specialist, specialist nurse, and general practitioner.” The platform helped us screen for the high-risk population in the community, and facilitate further diagnosis in tertiary hospitals with the specialist. It also helped in developing the treatment plan and adjusting the prescription. The patient was then transferred to the community health service center after their condition was stable, and the contracted team of “specialist—specialist nurse—general practitioner” arrived at the community health service center to regularly to carry out diagnosis, treatment services, and health management. In cases of unstable conditions (new complications or aggravation of original complications), a referral was made. The secondary hospital not only establishes files for all patients with chronic diseases, but the members of the health management team monitor the indicators of patients in the whole process, as well as provide online and offline preventive health care and hierarchical diagnosis and treatment services for patients so that patients can acquire closed-loop management before, during and after their hospital stay. Meanwhile, as an intermediary, secondary hospitals also have the responsibilities of monitoring and evaluating the work of medical staff in the community health center.
In this study, we analyzed the medical expenses, actual reimbursement rates, and medical behaviors of hypertensive patients diagnosed in Zhili town during 2014–2019 across different levels of medical institutions to understand the impact of the integrated delivery system on the management performance for patients with hypertension.
We present the following article in accordance with the MDAR checklist (available at http://dx.doi.org/10.21037/apm-20-2489).
Methods
Study population
On 1 January 2014, 7,037 patients with hypertension were identified in the Zhili Town Health Center’s hospital information system. Patients were selected if they met the following criteria: (I) hypertension was diagnosed according to the Guidelines for Prevention and Treatment of Hypertension in China (5); (II) blood pressure did not reach the control target (140/90 mmHg); (III) simple hypertension without other complications; (IV) aged between 36 and 99 (including 36 and 99 years old). Before and during the tracking research, those who met one of the following criteria were excluded: (I) patients with secondary hypertension; (II) patients with serious diseases, whose life expectancy was less than one year; (III) patients who had difficulty cooperating (obvious impairment of intelligence, hearing, and limb activity); (IV) patients who were not willing to participate in the project; (V) myocardial infarction (<3 months) and stroke (<3 months) in the acute stage.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Zhili Town Health Center’s Hospital of No.20170118004 and informed consent was taken from all individual participants.
Exposure
The hospital information system of Zhili Town Health Center investigated and recorded the ID numbers of the research subjects, and extracted the data pertaining to medical treatments from 1 January 2014 to 31 December 2019 through the database of Huzhou Medical Security Bureau (6). This included baseline information such as age, gender, medical insurance type, the insured units of all the research subjects, as well as all the outpatient and inpatient information in the four-year medical records, including the information of the hospital, the level of the hospital, and the successive medical expenses. Financial information was obtained from the relevant documents of the Huzhou Human Resources and Social Security Bureau (7), and the Huzhou Finance Bureau (8).
Statistical analysis
After obtaining the data, SPSS 22.0 was used for statistical analysis. Since the distribution of expenses was not normal, the median m (interquartile interval q) was used to describe expenses. The Kruskal-Wallis H test was used to compare and analyze the differences in expenses between different years and different medical institutions. The Kruskal-Wallis single factor ANOVA test was used to compare the two groups, and P<0.05 was considered statistically significant.
Results
General information of the subjects
In 2014, there were 99,982 residents under the jurisdiction of Zhili Town Health Center in Wuxing District, Huzhou, China, and 5,460 of them were selected as the subjects for the follow-up cohort study. There were no clinical differences in race, ethnicity, or type of insurance in the cohort. Of the 5,460 patients with hypertension, 2,559 (46.87%) were male, and 2,901 (53.13%) were female, and the ratio of males and females was balanced. The average age of the participants was 68.96±9.87 years. The average disease course of the 5,460 hypertensive patients was 6.7±2.6 years.
