
Outcomes and prognostic factors of apical periodontitis by root canal treatment and endodontic microsurgery—a retrospective cohort study
Introduction
Apical periodontitis (AP) is an inflammatory disorder of periapical tissues caused by etiological agents of endodontic origin (1). AP is one of the major causes of tooth extraction and may have local clinical signs of inflammation such as pain, swelling, or loss of function. In addition, AP may affect the general health of the patient by changing peripheral blood levels of inflammatory mediators and markers (2). Teeth with AP can be managed by either nonsurgical root canal treatment (RCT) or apical surgery (AS). In general, RCT includes initial RCT and nonsurgical retreatment (re-RCT).
RCT is the preferred treatment choice for AP as it eliminates microorganisms from the root canal system via chemo-mechanical debridement, followed by root filling to provide a good biological environment for the healing of AP. The success rate of RCT in teeth with AP varies from 53.6% to 87.8% (3-5). Re-RCT or AS can be considered for the treatment of persistent AP after initial RCT. AS is the treatment of choice for persistent AP as it can manage the infected apex, extra-radicular infection or true cysts and provide a hermetic seal of the apical area directly. The now widely used endodontic microsurgery (EMS) using a microscope, ultrasonic retro-tips, and new retro-filling materials has shown a significantly high success of 90% at 2–4 years and 84% at 4–6 years (6).
Numerous studies have been performed to evaluate the outcome and prognostic factors of RCT and EMS based on clinical and radiographic examinations (7-10). However, reported outcomes have shown considerable differences, probably due to differences in the data composition, clinical procedures, and methodology (3). In addition, previous analysis of the outcome of RCT was based on pulpal and periapical diseases, including cases with or without preoperative periapical lesions. It has been confirmed that the success was significantly lower in cases with periapical lesions than in those without periapical lesions (5,10-12). The healing of pulpal disease and AP after RCT involves different pathophysiological procedures. Therefore, in order to improve the understanding of AP, it is necessary to analyze the outcome of AP separately.
Many studies have also compared the success of initial RCT and re-RCT (5,9-12), most of which showed that the success rate of initial RCT was higher than that of re-RCT (9-12), while one study demonstrated that there was no difference (5). However, these studies included all pulpal and periapical diseases, and no conclusion was reached on the outcome difference between initial RCT and re-RCT of AP, or on the difference in prognostic factors following initial RCT and re-RCT for AP (13).
Therefore, by reviewing the medical records of patients with AP who received treatment in the Stomatology Department of the Peking University Third Hospital from January 2016 to December 2019, this study analyzed the outcome and prognostic factors of RCT and EMS in the treatment of AP, respectively, and the difference in outcome and prognostic factors between initial RCT and re-RCT.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-2507).
Methods
Study design and cohort establishment
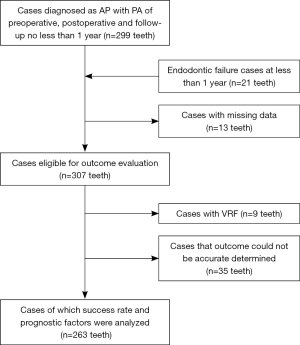
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Medical Science Research Ethics Committee of Peking University Third Hospital (No. 2020/142-03) and individual consent for this retrospective analysis was waived. The clinical records of all patients who were diagnosed with AP in the Department of Stomatology of Peking University Third Hospital from January 2016 to December 2019 were reviewed. Treatment options included RCT (initial RCT and re-RCT) and EMS. If RCT was undertaken, and failure was found at review, then EMS was undertaken, it was classified as one EMS case with a failed RCT history. Data were collected in a variety of ways to reduce loss to follow-up. Cases with periapical radiographs (PA) of preoperative, postoperative and follow-up images of no less than 1 year were included. In addition, cases who had teeth extracted or who underwent further treatment at less than 1 year due to endodontic failure were also included. Cases with missing data were excluded; thus, all patients in this cohort had complete data. In the outcome evaluation phase, cases with vertical root fracture (VRF) and those in whom outcome could not be accurately determined were excluded. The flowchart of case review and selection is shown in Figure 1.
