
Association between anxiety, depression, and bowel air bubbles at colonoscopy: a prospective observational study
Introduction
Colonoscopy is one of the most effective means to evaluate the colorectal situation, and plays an important role in the screening, diagnosis, and treatment of colorectal diseases. Colonoscopy is one of the key measures for the secondary prevention of colorectal cancer (CRC) (1). Bowel preparation has been regarded as an important factor in the success of colonoscopy for CRC screening. The quality of colonoscopy is closely related to the accuracy of colonoscopy diagnosis and the safety of treatment. If the intestinal tract is not fully prepared, the detection rate of lesions will be reduced, the unnecessary examination time will be prolonged, and the incidence of discomfort and adverse events will be increased (2).
In recent years, bowel air bubbles have become an indispensable indicator to evaluate intestinal cleanliness. During colonoscopy, there are many folds in the intestinal tract, which have a certain impact on the inspection field (3). Therefore, it is important to maintain high-quality intestinal cleanliness during the examination. Too many air bubbles in the intestinal tract are known as bowel air bubbles, and can cover up the lesion itself, leading to a missed diagnosis (4). At present, simethicone is commonly used as a defoamer at home and abroad, and is sometimes used in combination with intestinal cleansers to improve the defoaming rate and bowel preparation quality.
However, there are still some defects in the use of simethicone (5), such as its bad taste and failure to improve the detection rate of colon polyps. Its safety and effectiveness still need to be evaluated. Psychological factors can also lead to bowel preparation failure. A systematic analysis indicated that anxiety may lead to problems, such as inadequate bowel preparation and difficulty in inserting endoscope (6). Because patients are concerned about the test results and the adverse reactions that may be caused by the examination itself, such as abdominal pain, watching a video description of colonoscopy can relieve their tension and improve the quality of colonoscopy.
People with a high incidence of bowel air bubbles often also have anxiety; however, to the best of our knowledge, there is no current research on the association between anxiety and depression and bowel air bubbles. The present study focuses on the effect of anxiety and depression on the degree of bowel air bubbles in colonoscopy, and in future it could intervene in people with high risk of bowel air bubbles to improve the quality of bowel preparation.
We present the following article in accordance with the STROBE reporting checklist. (available at http://dx.doi.org/10.21037/apm-21-540).
Methods
Study design
The present study was a prospective observational study of patients undergoing colonoscopy at Guangdong Provincial Hospital of Traditional Chinese Medicine from July 2019 to January 2020 (Guangzhou, China). The trial was registered with the Chinese Clinical Trial Centre (registration No. ChiCTR1900024504), and received approval by the ethics committee of Guangdong Provincial Hospital of Traditional Chinese Medicine.
In this trial, all colonoscopies were performed by experienced endoscopists, who had performed >1,000 colonoscopy procedures; trainees were not included in the research. During the procedure, all the treatments were performed normally, and the operator would give the diagnosis based on the examination. All patients were informed about the nature of the study, including the aims and potential advantages and risks, and provided informed consent prior to collection of the questionnaires. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013).
Inclusion criteria
The inclusion criteria were adult patients aged between 18 and 70 years and scheduled for outpatient colonoscopy.
Exclusion criteria
The exclusion criteria were as follows: (I) intestinal obstruction and stenosis; (II) abdominal surgery (including gynecological surgery, appendiceal surgery, and laparoscopic surgery); (III) pregnancy and lactation; (IV) those who meet the contraindications of colonoscopy (severe suppurative inflammation of anus and rectum; severe acute enteritis and ischemic bowel disease; peritonitis, intestinal perforation, extensive intra-abdominal adhesions, and intestinal stenosis caused by various reasons; patients with a large abdominal aortic aneurysm, abnormal bowel flexion, and advanced cancer accompanied by extensive intra-abdominal metastasis; and weakness, and severe cardio-cerebral disease, severe pulmonary dysfunction, and intolerance to the examination); (V) patients with previous inflammatory bowel disease; (VI) failure to perform standardized bowel preparation; (VII) use of simethicone and other defoamers in bowel preparation; (VIII) incomplete data.