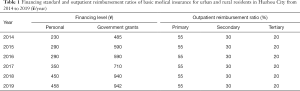
Reimbursement ratios of the different medical institutions
Table 1 shows the financing standard of basic medical insurance for urban and rural residents in Huzhou City from 2014 to 2019. The individual financing level and government subsidies increased year by year. The reimbursement ratios of basic medical insurance for urban and rural residents at different levels of medical institutions did not change, including 55% for primary hospitals, 30% for secondary hospitals, and 20% for tertiary hospitals.
Full table
Trends in medical expenses for patients with hypertension
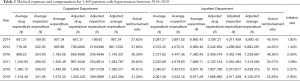
Table 2 shows the average total expenditure including drug costs, inspection costs, and other indirect costs (the costs of losing wages, transportation, eating, etc.). In this study, we only focused on drug costs and inspection costs, which comprised a large proportion of patients’ expenses. As for the outpatient department, they faced increasing expenses for both drugs and inspection, but drug costs took up a larger proportion than inspection costs. The actual reimbursement ratio rose for the outpatient department from 2014 to 2019, as well as hospitalization. Inpatient costs accounted for most of the costs for patients with hypertension, although the reimbursement ratio was higher than the outpatient department, in which inspection expenses comprised the majority.
Full table
Inflation is a necessary factor that needs to be considered when comparing time-series data. The inflation rate is generally considered to be the rise in the average price (subject to inflation). The inflation rate causes a significant change in the system’s operating costs, and consequently, a change in the economic efficiency index (9). Consumer price index (CPI) is a macro-economic index that reflects the price level changes of consumer goods and services purchased by households in general. It is the price index that can adequately and comprehensively reflect the inflation rate. According to the data from the National Bureau of Statistics of China (10), we obtained the adjusted medical expenses and compensation for 5,460 patients with hypertension between 2014–2019. We used 2014 as the base year. The adjusted data illustrated different results than the previous one, however, they had roughly the same trend.
From 2014 to 2019, all the expenses for hypertensive patients increased more slowly, and in 2019, there were some reverse trends for the expenditure on drugs in the outpatient and inpatient departments, as well as the average inspection expenses and average expenses for hospitalization. After taking into account the inflation rate of China, it was clearly observed that the platform at our hospital had positive effects on reducing the financial burden of patients with hypertension. The light blue part in Table 2 shows the medical expenses after adjusting for the inflation rate from 2014 to 2019. The apparent differences between the two tables were the average drug expenses for the outpatient and inpatient departments. Although the total expenses were rising, the drug expenses for our hospital’s patients decreased slightly from 2018, which demonstrated the impact of our platform in drug-expense control.
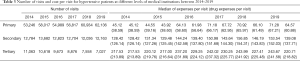
Number of visits and cost per visit
From 2014 to 2019, the average cost per visit increased, as shown in Table 3. The average annual number of patients in the tertiary hospitals showed a decreasing trend, while the number of patients in the community health center (primary hospital) showed an increasing trend. Nevertheless, for the annual number of visits to secondary hospitals, it became stable. This might be because we only used the secondary hospitals as transfer stations that connected the primary and tertiary hospitals together, as well as the staff working there. Patients with hypertension became more willing to visit tertiary hospitals than before, after our platform had formed. On the other hand, the average cost per visit of the tertiary hospitals was significantly higher than that of the primary and secondary hospitals. This could be another reason behind patients changing their usual medical behavior to visit tertiary hospitals. Drug costs comprised a dramatically high proportion of patients’ expenses.
Full table
The light blue block in Table 3 shows the total and drug costs adjusted for the inflation rate, which treated 2014 as the base year. After considering the inflation rate, patients’ expenses per visit in primary hospitals showed a more obvious decreasing trend, as well as the drug expenses per visit. For the secondary hospitals, the expenses were still stable in Table 4. However, the expenses per visit decreased from 2018 in tertiary hospitals after taking into account the inflation rate, which was earlier than shown in the former table.