RCT procedures
All of the RCT procedures were performed according to standard operation guidelines (14). After access cavity preparation, working length determination was aided by an electronic apex locator (Root ZX mini; J Morita Corp, Tokyo, Japan). The canals were enlarged in a crown-down or step-back technique using nickel-titanium rotary or stainless steel instruments. The canals were filled using the cold lateral compaction or a warm vertical condensation technique with gutta-percha and RoekoSeal sealer (Coltene/Whaledent, Langenau, Germany) followed by a definitive coronal restoration material, or a post and crown. In the case of multiple visit treatment, calcium hydroxide was used as an intracanal medication between appointments.
EMS procedures
All 34 EMS were performed by an experienced endodontic specialist under microscope using a standardized clinical protocol (15). Local anesthesia was administered followed by flap elevation. A surgical curette was used to enucleate the pathological tissue and identify the root apex with/without prior osteotomy. Approximately 3 mm of the apical was resected perpendicular to the long axis of the tooth with no or minimal bevel. The root apex and root surfaces before and after root-end resection was carefully inspected and observed under an OPMI Proergo operative microscope (Carl Zeiss AG, Jena, Germany). The root-end cavity was prepared with ultrasonic micro-tips and filled with retrograde materials, either ProRoot MTA (Dentsply Maillefer, Ballaigues, Switzerland) or IRM (Caulk Co., Ltd., Densply International, Milford, DE, USA). Flaps were repositioned and sutured. Antibiotics and analgesic medication were prescribed.
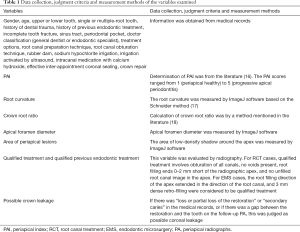
Data collection
A total of 27 variables were collected. Some variables were obtained from the medical records, while other variables were obtained by preoperative and postoperative PA evaluation or measurement. The specific judgment and measurement methods of the 27 variables are shown in Table 1.
Full table
PA using a parallel technique was obtained by Sirona Dental Systems GmhH (Sirona, Bensheim, Germany). ImageJ software (version 1.51, NIH Image, Bethesda, MD, USA) was used to measure the root curvature degree, crown root ratio, apical foramen diameter, and periapical lesion area of the teeth. Two experienced endodontic specialists independently evaluated the PA in a quiet environment, respectively, and the two observers had good agreement (kappa =0.822). In the case of inconsistent results, the two evaluators reached a consensus after discussion.
Outcome assessment
The presence or absence of signs and symptoms (pain, swelling, sinus tract) and the changes in periapical lesion area were used as outcome measures. Teeth were classified as successful healing when (I) clinically, there was absence of signs and symptoms and (II) radiographically, there was reduced periapical lesion area. Teeth were classified as unsuccessful healing or failure when clinical signs and symptoms were present, or when there was an unchanged or enlarged periapical lesion area. If a tooth had multiple roots and one of the roots was evaluated as unsuccessful, the tooth was classified as unsuccessful healing. Radiographically, preoperative and follow-up PA were compared to evaluate the periapical bone healing according to whether the measured periapical lesion area decreased. As the angles of preoperative and follow-up PA were not totally consistent, the measurement results of periapical lesion areas were incomparable. Therefore, the two images were calibrated with the ImageJ Turboreg plugin, and then the areas of radiolucency around the apex of both preoperative and follow-up PA were measured by ImageJ and compared to obtain the outcome. The devices and methods used to read the film were the same as those used for imaging assessments of variables as described above. If the observers could not reach an agreement, the case was excluded.
