
Patients’ understanding of communication about palliative care and health condition in Japanese patients with unresectable or recurrent cancer: a cross-sectional survey
Introduction
Good communication is essential for informed decision-making among patients with unresectable/recurrent solid cancers, according to individuals’ stated goals, values and preferences. Communication about end-of-life care are associated with terminal illness acceptance, greater use of hospice care, and fewer aggressive treatment at the end of life (1,2). Moreover, previous studies reported that palliative care which aimed to improve the quality of life of patients significantly improves patients’ understanding of prognosis over time, which may impact decision making about care near the end of life (3,4). However, previous studies showed that patients with unresectable/recurrent cancers tended to have excessively optimistic perceptions about their curability (1,5-7). Physicians often have difficulty delivering bad news and tend to deliver optimistic messages to patients with unresectable/recurrent cancer (8-15). Thus, patients with unresectable/recurrent cancer may believe that cure is possible even if they are in serious condition. Although several previous studies focused on patients’ misunderstanding of treatment goals, few studies have examined the gap between patients’ level of understanding and doctors’ explanations.
Previous studies reported that patients typically want physicians to provide adequate information that is straightforward and understandable (16). Therefore, this study aimed to examine agreement between patients’ and physicians’ reports of communication about palliative care and current health condition among patients with unresectable/recurrent cancer and explore factors associated with optimistic understanding in Japan.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-2045).
Methods
Study design
This study was a cross-sectional, multicenter, observational study in Japan. Between February 2015 and January 2016, patients with unresectable/recurrent solid cancers who were treated at Tohoku University Hospital and Miyagi Cancer Center were included. The researcher checked the medical record and asked physicians to enroll both inpatients and outpatients. Because the number of researchers was limited, we skipped enrollment when we identified several eligible patients on the same day at two hospitals. In addition, although we tried to enroll patients consecutively, however, in the specific periods when the research was not performed due to practical reasons, e.g., unavailability of researchers on certain days of the week, over the weekends or holidays or due to staff rotations, we allowed each institution to skip patient enrollment for the specific periods and the numbers of the patients were recorded. Therefore, patients were enrolled by convenience.
The primary responsible physician was defined as the medical oncologist who most frequently examined the patient. The primary responsible physician who provided care and communication obtained informed consent from patients. After informed consent was obtained, we immediately asked each primary responsible physician to complete the questionnaires about the explanations provided to their patients, and their approach about the explanations.
This study was conducted in accordance with the ethical standards of the Helsinki Declaration and the ethical guidelines for medical and health research involving human subjects presented by the Ministry of Health, Labour and Welfare in Japan. The primary responsible physicians obtained written informed consent from all patients in both Tohoku University Hospital and Miyagi Cancer Center. The patients were asked to complete and send survey questionnaires to our office. The study obtained approvals by the local Institutional Review Boards of all participating institutions. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The primary responsible physicians obtained written informed consent from all patients in both Tohoku University Hospital and Miyagi Cancer Center. The independent ethics committee of Tohoku University School of Medicine (approval No. 2014-1-085) and Miyagi Cancer Center (approval No. 2014-010) approved this study.
Patient survey
The inclusion criteria of this study were (I) patients with unresectable/recurrent solid cancer, (II) patients with failure of first-line chemotherapy and (III) adult patients (age ≥20 years). The exclusion criteria of this study were (I) patients who declined to provide written informed consent, (II) patients who exhibited cognitive impairment, (III) patients who had no image-confirmed lesion, (IV) patients who had not been informed about their disease, (V) patients who could not understand the Japanese questionnaire, (VI) patients who did not have sufficient strength to complete the questionnaire or (VII) patients who were deemed ineligible by the primary responsible physician. These exclusion criteria were applied by the primary responsible physician or queried via medical records.
To examine the proportion of agreement between patients’ recollection and physicians’ explanation, we asked patients about palliative care and current health condition.
First, patients were asked about palliative care. We defined palliative care (4,17) as (I) an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, (II) the treatment of pain and other problems, physical, psychosocial and spiritual, (III) the care provided at own home, palliative care units and hospices. Patients were asked following question about palliative care: “Have you talked with your doctor about palliative care?”. Response options were: “We discussed the option of receiving palliative care at home, in palliative care wards, hospice, etc., without chemotherapy”, “We talked about palliative care being generally available in palliative care wards and at home”, “We discussed the option of a specific palliative care ward or a doctor who conducts home visits” and “We did not discuss this topic”.