Full table
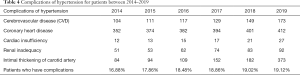
Complications of hypertension
The complications of hypertension listed in Table 4 are not a complete list, but were the complications our participants experienced during the research period from 2014 to 2019. Cerebrovascular diseases and coronary heart disease comprised the highest proportion of complications, and rose gradually. Cardiac insufficiency took up a small proportion of the complications of hypertension. Renal inadequacy was also a possibly acquired complication for patients with hypertension. Intimal thickening of the carotid artery can be hard to detect, but from 2019, a significant amount of attention was paid to this disease, resulting in numbers increasing dramatically. From 2014 to 2019, the total number of complications increased due to the increases of count of disease and more detailed examinations, which also explained the rise of inspection costs from the former table. For the proportion of hypertensive patients who had complications, numbers rose slightly, demonstrating the positive effect of our platform.
Patient satisfaction and utility
To directly understand the feelings of both patients and doctors towards our matrix chronic disease management platform, we sent questionnaires to them and obtained answers. Our platform not only optimizes the outcomes of the whole system, but also improves health care in the community health service center. Therefore, what the patients and doctors in the community center think was the standard we wanted to assess. Participant satisfaction was defined as the extent to which the participants were pleased with their experience in hospital (11). We sent 1,000 questionnaires (Appendix 1) to patients and 300 questionnaires to the doctors in the primary hospitals. We asked 5 questions in each questionnaire, and received 729 back from patients and 127 back from doctors. Each question was assigned 20 scores (in the questionnaire, we used 1–5 to represent bad-good, but we multiplied by 4 to get the final percentage of satisfaction), and the total score was 100. Figure 1 illustrates the results, in that the average degree of satisfaction of the patients and doctors in primary hospitals both increased after we established the matrix platform. According to the results from the questionnaires, our platform achieved preliminary success, as the degree of satisfaction was high for both the patients and doctors in the primary hospitals.
Discussion
With the acceleration in social and economic transformation, such as the aging and urbanization of the population, the basic health needs of the population are multiplying and diversifying, which is conducive to the establishment and improvement of the basic medical and health service system. The basic medical service system of the tertiary hospital mainly manages common diseases, and many diagnostic and treatment services. It not only uses a large number of high-quality medical resources, but also causes inconvenience for residents to see a doctor, and increases the burden of medical expenses, which is not conducive to fundamentally solving the problem of “difficult to see a doctor, expensive to see a doctor”.
Although evidence has shown that China has improved its control of hypertension, hypertension remains one of the most important preventable contributors to disease and death (12,13). The awareness, treatment, and control rates of hypertension have improved significantly, and the increasing prevalence, reducing urban-rural disparities, and changing geographical distribution patterns of the hypertension epidemic reflect dynamic changes over time (14). Compared with the independent medical facilities, the integration of medical institutions can make the system meet the same level of need with less capacity through coordinated actions. Through joint action, better capital access and economies of scale will lead to lower operating costs and lower medical costs for patients. This paper therefore analyzed the effect of the matrix chronic disease management platform on the integrated delivery system in Zhili, Huzhou.
In our platform, we treated primary, secondary, and tertiary hospitals as one system, which reflects L Von Bertalanffy’s “antibody system theory” from 1932 (15). In 1937, the general system theory was put forward, which laid the theoretical foundation of this science. It posits that each element in the system does not exist in isolation. Each element is in a particular position in the system and plays a specific role. The elements are interrelated and form an indivisible whole. An element is therefore an element of the whole. If an element is separated from the whole system, it will lose its function as an element. For our platform, primary, secondary, and tertiary hospitals were treated as a whole, and they all formed indispensable parts of our platform. Different levels of hospitals were related to each other, and played a specific role. The new nature and function of “the whole is greater than the sum of its parts” and “1+1>2” was formed by the interaction of each element in the system. We aim to make the system reach optimization by adjusting the system structure and coordinating the relationship between various elements. Moreover, vertical coordination among primary, secondary, and tertiary health facilities has been established, which is a crucial strategy to optimize resource allocation, and to provide technical support and the shifting of resources to primary care health providers (16).