Statistical analysis
Data analyses were performed using SPSS 26.0 software (IBM, Chicago, IL, USA). Among quantitative variables, the apical foramen diameter is converted to categorical variables with 1mm as the limit. Other quantitative variables were still statistically analyzed as quantitative variables. The median and interquartile range were used to describe quantitative variables, and the frequency and percentage were used to describe categorical variables. A battery of statistical analyses, including the χ2 test, Fisher’s exact test and Mann-Whitney U test were performed. All variables that demonstrated a P value <0.1 were incorporated into the multivariate logistic model to identify variables with statistically significant differences. Stratified subsamples were analyzed separately when deemed appropriate. All statistical tests were two-tailed, and interpreted at the 5% significance level. For total RCT, logistic regression analysis was performed on 10 possible influencing factors, requiring at least 50 successful cases and 50 failed cases. There were 162 successful cases and 67 failed cases in this retrospective cohort, which met the sample size requirements for influencing factor analysis of efficacy.
Results
Description of the study sample
A total of 263 cases were included in this retrospective cohort study. The follow-up time in the 263 cases was an average of 19 months (range, 1–46 months). Of the 229 RCT cases, 126 were completed by endodontic specialists and 103 by general dentists; 21 teeth were extracted or underwent further treatment at less than 1 year due to endodontic failure, and the remaining 208 teeth were followed up for an average of 20 months (range, 12–45 months). In addition, the follow-up time in 34 EMS cases was an average of 21 months (range, 12–46 months). Of the total 263 cases in the AP cohort, 194 cases showed successful healing (73.8%), and 69 cases (26.2%) showed unsuccessful healing.
Treatment outcome and prognostic factors of total RCT
The univariate analysis (Table 2) results revealed that of the total 229 RCT cases, 162 cases (70.7%) had successful healing, and 67 cases (29.3%) had unsuccessful healing. Significant successful healing rate differences were associated with five variables (P<0.05): age, crown root ratio, doctor classification, unqualified treatment and irrigation activated by ultrasound. With regard to preoperative factors, younger patients (P=0.002) and teeth with a smaller crown root ratio (P<0.001) had a more favorable outcome. With regard to intraoperative factors, teeth treated by an endodontic specialist (P=0.01), qualified treatment (P<0.001) and irrigation activated by ultrasound (P=0.047) resulted in a significantly greater success rate.
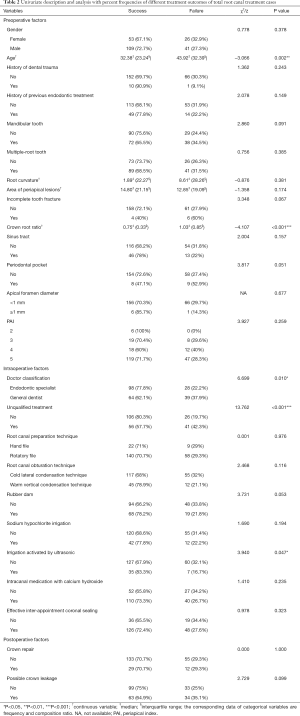
Full table
Multiple logistic regression results are shown in Table 3. These results revealed that treatment outcome following total RCT was significantly associated with five variables: age [odds ratio (OR) =1.025; confidence interval (CI): 1.005, 1.045], incomplete tooth fracture (OR =7.082; CI: 1.516, 33.089), crown root ratio (OR =1.198; CI: 1.019, 1.408), general dentist (OR =2.16; CI: 1.03, 4.545), and unqualified treatment (OR =2.841; CI: 1.456, 5.525). Thus, older age, greater crown root ratio, incomplete tooth fracture, general dentist rather than endodontic specialist and unqualified treatment were risk factors in the treatment of AP by total RCT.