Second, patients were asked the following question about their current health condition: “How would you describe your current health condition?”. Response options were: “Serious and incurable”, “Serious, but curable”, “Good and curable” and “I don’t know”.
In addition to survey data, we obtained patient characteristics, including age, sex, type of cancer, name of the primary responsible physician and number of chemotherapy regimens, from medical records. We inquired about patients’ educational level, marital status, family income, European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30 (EORTC QLQ C30) score and communication score [physician communication (18)] via questionnaire. Regarding EORTC QLQ C30 score, we calculated the score based on the EORTC QLQ-C30 scoring manual (19). For communication score, patients were asked following five questions: “How often did your doctors listen carefully to you?”, “How often did your doctors explain things in a way you could understand?”, “How often did your doctors give you as much information as you wanted about your cancer treatments, including potential benefits and side effects?”, “How often did your doctors encourage you to ask all the cancer-related questions you had?” and “How often did your doctors treat you with courtesy and respect?”. Response options for each question were “Always (score 3)”, “Usually (score 2)”, “Sometimes (score 1)” and “Never (score 0)”. We converted the total scores (0–15) to 100-point scales, multiplying by 100/15, with 0 representing the worst possible communication and 100 representing optimal communication. Furthermore, we solicited patients’ Eastern Cooperative Oncology Group performance status (ECOG PS) from the primary responsible physicians.
Physician survey
Immediately after patient registration, the primary responsible physicians completed the questionnaires regarding communication about palliative care, overall health condition and survival prediction.
First, the physician was asked about palliative care: “Have you talked with the patient about palliative care?”. Response options were: “Yes. We discussed the option of receiving palliative care without chemotherapy”, “Yes. We discussed choices about places to receive palliative care”, “Yes. We discussed the specific place the patient wanted to receive palliative care” and “Didn’t discuss”.
Second, the physician was asked a question about the patient’s current health condition: “How did you explain the patient’s current health condition?” Response options were: “Serious and incurable”, “Serious, but curable”, “Good and curable” and “Didn’t disclose”.
In addition to survey data, we investigated physicians’ approach to communication in routine clinical situations. Questions about the general approach to communication were asked of each physician only once by the questionnaire during the survey period. Physicians were asked about when they explained the purpose of chemotherapy, prognosis, impossibility of cure, hopes about place to die, palliative care unit, home medical care, and do-not-resuscitate (DNR) orders. Response options were: “Explain immediately”, “Explain when cancer symptoms first appear”, “Explain when there is no treatment other than palliative care”, “Explain when patient is hospitalized for worsening symptoms” and “Explain when patient or their family raises the topic”.
Sample size
Based on the previous report (5) that only 19% patients with unresectable/recurrent cancer understood their incurability, we estimated that 20% of enrolled patients would correctly understand that their cancers were incurable. Therefore, we estimated that 246 patients would be required to yield a standard error of <0.05, and set the target sample at 250 patients.
Statistical analysis
Statistical analysis was performed with JMP version 14 for Windows (SAS, Cary, NC, USA).
First, we examined the proportion of patients’ agreement with physicians’ explanations. We included patients who answered the questionnaire and whose physicians reported that they discussed palliative care and the patient’s health condition. Patients whose physicians did not discuss about palliative care and the patient’s current health condition were excluded. Patients in the “Realistic” group agreed with the physicians, or had more pessimistic views than physicians. Patients in the “Optimistic” group did not agree with physicians, or had a more optimistic view than the physicians explained. Patients who answered “We did not discuss this topic” about palliative care or “I don’t know” about current health condition despite having discussed the topic with their physicians, were unlikely to agree with their physicians, and were included in the “Optimistic” group. For palliative care, all patients who answered that they discussed about palliative care were classified into “Realistic group”.
Second, we performed bivariate analysis of patient factors (patient characteristics, EORTC QLQ C30 score and communication score) and physician’s approach. We performed the Wilcoxon rank-sum test for continuous variables, the Cochran-Armitage trend test for ordinal variables and Fisher’s exact test for categorical variables to identify the factors associated with patients in the “Optimistic” group. We considered a P value of <0.05 as significant for a parsimonious model.
