
Perioperative treatment compliance, anxiety and depression of elderly patients with ophthalmic surgery and the influential factors
Introduction
Mental health is defined as a continuous good mental state, which manifests as an individual with vitality, positive inner experience and good social adaptation (1). Elderly patients have a decline in physical function due to the aging of various tissues and organs, and they often have special psychological reactions when undergoing surgical treatment. Psychological stress will affect the neuroendocrine system, weaken the body’s immunity, and reduce the tolerance to surgery, thus increasing the difficulty of the operation and influencing treatment efficacy (2). Among the surgical operations, ophthalmic surgery has higher requirements due to the particularity of ocular tissues and nerves. It has been shown that elderly patients have more significant adverse psychological conditions during the perioperative period of ophthalmic surgery than younger patients, which will seriously affect treatment compliance (3). With the aging of the population, the proportion of clinical elderly patients has increased year by year, and how to improve the perioperative poor psychology of elderly patients undergoing ophthalmic surgery and improve their treatment compliance have been brought to clinical attention (4). In this study we analyzed the influential factors on perioperative treatment compliance, anxiety and depression in elderly patients undergoing ophthalmic surgery, aiming to provide ideas for improving clinical treatment. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-21-37).
Methods
Baseline information
The study group comprised 119 elderly patients who underwent ophthalmic surgery between March 2018 and March 2020. The inclusion criteria were: (I) undergone ophthalmic surgery and in a stable condition; (II) age >60 years; (III) complete clinical data and consent to participate in the study; (IV) able to complete questionnaire independently. Exclusion criteria were: (I) malignant tumors; (II) liver, kidney, heart, lung and other vital organ disorders; (III) severe mental illness or family history of mental illness.
Among the study subjects, 61 were male and 58 were female, aged 60–80 years, with an average age of 71.31±5.17 years. The types of surgery undergone were: 29 cases of cataract surgery, 31 of glaucoma surgery, 21 of vitrectomy, 20 of retinal repair surgery, 5 of vitrectomy + retinal repair + silicone oil injection, 4 of vitrectomy + retinal repair + cataract surgery, and 9 of vitrectomy + retinal repair. The education level of the patients was: 42 with elementary school or below, 57 with junior high school to high school, 15 with college to undergraduate, and 5 with postgraduate or above. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by The Third Affiliated Hospital of Qiqihar Medical University (No. 2020-256) and written informed consent was obtained from all patients.
Survey tools
After enrollment, the clinical data of all patients were collected, including sex, age, education level, economic status, treatment plan, marriage status, body mass index, complications, and other general information, for sorting and analysis. The questionnaire included the SAS, SDS and compliance questions. The agreed study protocol was carried out by two nurses. First, the investigator explained the purpose, significance and confidentiality of the study to the patient, and asked for consent before issuing the questionnaire. The investigation was performed 2–3 days after the surgery. If the patient was blind or illiterate, the investigators helped to complete the questionnaire by asking the questions orally to patients and then filling out the questionnaire. All the questionnaires were immediately collected on completion, and the two investigators cross-checked and reviewed any doubtful responses. The recovery rate of the questionnaires was 100.00%.
Self-rating anxiety scale (SAS) (5)
The SAS contains 20 sub-items with four scoring levels to define the frequency of symptoms by the rating items. The positive scoring standard was 1, 2, 3, 4, and the reverse scoring standard was 4, 3, 2, 1. After evaluation, the SAS standard score was obtained by adding up the scores of each item, then multiplying by 1.25 and taking the integer part. The higher the standard score, the more severe the symptoms. A score of <50 points was defined as normal, 50–60 points as mild anxiety, 61–70 points as moderate anxiety, and >70 points indicated severe anxiety.
Self-rating depression scale (SDS) (6)
The scoring method of the SDS scale was basically the same as for the SAS. The higher the standard score, the more severe the symptoms. A score of ≤52 points was defined as normal, 53–62 points as mild depression, 63–72 points as moderate depression, and >73 points indicated severe depression.