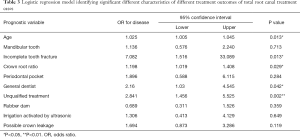
Full table
Treatment outcome and prognostic factors of initial RCT
The univariate analysis (Table 4) results revealed that of the 166 initial RCT cases, 113 cases (68.1%) had successful healing, and 53 cases (31.9%) had unsuccessful healing. Significant successful healing differences were associated with five variables (P<0.05): mandibular teeth, crown root ratio, sinus tract, unqualified treatment and root canal obturation technique. With regard to preoperative factors, maxillary teeth (P=0.042), teeth with a smaller crown root ratio (P=0.002) and a sinus tract (P=0.026) had a more favorable outcome. With regard to intraoperative factors, qualified treatment (P=0.018) and teeth treated with the warm vertical condensation technique (P=0.02) resulted in a significantly greater success rate.
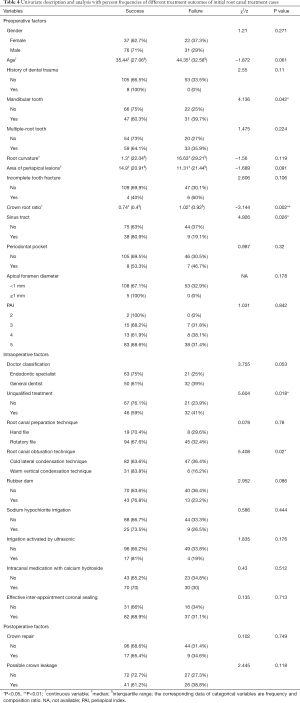
Full table
Multiple logistic regression results are shown in Table 5. These results revealed that treatment outcome following initial RCT was significantly associated with crown root ratio (OR =1.333; CI: 1.095, 1.623). Thus, greater crown root ratio is a risk factor in the treatment of AP by initial RCT.
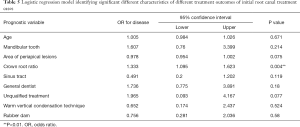
Full table
Treatment outcome and prognostic factors of re-RCT
The univariate analysis (Table 6) results revealed that of the 63 re-RCT cases, 49 cases (77.8%) had successful healing, and 14 cases (22.2%) had unsuccessful healing. Significant successful healing rate differences were associated with four variables (P<0.05): age, crown root ratio, periodontal pocket and unqualified treatment. With regard to preoperative factors, younger patients (P=0.008), teeth with a smaller crown root ratio (P=0.007) and teeth without periodontal pocket (P=0.047) had a more favorable outcome. With regard to intraoperative factors, unqualified treatment (P=0.005) resulted in a significantly lower success rate.
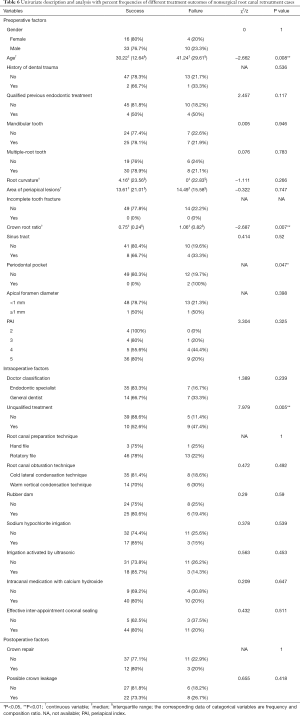
Full table
Multiple logistic regression results are shown in Table 7. These results revealed that treatment outcome following re-RCT was significantly associated with unqualified treatment (OR =5.291; CI: 1.339, 20.833). Because there are only two cases with periodontal pocket, the variable was not included in the regression model analysis, and the regression analysis of cases without periodontal pocket also revealed that unqualified treatment is a significant prognostic factor (OR =6.41; CI: 1.51, 27.0). Thus, unqualified treatment is a risk factor in the treatment of AP by re-RCT.