The average costs for hypertensive patients are increasing year by year in the outpatient and inpatient departments. Drugs account for most of the medical expenses in the outpatient departments, but the actual compensation ratio was also increasing. After adjusting the data for inflation, the average cost of patients, especially in inpatient departments, decreased in 2019, and the drug costs of outpatients also decreased. Under the new service system platform, the number of patients in tertiary hospitals decreased significantly, and the number of patients in community hospitals (primary hospitals) increased, while the number of patients in secondary hospitals has remained almost unchanged. This demonstrates the significant improvement in basic service capacity, and the effectiveness of the matrix chronic disease management platform. Furthermore, patient fees in hospitals across all levels also decreased during the study period. The main complications of hypertension were cerebrovascular disease and coronary heart disease, which were slightly increasing. The small increase in the proportion of patients with hypertension complications from 2014 to 2019 shows the positive role of our platform in controlling and managing complications.
The degree of satisfaction is also a critical assessment indicator to evaluate the effect of the platform. The continuous increasing trend in satisfaction of both the patients and doctors in the community health care center shows the advantages of the integrated delivery system in managing and facilitating hypertension treatment.
Utility refers to the ability of commodities to satisfy people’s desires, or the degree of satisfaction consumers feel when consuming commodities. Utility is a kind of subjective psychological evaluation that connects with peoples’ desires and consumers’ subjective psychological evaluations of the ability of goods to satisfy their desire. In health economics, utility function for patients can be more complicated, and is often hard to predict. Patients are willing to pay more for hypertension because they are risk averse. Therefore, even if the expenses were increasing in both the outpatient and hospitalization departments, they were still satisfied with the medical service. In order to reach our goal of getting more hypertensive patients visiting primary (community) hospitals rather than tertiary hospitals, improving the health service and quality may be a more effective method.
The reimbursement rate of medical insurance for primary diagnosis and treatment is generally higher than that of secondary and tertiary hospitals, and patients are encouraged to choose primary institutions. However, the lower reimbursement limit (top line) at the grass-roots level has objectively induced the behavior of visiting superior hospitals and needing unnecessary hospitalization. This makes it challenging to integrate and control the medical system. China should therefore aim to build a learning primary health care system that is data-driven and technology-enabled, and we should ensure that professionals are practicing at the top level of their training (17,18). The rural allowances should be added to the current salary system to improve the attraction and retention of the rural health workforce (19). The government should also pay more attention to the tight integration method by entrusting primary health institutions to hospitals (20).
Limitation
Zhili is a small district with a relatively high floating population, which makes it difficult to compile and obtain complete information for all patients on the hypertension database. When calculating costs, we only used direct costs, including drug and inspection costs, but there were some indirect costs we did not count. As mentioned before, the indirect costs include costs of losing wages, transportation, and eating, amongst others. Hypertension complications are caused by more factors beyond just hypertension, so precise assessment of hypertension complications requires additional clinical information (21). Some complications, such as arteriosclerosis of the retina, are not examined during regular inspection, so they are hard to detect. The complications of hypertension in this study were not only affected by our system and the policy. Lee et al. conducted analyses on the incidence of hypertension and hypertension complications using Cox regression as a variable selection method, and constructed Bayesian network topology to visualize the causal relationships between variables (22). Therefore, finding the proper data and algorithms will be the subject of future studies.
Conclusions
According to the 2014–2019 5-year data, the matrix chronic diseases management platform established under an integrated delivery system was effective for controlling and managing hypertension, serving patients with high blood pressure, and facilitating the work of the medical staff.
Acknowledgments
Funding: Key Research and Development Projects of Zhejiang Province in 2021. Counterpart Assistance Project – Research on the promotion and application of urban medical community system in medical and health cooperation between the East and the West.