Procedure
All patients used the standard intestinal preparation plan. They were advised to eat a low-fiber diet 1 day before endoscopy, and took 68.56 g polyethylene glycol (PEG; Shenzhen Wanhe Pharmaceutical Co., Ltd., Shenzhen, Guangdong, China) with 1,000 mL warm boiled water at 08:00 p.m. the night before the examination. The patients fasted on the examination day, then took 137.15 g PEG with 2,000 mL warm boiled water 5 h prior to examination; routine colonoscopy was then performed. The clinicians instruct the patients to fill in the questionnaire, answer the questions of the questionnaire, and ensure the accuracy of the questionnaire. The clinician was responsible for collecting and sorting through the completed questionnaire, and two researchers input data to the software and checked the data to ensure that they were correct.
Outcomes
General patient information, bubble score, bowel preparation score, and the anxiety and depression score were collected. All colonoscopies were performed by experienced physicians in the endoscopy center. All physicians were trained to complete the Boston scale before study commencement, and were responsible for recording the bubble score and bowel preparation under endoscopy. The primary outcome was degree of the bowel air bubble, measured by bubble scores and evaluated by the doctor who performed the gastrointestinal endoscopy. The bubble scale was used in a previous study described by McNally et al. (7,8). According to the bubble scale (8), the degrees of bowel air bubbles are divided into 4 levels [grade 0, no bubbles; grade 1, minimal or occasional bubbles (must be looked for actively); grade 2, moderate bubbles (obviously visible); grade 3, severe or too many bubbles]. The data were collected by questionnaire survey. In addition, the Boston Bowel Preparation Scale (BBPS) was used to evaluate the feces and liquid in the intestinal cavity by doctors who performed the gastroenteroscopy (9). When the total BBPS score ≥6, it was defined as high-quality bowel preparation. In contrast, inadequate bowel preparation was indicated by a total BBPS score <6.
Sample size calculation
The present study was an observational study, referring to the multi-factor sample content estimation method. The sample size calculation formula was as follows: N=observation variable × [5–10] times. A total of 304 patients were initially included.
Statistical methods
The χ2-test or Fisher’s exact test was used for the categorical data. Student’s t-test or 1-way analysis of variance was used for continuous variables and between-group differences, including mean (± standard deviation) and range. If the data did not conform to the normal distribution, the Mann–Whitney U-test was used. Regression analysis was used to explore risk factors of bowel air bubbles. The mean significance test α=0.05. P<0.05 was considered statistically significant. Missing data is not used to analyze. SPSS version 22.0 (IBM Corp., Armonk, NY, USA) was used for data analysis.
Results
General patient characteristics
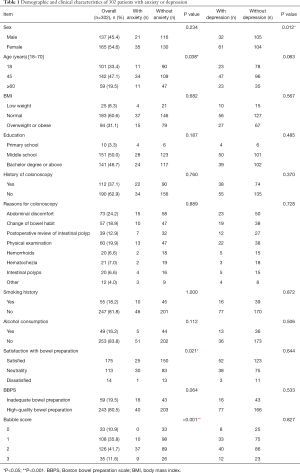
Patients undergoing colonoscopy at the Digestive Endoscopy Center of Guangdong Hospital of Traditional Chinese Medicine from July 2019 to January 2020 were included in the study. A total of 304 questionnaires were issued, and 2 were excluded from the study (Figure 1). Patient demographics and baseline characteristics are shown in Table 1. There were 137 males (45.4%) and 165 females (54.6%), with a male-to-female ratio of 0.83:1. The ages of all included patients were from 18 to 70 years. The mean age of the included patients was 48.74±11.73 years. In terms of body mass index (BMI), 25 were underweight, 183 were normal, and 94 were overweight or obese. In terms of education, 10 had a primary school education, 151 had a secondary school education, and 141 had a bachelor degree or above. Of the 302 patients, 55 had a history of smoking, 247 had no history of smoking, 49 had a history of alcohol consumption, and 253 had no history of alcohol consumption.
Full table
Demographic and clinical characteristics with anxiety or depression
Fifty six of the 302 patients had anxiety in the present study. Of these, 15.3% (21/137) were males and 21.2% (35/165) were females; 10.9% (11/101) of the patients aged 18–45 years had anxiety, 23.9% (34/142) of those aged 45–60 years, and 18.6% (11/59) of those >60 years (P=0.038) (Table 1). There was a significant difference in satisfaction with bowel preparation between those with anxiety and those without (P=0.021) (Table 1). There was also a significant difference in the degree of bowel air bubbles (P<0.001) (Table 1).