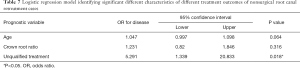
Full table
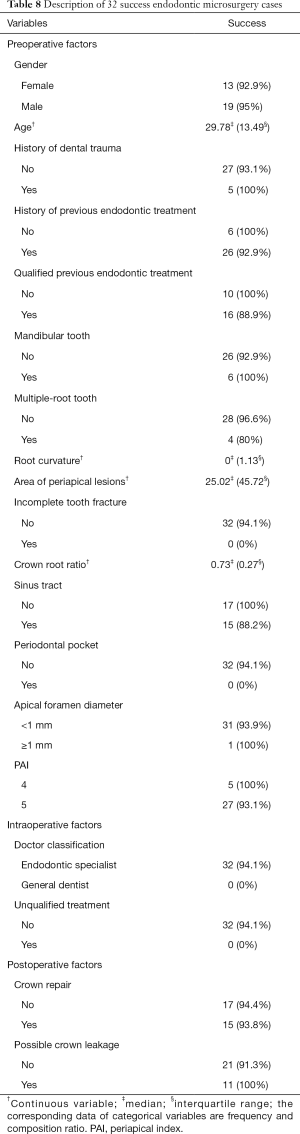
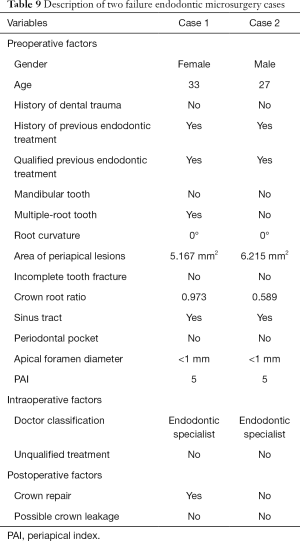
Description of EMS cases
The description of EMS cases (Tables 8 and 9) revealed that of the 34 examined cases, 32 cases (94.1%) had successful healing, and two cases (5.9%) had unsuccessful healing. The univariate analysis results revealed that none of the variables examined were associated with significant successful healing rate differences (P<0.05), which are not shown in the Tables. A detailed description of the two failed EMS cases is given in Table 9.
Full table
Full table
Discussion
This retrospective study included a relatively strict study design. To ensure the reliability of the variables and outcome data, pre-operative diagnosis and follow-up time were stipulated, and a consistency test was applied to assess intra-examiner and inter-examiner reproducibility at several intervals during the study. The limitation of this study was that it was a single-center study, and the results need to be verified by further investigation.
Studies have shown that the greatest decrease in lesion size occurred immediately after treatment (19). At least 89% of all healing roots showed signs of healing 1 year after RCT (20) and this figure was 95% for AS (21). Therefore, we choose 1 year as the shortest follow-up period, which was also suggested by Wu (22).
There is no unified evaluation standard for RCT and EMS. Both RCT and EMS have strict and loose radiographic standards. For RCT, either strict (complete resolution of existing periapical radiolucency at recall) or loose (reduction in size of existing periapical radiolucency at recall) radiographic criteria were used (23,24). For AS, Rud (25) and Molven proposed four radiographic classifications: complete healing, incomplete healing, uncertain healing and unsatisfactory healing. With regard to the strict criteria, success was defined as complete or incomplete healing, whereas uncertain or unsatisfactory healing was defined as failure (26,27). However, 65% of cases with uncertain healing at 1-year-recall were considered successful (complete or incomplete healing) at later recall (28). In addition, the discrepancies between the repeated readings were almost always between incomplete healing and uncertain healing (25). Therefore, a loose standard defined incomplete and uncertain healing as improved or partial healing, which is also widely accepted and used by researchers (7,29). Due to the anatomical complexity of the root canal system, debridement is relatively limited in AP treatment, and teeth with previous RCT without signs of periapical radiolucency also harbor microorganisms (30). As healing of AP depends on the reaction of the host immune system to the remaining microorganisms in the root canal system or around the root apex (31), smaller lesions mean that the host immune system has an advantage over the remaining microorganisms without any adverse effects on systemic health (32). Therefore, in order to evaluate the outcome of RCT and EMS using a unified method in this study, loose criteria (a decrease in the size of the periapical radiolucency) was selected as the successful radiographic criterion. Although there is an increased risk of VRF after RCT (33), the presence of VRF may occur in non-endodontically treated teeth (34,35). A retrospective study confirmed that VRF in non-endodontically treated teeth is not uncommon and constitutes 40% in Chinese patients (36). Therefore, VRF cases were not classified as failure in the present study. Similarly, VRF cases were not classified as failure in the study by Huang and in the study by Zandi (8,37).