Compliance (7)
Patient compliance was divided into three levels: complete compliance was defined as following medical and nursing instructions completely; incomplete compliance was defined as failure to complete or omitting the medical instructions for some reason; complete non-compliance was defined as not following medical or nursing instructions at all. Patients showing complete compliance were rated as good, while those showing incomplete compliance or complete non-compliance were defined as poor.
Statistical analysis
Data were analyzed using SPSS 20.0 statistical software (IBM, New York, USA). Measurement data are expressed as mean ± standard deviation (
Results
Perioperative treatment compliance, anxiety and depression scores
The 119 elderly surgical patients had a mean SAS score of 65.13±14.36 points, and SDS score of 61.94±17.39 points. As for treatment compliance, there were 76 cases (63.87%) of complete compliance, 25 cases of incomplete compliance (21.01%), and 18 cases (15.13%) of complete non-compliance.
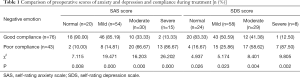
Relationship between depression, anxiety and treatment compliance
The higher the degree of anxiety and depression, the lower the complete compliance in the treatment process (P<0.05, Table 1).
Full table
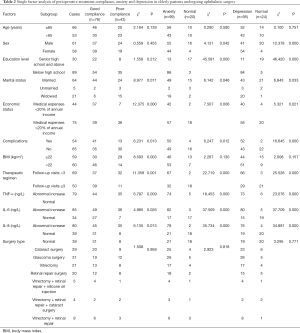
Analysis of factors affecting perioperative treatment compliance, anxiety and depression
Patients with different marital status, economic status, complication status, therapeutic regimen, and levels of TNF-α, IL-6, and IL-8 among the study group of elderly patients undergoing ophthalmic surgery differed in their perioperative treatment compliance (P<0.05). Perioperative anxiety and depression differed among the patients according to sex, education level, marital status, economic status, complications, therapeutic regimen, and levels of TNF-α, IL-6, and IL-8 (P<0.05, Table 2).
Full table
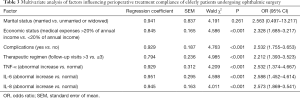
Analysis of multiple factors affecting perioperative treatment compliance
Economic status, complications, therapeutic regimen, and levels of TNF-α, IL-6, and IL-8 were independent risk factors affecting the compliance of elderly patients with ophthalmic surgery during the perioperative period (P<0.05, Table 3).
Full table
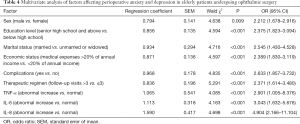
Analysis of multiple factors affecting perioperative anxiety and depression
Sex, education level, marital status, economic status, complication, therapeutic regimen, and levels of TNF-α, IL-6, and IL-8 were independent risk factors affecting perioperative anxiety and depression in elderly patients undergoing ophthalmic surgery (P<0.05, Table 4).
Full table
Discussion
The psychological state of patients requiring corrective surgery is an important factor in good surgical outcome (8). However, because surgery is an invasive treatment, there are many factors influencing the efficacy of surgery, the occurrence of complications, and the recovery time, all of which can affect the psychological reaction of the patient (9).
Depression is an affective disorder characterized by low emotions, crying, sadness, disappointment, reduced mobility, and delayed thinking and cognitive functions (10). Anxiety refers to an inner restlessness or unfounded fear without obvious objective reasons, which is a normal emotional response when people encounter challenges, difficulties or dangers (11). Eye disease is common in elderly patients and research has indicated a general anxiety in ophthalmic surgery patients. The results of our study showed that the 119 elderly surgical patients had a mean perioperative SAS score of 65.13±14.36 and SDS score of 61.94±17.39, with all of them showing mild to moderate anxiety or depression. Negative emotions such as anxiety and depression or the lack of understanding about the surgery can lead to patients not paying enough attention to medical and nursing advice, resulting in poor treatment compliance (12,13). Therefore, clarifying the risk factors that affect the perioperative treatment compliance, anxiety and depression in elderly patients undergoing ophthalmic surgery has great significance for effective interventions to improve patient compliance and surgical efficacy (14).