Footnote
Reporting Checklist: The authors have completed the MDAR checklist. Available at http://dx.doi.org/10.21037/apm-20-2489
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-2489
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-2489). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Zhili Town Health Center of No.20170118004 and informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lewington S, Lacey B, Clarke R, et al. The burden of hypertension and associated risk for cardiovascular mortality in China. JAMA Intern Med 2016;176:524-32. [Crossref] [PubMed]
- Su M, Zhang QL, Bai XK, et al. Availability, cost, and prescription patterns of antihypertensive medications in primary health care in China: a nationwide cross-sectional survey. Lancet 2017;390:2559-68. [Crossref] [PubMed]
- Guidance of the national health and Family Planning Commission on the pilot work of the construction of medical consortia (No. 75). Available online: http://www.nhc.gov.cn/yzygj/s3594q/201701/4a39ec35c70a4899b3e415b51e821464.shtml. Accessed 23 January 2017.
- Park PW, Dryer RD, Hegeman-Dingle R, et al. Cost burden of chronic pain patients in a large Integrated Delivery System in the United States. Pain Pract 2016;16:1001-11. [Crossref] [PubMed]
- Guidelines for the prevention and treatment of hypertension in China (revised in 2018). Chinese Journal of Cardiology 2019;1:1-44.
- Huzhou Medical Security Bureau web site. Available online: http://ybj.huzhou.gov.cn/
- Huzhou human resources and Social Security Bureau web site. Available online: http://hrss.huzhou.gov.cn/
- Huzhou Finance Bureau web site. Available online: http://czj.huzhou.gov.cn/
- Walery M. The effect of inflation rate on the cost of medical waste management system. E3S Web of Conferences 2017; 22.
- Chineses Statistical Bureau web site. Available online: http://data.stats.gov.cn/easyquery.htm?cn=C01
- Zou P, Dennis CL, Lee R, et al. Hypertension prevalence, health service utilization, and participant satisfaction: Findings from a pilot randomized controlled trial in aged Chinese Canadians. Inquiry 2017;54:46958017724942. [Crossref] [PubMed]
- James PA, Oparil S, Carter BL, et al. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507-20. [Crossref] [PubMed]
- Cai G, Zheng Y, Sun X, et al. Prevalence, Awareness, Treatment, and Control of Hypertension in Elderly Adults with Chronic Kidney Disease: Results from the Survey of Prevalence, Awareness, and Treatment Rates in Chronic Kidney Disease Patients with Hypertension in China. J Am Geriatr Soc 2013;61:2160-7. [Crossref] [PubMed]
- Wang Z, Chen Z, Zhang L, et al. Status of Hypertension in China: Results from the China Hypertension Survey, 2012-2015. Circulation 2018;137:2344-56. [Crossref] [PubMed]
- Bertalanffy LV. General system theory: foundations, development, applications. 1973.
- Zhao R, Li YZ, Liu CP, et al. Effects of the Integrated Healthcare Delivery System on 270 pilot cities in 2016: a mixed methods study. Lancet 2017;390:S101. [Crossref]
- Li X, Krumholz HM, Yip W, et al. Quality of primary health care in China: challenges and recommendations. Lancet 2020;395:1802-12. [Crossref] [PubMed]
- Li X, Lu JP, Hu S, et al. The primary health-care system in China. Lancet 2017;390:2584-94. [Crossref] [PubMed]
- Liu XY, Zhao SC, Zhang MM, et al. The development of rural primary health care in China’s health system reform. Journal of Asian Public Policy 2015;8:88-101. [Crossref]
- Yuan SS, Wang F, Zhao Y, et al. Assessing perceived quality of primary care under hospital-township health centre integration: Across-sectional study in China. Int J Health Plann Manage 2020;35:196-209. [Crossref]
- Saxena R, Mehrotra V. Prediction of hypertension and cardiovascular disease risk in North Indian geriatric population: A conundrum of senescence. Int J Community Med Public Health 2014;1:18-23. [Crossref]
- Lee JH, Lee WJ, Park IS, et al. Risk assessment for hypertension and hypertension complications incidences using a Bayesian network. IIE Trans Healthc Syst Eng 2016;6:246-59. [Crossref]
(English Language Editor: C. Betlazar-Maseh)