Due to the advantages of low price, low radiation dose and easy accessibility, PA had been widely used by researchers to evaluate the outcome of RCT. However, radiographic images are two-dimensional, preventing the detection of buccolingual lesion expansions. In teeth, where the reduction in size of the existing radiolucency was diagnosed by radiographs and considered to represent periapical healing, enlargement of the lesion was frequently confirmed by cone-beam computed tomography (CBCT) (38,39). CBCT could detect the change in periapical lesions more accurately than PA (40-42). Due to the limitation of the lack of CBCT in this retrospective cohort study, CBCT will be used as the radiographic method to evaluate outcome in our prospective study.
The overall success of AP treatment by RCT and EMS was 73.8% in this study. No previous studies have investigated the overall outcome of AP regardless of treatment options. The success of RCT was 70.7%, which is consistent with the success rate reported in previous studies which varied from 53.6% to 87.8% (3-5). Discrepancies among the studies were probably due to differences in the data composition, clinical procedures, and the methodology in different studies. In the present study, not all RCTs were completed by endodontic specialists, and 103 cases were completed by general dentists. In addition, 97 of 229 cases underwent unqualified treatment, which may be one of the reasons for the relatively low success of RCT in this study. In addition, in this retrospective study, only teeth with more than 1-year-follow-up data were included. Those with non-included teeth may have refused review due to the absence of symptoms. As a result, the exclusion of these cases may also have contributed to the lower success rate of RCT.
It was shown that there was no significant difference in outcome following initial RCT (68.1%) and re-RCT (77.8%) for AP. Most studies comparing the success of initial RCT and re-RCT showed that the success of initial RCT was higher than that of re-RCT (10-12), and one study showed no difference between initial RCT and re-RCT (5). However, these studies focused on pulpal and periapical diseases, and no previous studies have investigated the outcome of initial RCT and re-RCT for AP. In theory, re-RCT was more challenging than initial RCT for the following reasons. First, re-RCT was found to significantly damage the root and result in cracks and fractures (43). Second, preexisting root canal filling materials, posts and separated files can limit the penetration of disinfectants and removal of contaminated root canal material, which is important but challenging (44). Finally, persistent infection involves more diverse bacterial communities than those detected in primary infection (45). The findings in this study may be attributable to the substantially large proportion of cases with unqualified endodontic treatment history, as 55 cases had an unqualified endodontic treatment history out of a total of 63 re-RCT cases. These re-RCT cases may respond to chemo-mechanical debridement similar to initial RCT cases (5). A much larger sample size is required to verify these results.
For AP treated by RCT, age, incomplete tooth fracture, crown root ratio, doctor classification and unqualified treatment had a strong impact on determining outcome. The results suggested that the outcome of RCT was influenced by age, in contrast to the findings in the majority of other studies (46). However, these studies involved RCT of pulp and periapical diseases, rather than AP. The success of AP is lower than that without periapical lesions (5,10), and the healing of bone defects of AP requires involvement of the body, and is related to age and systemic conditions. This may explain the difference in the results between this study and other studies in terms of age as a prognostic factor.