Ninety three of the 302 patients had depression in the present study. Of these, 23.3% (32/137) were males and 37% (61/165) were females. There was a significant difference in the sex between those with depression and those without; 22.8% (23/101) of the patients aged 18–45 had anxiety, 33.1% (47/142) of those aged 45–60 years, and 39% (23/59) of those >60 years (P=0.063) (Table 1).
Univariate and multivariate analyses for bowel air bubbles
The risk factor analysis was based on 302 patients in the present study. The univariate and multivariate analyses for bowel air bubbles are shown in Table 2. Four variables (age 45–60 years, a bachelor degree and above, history of colonoscopy, and anxiety) had a P value <0.05.
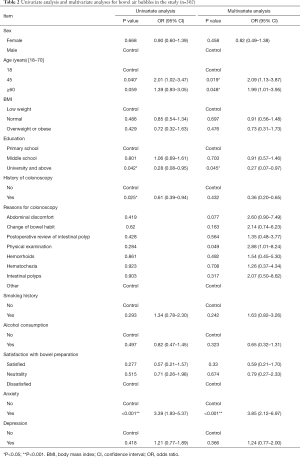
Full table
For the multivariate analysis, 4 variables (age 45–60 years, age >60 years, university education and above, and anxiety) were found to be independent predictors for bowel air bubbles. Age 45–60 years [odds ratio (OR): 2.09, 95% confidence interval (CI): 1.13–3.87], age >60 years (OR: 1.99, 95% CI: 1.01–3.95), and anxiety (OR: 3.85, 95% CI: 2.12–6.97) were identified risk factors for the bowel air bubbles. University education and above (OR: 0.27, 95% CI: 0.07–0.97) were identified protective factors for bowel air bubbles.
Discussion
Good intestinal cleanliness can provide a clear visual environment, which is important to improve the quality of colonoscopy. Multiple meta-analyses have indicated that adequate intestinal preparation is associated with significantly lower detection rates of adenomas and advanced adenomas (10,11). A prospective observational study showed that the rate of missed diagnosis of colorectal adenomas ≥5 mm size was 3 times higher when the intestinal preparation was insufficient (12). In China, 32–57% of colons have obvious intestinal vesicles, which may affect endoscopic examination (4). Previous studies have suggested that the presence of surface bowel air bubbles may be related to colonic viscosity, gastrointestinal motility, and bile secretion and excretion (13).
Psychological factors can also cause bowel preparation failure. Hertig et al. found that, in irritable bowel syndrome (IBS) patients, intestinal symptoms (constipation or diarrhea), abdominal pain, abdominal distension, and gas in the intestinal cavity were correlated with psychological stress (14). In their study, Gorard et al. observed the intestinal transport time of 21 patients with mental and emotional disorders using the oral method of radioactive markers (15). The frequency of intestinal movement was found to be faster in anxious patients, and the time of intestinal movement was slowest in depressed patients (15). This suggests that psychological factors, such as anxiety and depression, can affect the degree of bubbles in the intestinal lumen by regulating the speed of intestinal transport. However, there are few reports on the factors influencing bowel air bubbles. In the present study, we preliminarily investigated the relationship between anxiety and depression and bowel air bubble cleanliness.
The number of bowel air bubbles was not statistically significant in terms of sex, age, BMI, education, smoking history, and alcohol consumption. A slightly higher proportion of women were randomly enrolled for colonoscopy in the present study. Previous studies have found that men are more likely to undergo colonoscopy than women, and that men have a higher incidence of CRC and females chose colonoscopy because of the inconvenience caused by the lack of female endoscopists (16). The sex distribution of patients in the present study was different from those of previous epidemiological studies, which may be due to the long distance between relevant epidemiological studies. With the popularization of medical knowledge, more female patients have realized the importance of colonoscopy screening. In terms of age, the colonoscopy group showed a younger trend, among which the young and middle-aged group was the most. This may be related to the recommendation of guidelines for CRC screening as early as possible for people at moderate risk, especially those >50 years (17). Ladabaum et al. made a nationwide prediction based on census data and found that colonoscopy after age 45 could avoid the occurrence of CRC to the greatest extent (18). However, due to the large social and economic pressure and irregular diets of young and middle-aged people, experimental studies found that high-fat diets activated tumor-related macrophages and accelerated the deterioration of intestinal adenoma (19). Therefore, young and middle-aged people are more likely to undergo colonoscopy.