Third, we included variables with P values of <0.05 in the univariate analyses for final model fitting using multivariate logistic regression to identify factors associated with patients in the “Optimistic” group. We checked for multicollinearity on the variables with P values of <0.05 in the univariate analyses before adding them to the regression model and there were no variables to exclude.
Results
Patient characteristics
Between February 2015 to January 2016, we enrolled 178 patients (114 men and 62 women) in this study [mean (standard deviation) age, 66 (12.2) years]. The characteristics of these patients are shown in Table 1. Between study recruitment, the responsible researcher was transferred to another hospital. The consequent inability to recruit additional patients considerably limited the study sample size compared with the target of 250.
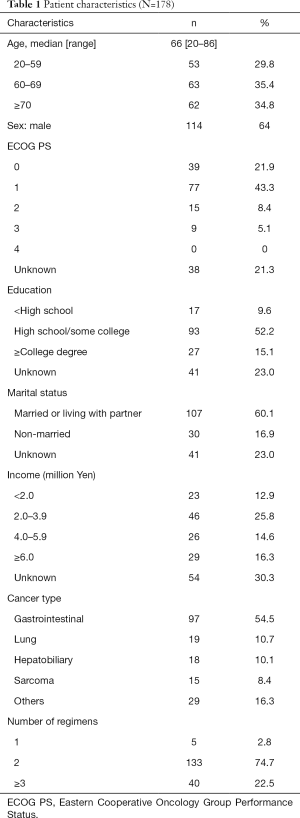
Full table
Physician characteristics
Sixteen physicians with medical oncology backgrounds participated in the survey. Physicians primarily attended to patients with solid cancer, including lung, gastrointestinal, hepatobiliary, head and neck, breast and sarcoma. We did not receive responses from two physicians.
Proportion of patients’ agreement with physicians’ explanation
Tables 2,3 shows the proportion of patients’ agreement with physicians’ explanation. Regarding palliative care, 39 ineligible patients were excluded because they did not answer the question. Among 139 eligible patients, 83 were excluded because physicians did not talk with them about palliative care. Thus, a total of 56 patients were evaluated. Among 56 eligible patients, 25 (44.6%) agreed with their physician, and 31 (55.4%) were optimistic.
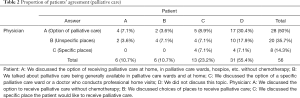
Full table
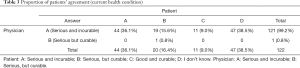
Full table
Regarding current health condition, 48 ineligible patients were excluded because they did not answer the question. Among 130 eligible patients, eight were excluded because physicians did not talk with them about their current health condition. Thus, a total of 122 patients were evaluated. Among 122 eligible patients, 45 (36.9%) agreed with their physician and 77 (63.1%) were optimistic.
Factors associated with optimistic understanding
Table 4 shows the significant results in the bivariate analysis of patients’ factors associated with patients in the “Optimistic” group. Regarding palliative care, four variables had an independent value: treatment preferences (P=0.02), hope about place to recuperate (P=0.03), hope to be informed of survival prediction (P=0.03) and nausea and vomiting (P<0.01). Regarding current health condition, nine variables had an independent value: number of regimens (P=0.04), treatment preferences (P=0.01), hopes about place to die (P=0.04), survival prediction (P=0.01), explanation of the purpose of chemotherapy (P=0.05), social functioning (P<0.01), fatigue (P=0.01), appetite loss (P=0.03) and constipation (P<0.01).

Full table
Table 5 shows the results of the univariate analysis of physicians’ factors associated with patients in the “Optimistic” group. Most physicians explained “immediately” about “impossibility of cure”, “when patient and his or her family raises the topic” about “prognosis”, “when there is no treatment other than palliative care” about “palliative care unit and home medical care” and “when hospitalized for worsening symptoms” about “do-not-resuscitate”. However, physicians’ approach about explaining “hope for a place to die” were disparate. Regarding explanation of the purpose of chemotherapy, all physicians answered “explain immediately”. Therefore, the variable was excluded from the analysis. However, no variables had an independent value.