The effect of crown root ratio was analyzed as a continuous variable and was found to have a significant influence (OR =1.198; CI: 1.019, 1.408) on the success of total RCT. Few previous studies have examined the effect of this factor on outcome. Greater crown root ratio is usually associated with the presence of periodontal bone destruction and periodontal infection. As the periodontal pocket and pulp are communicated by the lateral root canal, dentin tubule and anatomical abnormalities, affected teeth with periodontal pockets are more likely to have microleakage of periodontal infection into the root canal system, leading to the failure of AP treatment (47). In some teeth with severe alveolar bone resorption, another possible route is the direct spread of marginal inflammation to the apical area, which causes treatment failure of AP. In addition, when the crown root ratio is greater, the periapical tissues will be subjected to greater stress due to the lever principle during mastication, which may affect the healing of periapical lesions (48). Therefore, active treatment of periodontitis and improvement of crown root ratio may be helpful in the prognosis of AP.
Incomplete tooth fracture may contribute to the lower success rate of RCT compared to those without cracks (OR =7.082; CI: 1.516, 33.089). Few studies have investigated the effect of cracks on outcome of AP treatment. In incomplete fractured teeth, bacteria remain in the crack and cannot be eliminated without removing the dental hard tissue surrounding the crack. In deep cracks this is not possible and the cracks become channels for leakage of bacteria that can lead to treatment failure of AP (49).
The quality of RCT according to post-treatment PA on outcome has been studied. The failure of unqualified-treated teeth was 2.841 times that of well-treated teeth, a finding also reported by a number of other studies (50,51). With qualified treatment this means better infection control during treatment, which could directly affect the prognosis of AP. This suggested the importance of “accurate filling” on post-treatment radiography.
The failure in teeth treated by a general dentist was 2.16 times that following treatment by an endodontic specialist. These findings are in agreement with those in previous studies, and showed that outcomes are influenced by the operator’s experience (52,53). This is particularly true for teeth with a more complex anatomy, such as molars, and healing appear to be higher if treated by endodontic specialists (52).
The prognostic factor in initial RCT for AP was crown root ratio, while the prognostic factor in re-RCT for AP was unqualified treatment. This means that qualified treatment in re-RCT has a greater impact on outcome than that in initial RCT. Considering the greater difficulties in re-RCT cases mentioned above, a decrease in the lesion size may be more difficult to achieve if unqualified treatment of re-RCT is performed. In addition, unqualified treatment during re-RCT was often related to defects from a previous RCT that failed to be corrected, such as root canal obstruction, ledge or instrument separation, which are associated with the persistence of AP. As a result, unqualified treatment in re-RCT appears to be more strongly associated with treatment failure.
In this study, the success of EMS was 94.1%, which is similar to that observed in a recent systematic review that reported a success rate of 92% based on eleven studies of EMS (54). The univariate analysis showed that none of the variables were significantly related to treatment outcome. The small sample size may be the reason for these negative results. Thus, only the descriptive results of the EMS group are provided. Prospective studies will be carried out to increase the sample size in order to clarify the prognostic factors of initial EMS versus EMS with failed RCT.
In conclusion, for AP treated by RCT, age, incomplete tooth fracture, crown root ratio, doctor classification and unqualified treatment had a strong impact on determining outcome. For initial RCT, crown root ratio was a significant outcome predictor, while for re-RCT, unqualified treatment was a strong statistically significant factor. No significant difference was found between the success of initial RCT and re-RCT for AP.