The occurrence of depression and anxiety is not only related to many mental and physical diseases, but also closely related to a variety of social and environmental factors such as poverty, unemployment, marital problems, family discord, and age (15). A lack of financial security places a heavy burden on patients and therefore greater psychological pressure (16). In addition, patients who have previously undergone operations are aware of the unpredictability in surgery, which increases the psychological pressure and ideological burden (17). Such patients are worried about the effects on their family, so they are often anxious and irritable (18). Cytokines are a series of highly active and multifunctional inductive proteins secreted from the cells. During surgery, the dynamic balance of cytokines may be disturbed to varying degrees. TNF-α, IL-6 and IL-8 are all important mediators involved in inflammatory response, and they can be stimulated and synergized each other. Abnormal levels of TNF-α, IL-6 and IL-8, on the one hand, can increase the incidence of postoperative infectious complications, and on the other hand, can directly affect the surgical effect, and thus affecting the psychological state and treatment compliance of patients. The results of this study showed that increased levels of TNF-α, IL-6 and IL-8 were independent risk factors of treatment compliance, depression and anxiety in elderly patients undergoing eye surgery, which suggested that the regulation of cytokine levels in elderly patients should be paid more attention in clinical practice.
In the process of ophthalmological treatment, more attention should be paid to patients’ treatment compliance and the occurrence of depression, anxiety and other adverse emotions. Depression and anxiety scales should be used in clinical workup to provide a good basis for effective interventions that can improve the anxiety and depression of patients. Research has shown that active psychological intervention in elderly patients undergoing ophthalmic surgery had a significant effect (19). Faezi et al. (20) believe that psychological intervention for elderly patients undergoing ophthalmic surgery needs to include the following aspects: (I) a good doctor–patient relationship, strengthening the overall quality of doctors and nurses, and increasing the trust between patients and doctors; (II) accurate assessment of the patient’s social support, assistance with building a good social support system, improving both patients’ access to social support, and negative emotional state; (III) antipsychotic drugs and psychotherapy for severely affected patients. In short, the modern medical model requires not only solid professional knowledge, but also psychological, ethical, and interpersonal relationship knowledge. Psychological intervention is indispensable for patients undergoing ophthalmic surgery, especially elderly patients, who may need to improvement in their anxiety and depression status while treating the disease, in order to improve the efficacy of surgery and improve quality of life.
In summary, there are many subjective and objective factors that affect the perioperative treatment compliance, anxiety and depression of elderly patients undergoing ophthalmic surgery. Effective interventions based on accurate status should be performed to improve patients’ compliance after treatment, reduce the negative emotions of patients, and successfully improve surgical efficacy.
Acknowledgments
Funding: This study was approved by Qiqihar Science and Technology Project (No. CSFGG-2020014).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-21-37
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-21-37
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-21-37). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by The Third Affiliated Hospital of Qiqihar Medical University (No. 2020-256) and written informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tang YY, Yang HX, Dang D. Analysis of related factors of anxiety and depression in gynecological surgery patients. Nursing Practice Res 2018;34:561-4.
- Faezi ST, Paragomi P, Shahali A, et al. Prevalence and Severity of Depression and Anxiety in Patients With Systemic Sclerosis: An Epidemiologic Survey and Investigation of Clinical Correlates. J Clin Rheumatol 2017;23:80-6. [Crossref] [PubMed]
- Parastoo G, Anita T, Arash N. The Role of Depression, Anxiety, and Stress in Medication Adherence in Patients with Hypertension. Journal of Isfahan Medical School 2017;35:781-8.
- Betancur MN, Lins L, Oliveira IR, et al. Quality of life, anxiety and depression in patients with HIV/AIDS who present poor adherence to antiretroviral therapy: a cross-sectional study in Salvador, Brazil. Braz J Infect Dis 2017;21:507-14. [Crossref] [PubMed]
- Eisele M, Harder M, Rakebrandt A, et al. Association of depression and anxiety with adherence in primary care patients with heart failure-cross-sectional results of the observational RECODE-HF cohort study. Fam Pract 2020;37:695-702. [Crossref] [PubMed]
- Chen T, Wang W, Chen ZS, et al. Prevalence and factors influencing depression and anxiety among AIDS patients in Ili Prefecture. Chinese Journal of Disease Control & Prevention 2018;23:365-8.