Full table
Table 6 lists the results of multiple analyses in patients’ factors associated with patients in the “Optimistic” group. Regarding palliative care, one variable had an independent value: aggressive treatment preferences (prolong life vs. palliation) [odds ratio (OR) 3.99; 95% confidence interval (CI), 1.03 to 15.35; P=0.04]. Regarding the current health condition, three variables had an independent value: fewer regimens (1 or 2 vs. ≥3) (OR 63.76; 95% CI, 2.64 to 1,541.67; P=0.01), hopes about place to die (home vs. hospital) (OR 20.45; 95% CI, 1.74 to 239.98; P=0.02) and higher social functioning score (OR 1.06; 95% CI, 1.01 to 1.10; P=0.01).
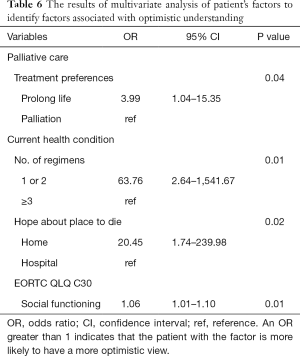
Full table
Discussion
This study yielded three major findings. First, fewer than 50% of Japanese patients agreed with their physicians, whereas most others were more optimistic than physicians’ explanations. Second, several factors were significantly associated with Japanese patients’ proportion of agreement. Third, Japanese physicians’ general approach about disclosure were not associated with patients’ understanding prognosis.
One of the goals of good communication between physicians and patients is to make sure that the patients understand what they are told by physicians. Previous studies have suggested that patients only remember 20% of what they hear in the clinic, and, of that, only remember half of the information correctly; thus, only 10% of everything patients hear is understood and recalled correctly (20). Therefore, the current finding that 30–50% of patients correctly understood the physician's explanation can be considered a relatively high proportion. Based on previous reports, some patients would be expected to hold unrealistic views rather than physicians’ realistic explanations, in order not to lose hope (21); therefore the actual proportion of patients who actually understood their prognosis may have been slightly higher. However, the finding that fewer than 50% of Japanese patients agreed with their physicians suggests that physician-patient communication could be improved. The finding that most patients were more optimistic than physicians’ explanations may also be an obstacle to decision-making according to individuals’ stated goals, values and preferences. A systematic review reported that approximately half of unresectable/recurrent ill cancer patients had accurate prognostic awareness (22). Furthermore, it has been reported that terminally ill cancer patients tend to develop accurate prognostic awareness late in their terminal illness trajectory (23). Therefore, the proportion of agreement might be improved in the late stages of the illness trajectory.
Patients with aggressive treatment preferences were more optimistic about palliative care. Many Japanese people have the image of palliative care as end-of-life care and have resistance to the word “palliative care” to remind them of death (24-28). In addition, as suggested in the results, most physicians explained “when there is no treatment other than palliative care” in relation to palliative care. In Japan, it is common in daily clinical practice to administer first-line treatment for its potential to prolong life. Therefore, it may be natural that patients want to aggressive prolong-life treatment and avoid to think of palliative care.
Patients with fewer regimens were more optimistic about their current health status. Although previous studies reported that patients with unresectable/recurrent cancers tend to have excessively optimistic perceptions of their curability (1,5-7), patients with first-line or second-line regimens might tend to have high expectations for chemotherapy. We found that patients who hoped to die at home had more optimistic views about their current health status. A previous study reported that the predictors of preferred home death included better physical health (29). Thus, patients who preferred home death might have perceived their physical health to be better than their actual health. In addition, it has been reported that social functioning scores evaluated by EORTC QLQ C30 were higher in progressive disease (PD) patients after chemotherapy for gastrointestinal cancer in Japan (30). One of the inclusion criteria in the current study was failure of first-line chemotherapy (PD); therefore, social functioning scores tended to be higher. We speculate that patients with higher social functioning scores may have felt that their disease disturbed their daily life and believed that chemotherapy would improve their health to regain their daily lives.
To date, few studies have examined the influence of physicians’ approach on patient understanding. However, in the current study, physicians’ factors were not associated with agreement proportion. “Physician” was not a significant factor in the bivariate analysis. Therefore, patients’ optimistic views did not appear to be affected by physicians’ approach. Patients’ factors had a greater impact on the proportion of agreement than physicians’ approach. In addition, the current findings revealed differences in approach among physicians. Most physicians had similar approach about explanation about “the purpose of chemotherapy”, “impossibility of cure”, “prognosis”, “palliative care unit and home medical care” and “do-not-resuscitate”. However, physicians’ approach about explanation of “hope about place to die” were disparate. On the other hand, physician’s approach could differ depending on patients in clinical practice although we investigated physician’s approach in routine clinical situation. Further studies on physicians’ approach to individual patients may be necessary.