In terms of the relationship between anxiety score and bubbles, in the univariate analysis in the present study, we found that the anxiety standard score was correlated with the number of bowel air bubbles, and the higher the anxiety standard score, the higher the bubble score. After multi-factor adjustment, anxiety was found to be a risk factor for bowel air bubbles.
A study of anxiety and colonoscopy (20) found that women were more likely to have anxiety compared with men. Similarly, people who have their first colonoscopy, not complete their course of laxatives, and not be familiar with the procedure are more anxiety. This study also discussed whether anxiety resulted in patients having difficulty completing the bowel preparation process, leading to a decline in the quality of bowel preparation. A multivariate analysis found that anxiety may be caused by gastrointestinal discomfort (20). Women were also more likely to have anxiety compared with men, which partly due to sex difference in certain neural circuits (21-23).
There are many reasons that affect the generation of bowel air bubbles, and these are mainly related to gastrointestinal motility. Gas is transmitted from the upper digestive tract to the colorectal segment through intestinal peristalsis (24), and bubbles are generated during peristalsis. Previous studies have found that anxiety is related to intestinal movement from the upper site (15). In the present study, we found that the number of bubbles decreased from the right to the left of the intestinal segment, that is, from the cecum to the rectum, indicating that the gas in the colon segment may originate from the small intestine. Studies have shown that a large number of patients have anxiety about colonoscopy and examination results, and such anxiety may induce increased frequency of intestinal movement, resulting in more bubbles, which stick to the colon wall and affect the visual field of examination (15,20).
The close relationship between anxiety and depression, known as psychological distress, and IBS has been demonstrated extensively in the literature (24-27). IBS patients with gastrointestinal issues tend to be at a high level of anxiety, which is known as gastrointestinal-specific anxiety (28). However, a multivariate analysis on IBS and stress indicated that colonic transit time has no significant difference in patients with and without anxiety and depression (27). Another study on lactose malabsorption and intolerance indicated that anxiety, which may be the result of fear of abdominal pain and diarrhea triggered by food, increases the risk of lactose intolerance (29). This intolerance is a result of rapid small intestinal transit and bacterial imbalance (30).
Studies have shown that the video explanation before the examination can reduce the anxiety of patients to a certain extent (20), as can music and brochures. Other studies have shown that there is a certain relationship between gas in the intestinal cavity and mental pressure of patients (14).
Psychological factors are closely related to the digestive system. Many studies have shown that homeostatic regulation of intestinal microecology is associated with psychological diseases, especially depressive behaviors (31-33). However, depression and anxiety are often accompanied by changes in colon dynamics, which in turn change the composition and stability of intestinal microbiota, as well as the physiology and morphology of the colon (34,35). Depression is usually accompanied by changes in colonic transport (27,36). Experimental studies have clearly shown that changes in colonic motility occur in depressed mice, and the driving agent of exercise change is due to the increased expression of kinesthetic neuropeptides, intestinal hormones, and serotonin in the colonic wall (37,38).
In patients with IBS who also have depression, changes in colon motion caused by depression aggravate the severity of intestinal dysfunction and further destroy the stability of intestinal flora (39,40). A statistically significant association between intestinal microbial composition and depression and slow colon metastasis in IBS patients has been found in a previously published study (41). A Japanese study found that depression was associated with the patients with a lower frequency of bowel movements and laxatives had higher depression-related risk factors (42).
In terms of the relationship between BBPS score and bubbles, the BBPS score included whether the fecal liquid affected the visual field. The higher the score, the better the intestinal preparation quality. In the present study, it was found that the group with fewer bubbles had a higher BBPS score, indicating that there were fewer bubbles and fewer liquid pairs of fecal slag remaining in the intestinal cavity. The BBPS score may have taken into account the bubble condition to some extent, which was consistent with the bubble condition evaluation. However, excessive bubbles are difficult to be rinsed out in colonoscopy with sterile water alone, which can have a serios impact on observation of the intestinal cavity. Therefore, the evaluation of intestinal preparation quality should be more comprehensive and include the evaluation of bowel air bubbles. Guo et al. used the bubble score as a supplement to the BBPS score to evaluate intestinal cleanliness in order to explore the detection rate of colorectal adenoma (43). They found that 65.7% of patients had bowel air bubbles that affected visual field observation, and the bowel air bubbles were negatively correlated with the detection rate of adenoma.