- Zhang D, Fan Z, Gao X, et al. Illness uncertainty, anxiety and depression in Chinese patients with glaucoma or cataract. Sci Rep 2018;8:11671. [Crossref] [PubMed]
- Apostolia A, Georgios L. Measuring the effectiveness of psychoeducation on adherence, depression, anxiety and stress among patients with diagnosis of schizophrenia. a control trial. Curr Psychol (New Brunswick, N.J.) 2019;31:1-12.
- Woon LS, Sidi HB, Ravindran A, et al. Depression, anxiety, and associated factors in patients with diabetes: evidence from the anxiety, depression, and personality traits in diabetes mellitus (ADAPT-DM) study. BMC Psychiatry 2020;20:227. [Crossref] [PubMed]
- Cinar M, Cinar FI, Tekgoz E, et al. THU0385 Assessment of relationship between beliefs’ about medicines and treatment adherence in ankylosing spondylitis patients. Ann Rheumatic Dis 2017;76:352-4.
- Montgomery JR, Cohen JA, Brown CS, et al. Perioperative risks of bariatric surgery among patients with and without history of solid organ transplant. Am J Transplant 2020;20:2530-9. [Crossref] [PubMed]
- Manit S, Yee Ming M, Yen Kuang Y, et al. Cognitive Dysfunction in Asian Patients with Depression (CogDAD): A Cross-Sectional Study. Clin Pract Epidemiol Ment Health 2017;13:185-99. [Crossref] [PubMed]
- Wada S, Inoguchi H, Hirayama T, et al. Yokukansan for the treatment of preoperative anxiety and postoperative delirium in colorectal cancer patients: a retrospective study. Jpn J Clin Oncol 2017;47:844-8. [Crossref] [PubMed]
- Rojas-Villegas Y, Ruíz-Martínez AO, González-Sotomayor R. Anxiety and depression on therapeutic adherence in patients with kidney disease. Revista de Psicología 2017;35:347-9.
- Thanawattano C, Buekban C, Dumnin S, et al. The Ambulatory Eye Shield Head Tracking Device with Real-Time Feedback for Gas Filled Eye Patients. Annu Int Conf IEEE Eng Med Biol Soc 2019;2019:7149-52. [Crossref] [PubMed]
- Xiang W, Chen W, Liu R, et al. Ocular Cyclorotation and Corneal Axial Misalignment in Femtosecond Laser-Assisted Cataract Surgery. Curr Eye Res 2019;44:1313-8. [Crossref] [PubMed]
- Dyussenova L, Pivina L, Semenova Y, et al. Associations between depression, anxiety and medication adherence among patients with arterial hypertension: Comparison between persons exposed and non-exposed to radiation from the Semipalatinsk Nuclear Test Site. J Environ Radioact 2018;195:33-9. [Crossref] [PubMed]
- Kazantzis N, Brownfield NR, Mosely L, et al. Homework in Cognitive Behavioral Therapy: A Systematic Review of Adherence Assessment in Anxiety and Depression (2011-2016). Psychiatr Clin North Am 2017;40:625-39. [Crossref] [PubMed]
- Mendes R, Martins S, Fernandes L. Adherence to Medication, Physical Activity and Diet in Older Adults With Diabetes: Its Association With Cognition, Anxiety and Depression. J Clin Med Res 2019;11:583-92. [Crossref] [PubMed]
- Faezi ST, Paragomi P, Shahali A, et al. Prevalence and Severity of Depression and Anxiety in Patients With Systemic Sclerosis: An Epidemiologic Survey and Investigation of Clinical Correlates. J Clin Rheumatol 2017;23:80-6. [Crossref] [PubMed]
(English Language Editor: K. Brown)