The current study involved several limitations. First, the statistical power was weaker than planned. The proportion of agreement may have been affected by this limitation. Second, this study was conducted in one region in Japan. Our results regarding the proportion of agreement may not be generalizable to other regions of Japan, or other countries. Third, the cross-sectional design did not allow us to determine causality between the proportion of agreement and other factors. Fourth, because we asked patients and doctors about previous communication, recall bias might be present. Although the physician response was considered the gold standard as to whether communication took place, we cannot be sure that physicians actually discussed the information. Fifth, although patients who answered “I don’t know” despite having discussed the topic with their physicians were included in the “Optimistic” group, the patients might have answered “I don’t know” because physicians’ explanation was too vague or indirect. Therefore, the patients might not be optimistic. Sixth, because physicians approached their own patients with the study, and because they could choose which patients were selected, selection bias is a possible limitation. It would have been more appropriate to obtain informed consent by a researcher other than the primary responsible physician and to conduct rigorous consecutive enrollment.
Overall, the results revealed that many Japanese patients with unresectable/recurrent cancer were optimistic about palliative care communication and their health condition relative to physicians’ explanations. Ensuring effective communication is essential for informed decision-making.
Acknowledgments
We thank Inga T. Lennes, MD, MPH, at Massachusetts General Hospital Cancer Center, Boston, MA, USA for assisting with the backtranslation of the questions used in this survey. We are also deeply grateful to Mrs Yamagishi, RN, of the Department of Palliative Nursing, Tohoku University Graduate School of Medicine, Miyagi, Japan for participant recruitment and data collection. We thank Benjamin Knight, MSc., from Edanz Group (
Funding: This work was supported by JSPS KAKENHI (Grant Numbers 15K15161, 18K10266).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-2045
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-2045
Peer Review File: Available at http://dx.doi.org/10.21037/apm-20-2045
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-2045). Dr. Mitsunori Miyashita serves as an unpaid editorial board member of Annals of Palliative Medicine from Jul 2019 to Jun 2021. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The primary responsible physicians obtained written informed consent from all patients in both Tohoku University Hospital and Miyagi Cancer Center. The independent ethics committee of Tohoku University School of Medicine (approval no. 2014-1-085) and Miyagi Cancer Center (approval no. 2014-010) approved this study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 2008;300:1665-73. [Crossref] [PubMed]
- Mack JW, Cronin A, Keating NL, et al. Associations between end-of-life discussion characteristics and care received near death: a prospective cohort study. J Clin Oncol 2012;30:4387-95. [Crossref] [PubMed]
- Temel JS, Greer JA, Admane S, et al. Longitudinal perceptions of prognosis and goals of therapy in patients with metastatic non-small-cell lung cancer: results of a randomized study of early palliative care. J Clin Oncol 2011;29:2319-26. [Crossref] [PubMed]
- World Health Organization [Internet]. The definition of palliative care; c2002 [cited 2020 Nov 16]. Available online: http://www.who.int/cancer/palliative/definition/en/
- Weeks JC, Catalano PJ, Cronin A, et al. Patients' expectations about effects of chemotherapy for advanced cancer. N Engl J Med 2012;367:1616-25. [Crossref] [PubMed]
- Mack JW, Walling A, Dy S, et al. Patient beliefs that chemotherapy may be curative and care received at the end of life among patients with metastatic lung and colorectal cancer. Cancer 2015;121:1891-7. [Crossref] [PubMed]
- Oishi T, Sato K, Morita T, et al. Patient perceptions of curability and physician-reported disclosures of incurability in Japanese patients with unresectable/recurrent cancer: a cross-sectional survey. Jpn J Clin Oncol 2018;48:913-9. [Crossref] [PubMed]
- Russell BJ, Ward AM. Deciding what information is necessary: do patients with advanced cancer want to know all the details? Cancer Manag Res 2011;3:191-9. [PubMed]
- Bruera E. Process and content of decision making by advanced cancer patients. J Clin Oncol 2006;24:1029-30. [Crossref] [PubMed]
- Kearney MK, Weininger RB, Vachon ML, et al. Self-care of physicians caring for patients at the end of life: "Being connected... a key to my survival". JAMA 2009;301:1155-64, E1.