Limitations
The present study has some limitations. First, this was a single-center study, and all the included cases were from Guangdong Hospital of Traditional Chinese Medicine. The source is single, the research time span was not large enough, and there are regional seasonal factors, so it probably represents the characteristics of colonoscopy patients in this region. Second, the number of included cases was small, mainly because the questionnaire covered a wide range of items and took some time to complete. People are generally time poor, which increases the difficulty of questionnaire completion. Third, we adopted the questionnaire survey method in the present study. Although we explained the questions and options in detail to the patients, patients may have different understandings of these when filling in the questionnaire, resulting in certain bias. In future studies, we hope to use the questionnaire on a larger sample size, and conduct multi-center studies to further explore the relationship between bowel air bubble cleanliness and anxiety and depression so as to determine a bowel preparation plan for intervention and provide strong scientific support for individualized high-quality intestinal preparation.
The present study included 302 patients who underwent colonoscopy. No significant differences in sex, age, BMI, level of education, smoking history, alcohol consumption, and distribution of depression score between the 4 groups were found; however, the anxiety score and BBPS score demonstrated statistically significant differences. As the degree of the bowel air bubble increased, anxiety scores also increased and the BBPS scores decreased. To improve the quality of bubble clearance, bowel preparation for intestinal preparation, and satisfaction, the first step is to reduce anxiety. This could be done with the use of details brochures or a video on the procedure, and with an emphasis on the psychological guidance before colonoscopy. This could broaden patients’ understanding of the procedure and alleviate stress. Face to face counseling should be actively conducted according to different needs, with targeted nursing work.
In the present study, the association of anxiety on bowel air bubbles were discussed, and we found that personalized early intervention could improve the quality of intestinal preparation and clarity of the intestinal field so as to improve the quality of colonoscopy.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-21-540
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-21-540
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-21-540). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The trial received approval by the ethics committee of Guangdong Provincial Hospital of Traditional Chinese Medicine. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). All patients were informed about the nature of the study, including the aims and potential advantages and risks, and provided informed consent prior to collection of the questionnaires.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rex DK, Boland CR, Dominitz JA, et al. Colorectal cancer screening: Recommendations for physicians and patients from the U.S. Multi-Society Task Force on Colorectal Cancer. Gastrointest Endosc 2017;86:18-33. [Crossref] [PubMed]
- Kim MJ, Hong CW, Kim BC, et al. Phase II Randomized Controlled Trial of Combined Oral laxatives Medication for BOwel PREParation (COMBO-PREP study). Medicine (Baltimore) 2016;95:e2824 [Crossref] [PubMed]
- De Palma GD, Giglio MC, Bruzzese D, et al. Cap cuff–assisted colonoscopy versus standard colonoscopy for adenoma detection: a randomized back-to-back study. Gastrointest Endosc 2018;87:232-40. [Crossref] [PubMed]
- Digestive Endoscopy Special Committee of Endoscopic Physicians Branch of Chinese Medical Association. Digestive, Chinese guideline for bowel preparation for colonoscopy (2019, Shanghai). Zhonghua Nei Ke Za Zhi 2019;58:485. [PubMed]
- Bai Y, Fang J, Zhao SB, et al. Impact of preprocedure simethicone on adenoma detection rate during colonoscopy: a multicenter, endoscopist-blinded randomized controlled trial. Endoscopy 2018;50:128-36. [PubMed]
- Yang C, Sriranjan V, Abou-Setta AM, et al. Anxiety Associated with Colonoscopy and Flexible Sigmoidoscopy: A Systematic Review. Am J Gastroenterol 2018;113:1810-8. [Crossref] [PubMed]
- McNally PR, Maydonovitch CL, Wong RK. The effectiveness of simethicone in improving visibility during colonoscopy: a double-blind randomized study. Gastrointest Endosc 1988;34:255-8. [Crossref] [PubMed]
- Lazzaroni M, Petrillo M, Desideri S, et al. Efficacy and tolerability of polyethylene glycol-electrolyte lavage solution with and without simethicone in the preparation of patients with inflammatory bowel disease for colonoscopy. Aliment Pharmacol Ther 1993;7:655-9. [Crossref] [PubMed]
- Lai EJ, Calderwood AH, Doros G, et al. The Boston bowel preparation scale: a valid and reliable instrument for colonoscopy-oriented research. Gastrointest Endosc 2009;69:620-5. [Crossref] [PubMed]
- Sulz MC, Kroger A, Prakash M, et al. Meta-Analysis of the Effect of Bowel Preparation on Adenoma Detection: Early Adenomas Affected Stronger than Advanced Adenomas. PLoS One 2016;11:e0154149 [Crossref] [PubMed]
- Clark BT, Rustagi T, Laine L. What level of bowel prep quality requires early repeat colonoscopy: systematic review and meta-analysis of the impact of preparation quality on adenoma detection rate. Am J Gastroenterol 2014;109:1714-23; quiz 1724. [Crossref] [PubMed]
- Clark BT, Protiva P, Nagar A, et al. Quantification of Adequate Bowel Preparation for Screening or Surveillance Colonoscopy in Men. Gastroenterology 2016;150:396-405; quiz e14-5. [Crossref] [PubMed]
- Yang ZL, Zhao M, Huang QR, et al. Application of simethicone before colonoscope examination. China Journal of Endoscopy 2017;23:26-9.
- Hertig VL, Cain KC, Jarrett ME, et al. Daily Stress and Gastrointestinal Symptoms in Women With Irritable Bowel Syndrome. Nur Res 2007;56:399-406. [Crossref] [PubMed]
- Gorard DA, Gomborone JE, Libby GW, et al. Intestinal transit in anxiety and depression. Gut 1996;39:551-5. [Crossref] [PubMed]
- Mittal S, Lin YL, Tan A, et al. Limited Life Expectancy Among a Subgroup of Medicare Beneficiaries Receiving Screening Colonoscopies. Clin Gastroenterol Hepatol 2014;12:443-50. [Crossref] [PubMed]
- Săftoiu A, Hassan C, Areia M, et al. Role of gastrointestinal endoscopy in the screening of digestive tract cancers in Europe: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy 2020;52:293-304. [Crossref] [PubMed]
- Ladabaum U, Mannalithara A, Meester R, et al. Cost-Effectiveness and National Effects of Initiating Colorectal Cancer Screening for Average-Risk Persons at Age 45 Years Instead of 50 Years. Gastroenterology 2019;157:137-48. [Crossref] [PubMed]
- Liu T, Guo Z, Song X, et al. High-fat diet-induced dysbiosis mediates MCP-1/CCR2 axis-dependent M2 macrophage polarization and promotes intestinal adenoma-adenocarcinoma sequence. J Cell Mol Med 2020;24:2648-62. [Crossref] [PubMed]
- Shafer LA, Walker JR, Waldman C, et al. Factors Associated with Anxiety About Colonoscopy: The Preparation, the Procedure, and the Anticipated Findings. Dig Dis Sci 2018;63:610-8. [Crossref] [PubMed]
- Beesdo K, Knappe S, Pine DS. Pine, Anxiety and Anxiety Disorders in Children and Adolescents: Developmental Issues and Implications for DSM-V. Psychiatr Clin North Am 2009;32:483-524. [Crossref] [PubMed]
- Moser JS, Moran TP, Kneip C, et al. Sex moderates the association between symptoms of anxiety, but not obsessive compulsive disorder, and error-monitoring brain activity: A meta-analytic review. Psychophysiology 2016;53:21-9. [Crossref] [PubMed]
- Bangasser DA, Valentino RJ. Sex differences in stress-related psychiatric disorders: neurobiological perspectives. Front Neuroendocrinol 2014;35:303-19. [Crossref] [PubMed]