- Fallowfield L, Jenkins V. Communicating sad, bad, and difficult news in medicine. Lancet 2004;363:312-9. [Crossref] [PubMed]
- Friedrichsen M, Milberg A. Concerns about losing control when breaking bad news to terminally ill patients with cancer: physicians' perspective. J Palliat Med 2006;9:673-82. [Crossref] [PubMed]
- Meier DE, Back AL, Morrison RS. The inner life of physicians and care of the seriously ill. JAMA 2001;286:3007-14. [Crossref] [PubMed]
- Lamont EB, Christakis NA. Prognostic disclosure to patients with cancer near the end of life. Ann Intern Med 2001;134:1096-105. [Crossref] [PubMed]
- Akabayashi A, Kai I, Takemura H, et al. Truth telling in the case of a pessimistic diagnosis in Japan. Lancet 1999;354:1263. [Crossref] [PubMed]
- Wenrich MD, Curtis JR, Shannon SE, et al. Communicating with dying patients within the spectrum of medical care from terminal diagnosis to death. Arch Intern Med 2001;161:868-74. [Crossref] [PubMed]
- Vitillo R, Puchalski C. World Health Organization authorities promote greater attention and action on palliative care. J Palliat Med 2014;17:988-9. [Crossref] [PubMed]
- Ayanian JZ, Zaslavsky AM, Arora NK, et al. Patients' experiences with care for lung cancer and colorectal cancer: findings from the Cancer Care Outcomes Research and Surveillance Consortium. J Clin Oncol 2010;28:4154-61. [Crossref] [PubMed]
- Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 1993;85:365-76. [Crossref] [PubMed]
- Rost K, Roter D. Predictors of recall of medication regimens and recommendations for lifestyle change in elderly patients. Gerontologist 1987;27:510-5. [Crossref] [PubMed]
- DeMartini J, Fenton JJ, Epstein R, et al. Patients' Hopes for Advanced Cancer Treatment. J Pain Symptom Manage 2019;57:57-63.e2. [Crossref] [PubMed]
- Chen CH, Kuo SC, Tang ST. Current status of accurate prognostic awareness in advanced/terminally ill cancer patients: Systematic review and meta-regression analysis. Palliat Med 2017;31:406-18. [Crossref] [PubMed]
- Abarshi E, Echteld M, Donker G, et al. Discussing end-of-life issues in the last months of life: a nationwide study among general practitioners. J Palliat Med 2011;14:323-30. [Crossref] [PubMed]
- Fadul N, Elsayem A, Palmer JL, et al. Supportive versus palliative care: what's in a name?: a survey of medical oncologists and midlevel providers at a comprehensive cancer center. Cancer 2009;115:2013-21. [Crossref] [PubMed]
- Miyashita M, Hirai K, Morita T, et al. Barriers to referral to inpatient palliative care units in Japan: a qualitative survey with content analysis. Support Care Cancer 2008;16:217-22. [Crossref] [PubMed]
- Miyashita M, Sanjo M, Morita T, et al. Barriers to providing palliative care and priorities for future actions to advance palliative care in Japan: a nationwide expert opinion survey. J Palliat Med 2007;10:390-9. [Crossref] [PubMed]
- Morita T, Akechi T, Ikenaga M, et al. Late referrals to specialized palliative care service in Japan. J Clin Oncol 2005;23:2637-44. [Crossref] [PubMed]
- Sanjo M, Miyashita M, Morita T, et al. Perceptions of specialized inpatient palliative care: a population-based survey in Japan. J Pain Symptom Manage 2008;35:275-82. [Crossref] [PubMed]
- Foreman LM, Hunt RW, Luke CG, et al. Factors predictive of preferred place of death in the general population of South Australia. Palliat Med 2006;20:447-53. [Crossref] [PubMed]
- Kato J, Nagahara A, Iijima K, et al. Evaluation of EORTC QLQ-C30 questionnaire in patients undergoing in-hospital chemotherapy for gastrointestinal cancer in Japan. J Gastroenterol Hepatol 2008;23:S268-72. [Crossref] [PubMed]