- Kutyla M, O'Connor S, Gurusamy SR, et al. Influence of Simethicone Added to the Rinse Water during Colonoscopies on Polyp Detection Rates: Results of an Unintended Cohort Study. Digestion 2018;98:217-21. [Crossref] [PubMed]
- Roohafza H, Bidaki E, Hasanzadeh-Keshteli A, et al. Anxiety, depression and distress among irritable bowel syndrome and their subtypes: An epidemiological population based study. Adv Biomed Res 2016;5:183. [Crossref] [PubMed]
- Cho HS, Park JM, Lim CH, et al. Anxiety, depression and quality of life in patients with irritable bowel syndrome. Gut Liver 2011;5:29-36. [Crossref] [PubMed]
- Midenfjord I, Polster A, Sjovall H, et al. Anxiety and depression in irritable bowel syndrome: Exploring the interaction with other symptoms and pathophysiology using multivariate analyses. Neurogastroenterol Motil 2019;31:e13619 [Crossref] [PubMed]
- Jerndal P, Ringstrom G, Agerforz P, et al. Gastrointestinal-specific anxiety: an important factor for severity of GI symptoms and quality of life in IBS. Neurogastroenterol Motil 2010;22:646-e179. [Crossref] [PubMed]
- Misselwitz B, Butter M, Verbeke K, et al. Update on lactose malabsorption and intolerance: pathogenesis, diagnosis and clinical management. Gut 2019;68:2080-91. [Crossref] [PubMed]
- Davidson GP, Goodwin D, Robb TA. Incidence and duration of lactose malabsorption in children hospitalized with acute enteritis: study in a well-nourished urban population. J Pediatr 1984;105:587-90. [Crossref] [PubMed]
- Bravo JA, Forsythe P, Chew MV, et al. Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proc Natl Acad Sci U S A 2011;108:16050-5. [Crossref] [PubMed]
- Desbonnet L, Clarke G, Traplin A, et al. Gut microbiota depletion from early adolescence in mice: Implications for brain and behaviour. Brain Behav Immun 2015;48:165-173. [Crossref] [PubMed]
- Wong ML, Inserra A, Lewis MD, et al. Inflammasome signaling affects anxiety- and depressive-like behavior and gut microbiome composition. Mol Psychiatry 2016;21:797-805. [Crossref] [PubMed]
- Bailey MT, Coe CL. Maternal separation disrupts the integrity of the intestinal microflora in infant rhesus monkeys. Dev Psychobiol 1999;35:146-55. [Crossref] [PubMed]
- O'Malley D, Julio-Pieper M, Gibney SM, et al. Distinct alterations in colonic morphology and physiology in two rat models of enhanced stress-induced anxiety and depression-like behaviour. Stress 2010;13:114-22. [Crossref] [PubMed]
- Lechin F, Van der Dijs B, Acosta E, et al. Distal colon motility and clinical parameters in depression. J Affect Disord 1983;5:19-26. [Crossref] [PubMed]
- Rodes L, Paul A, Coussa-Charley M, et al. Transit time affects the community stability of Lactobacillus and Bifidobacterium species in an in vitro model of human colonic microbiotia. Artif Cells Blood Substit Immobil Biotechnol 2011;39:351-6. [Crossref] [PubMed]
- Park AJ, Collins J, Blennerhassett PA, et al. Altered colonic function and microbiota profile in a mouse model of chronic depression. Neurogastroenterol Motil 2013;25:733-e575. [Crossref] [PubMed]
- Folks DG. The interface of psychiatry and irritable bowel syndrome. Curr Psychiatry Rep 2004;6:210-5. [Crossref] [PubMed]
- Matto J, Maunuksela L, Kajander K, et al. Composition and temporal stability of gastrointestinal microbiota in irritable bowel syndrome--a longitudinal study in IBS and control subjects. FEMS Immunol Med Microbiol 2005;43:213-22. [Crossref] [PubMed]
- Jeffery IB, Quigley EM, Ohman L, et al. The microbiota link to irritable bowel syndrome: an emerging story. Gut Microbes 2012;3:572-6. [Crossref] [PubMed]
- Kubota Y, Iso H, Tamakoshi A. Bowel Movement Frequency, Laxative Use, and Mortality From Coronary Heart Disease and Stroke Among Japanese Men and Women: The Japan Collaborative Cohort (JACC) Study. J Epidemiol 2016;26:242-8. [Crossref] [PubMed]
- Guo R, Wang YJ, Liu M, et al. The effect of quality of segmental bowel preparation on adenoma detection rate. BMC Gastroenterol 2019;19:119. [Crossref] [PubMed]
(English Language Editor: R. Scott)