Acknowledgments
Funding: This work was supported by Clinical Cohort Construction Program of Peking University Third Hospital No. BYSYDL2019011.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-2507
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-2507
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-2507). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Medical Science Research Ethics Committee of Peking University Third Hospital (No. 2020/142-03) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Nair PN. On the causes of persistent apical periodontitis: a review. Int Endod J 2006;39:249-81. [Crossref] [PubMed]
- Georgiou AC, Crielaard W, Armenis I, et al. Apical Periodontitis Is Associated with Elevated Concentrations of Inflammatory Mediators in Peripheral Blood: A Systematic Review and Meta-analysis. J Endod 2019;45:1279-95.e3. [Crossref] [PubMed]
- Restrepo-Restrepo FA, Canas-Jimenez SJ, Romero-Albarracin RD, et al. Prognosis of root canal treatment in teeth with preoperative apical periodontitis: a study with cone-beam computed tomography and digital periapical radiography. Int Endod J 2019;52:1533-46. [Crossref] [PubMed]
- Chércoles-Ruiz A, Sanchez-Torres A, Gay-Escoda C. Endodontics, Endodontic Retreatment, and Apical Surgery Versus Tooth Extraction and Implant Placement: A Systematic Review. J Endod 2017;43:679-86. [Crossref] [PubMed]
- Ng YL, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: part 1: periapical health. Int Endod J 2011;44:583-609. [Crossref] [PubMed]
- Torabinejad M, Landaez M, Milan M, et al. Tooth retention through endodontic microsurgery or tooth replacement using single implants: a systematic review of treatment outcomes. J Endod 2015;41:1-10. [Crossref] [PubMed]
- Chan S, Glickman GN, Woodmansey KF, et al. Retrospective Analysis of Root-end Microsurgery Outcomes in a Postgraduate Program in Endodontics Using Calcium Silicate-based Cements as Root-end Filling Materials. J Endod 2020;46:345-51. [Crossref] [PubMed]
- Huang S, Chen NN, Yu V, et al. Long-term Success and Survival of Endodontic Microsurgery. J Endod 2020;46:149-57.e4. [Crossref] [PubMed]
- Goldberg F, Cantarini C, Alfie D, et al. Relationship between unintentional canal overfilling and the long-term outcome of primary root canal treatments and nonsurgical retreatments: a retrospective radiographic assessment. Int Endod J 2020;53:19-26. [Crossref] [PubMed]
- Imura N, Pinheiro ET, Gomes BP, et al. The outcome of endodontic treatment: a retrospective study of 2000 cases performed by a specialist. J Endod 2007;33:1278-82. [Crossref] [PubMed]
- Sjogren U, Hagglund B, Sundqvist G, et al. Factors affecting the long-term results of endodontic treatment. J Endod 1990;16:498-504. [Crossref] [PubMed]
- Friedman S, Lost C, Zarrabian M, et al. Evaluation of success and failure after endodontic therapy using a glass ionomer cement sealer. J Endod 1995;21:384-90. [Crossref] [PubMed]
- Ng YL, Mann V, Gulabivala K. Outcome of secondary root canal treatment: a systematic review of the literature. Int Endod J 2008;41:1026-46. [Crossref] [PubMed]
- . Guidelines for root canal treatment. Zhonghua Kou Qiang Yi Xue Za Zhi 2014;49:272-4. [PubMed]
- Kim S, Kratchman S. Modern endodontic surgery concepts and practice: a review. J Endod 2006;32:601-23. [Crossref] [PubMed]
- Orstavik D, Kerekes K, Eriksen HM. The periapical index: a scoring system for radiographic assessment of apical periodontitis. Endod Dent Traumatol 1986;2:20-34. [Crossref] [PubMed]
- Schneider SW. A comparison of canal preparations in straight and curved root canals. Oral Surg Oral Med Oral Pathol 1971;32:271-5. [Crossref] [PubMed]
- Patil K, Khalighinejad N, El-Refai N, et al. The Effect of Crown Lengthening on the Outcome of Endodontically Treated Posterior Teeth: 10-year Survival Analysis. J Endod 2019;45:696-700. [Crossref] [PubMed]
- Zhang MM, Liang YH, Gao XJ, et al. Management of Apical Periodontitis: Healing of Post-treatment Periapical Lesions Present 1 Year after Endodontic Treatment. J Endod 2015;41:1020-5. [Crossref] [PubMed]
- Orstavik D. Time-course and risk analyses of the development and healing of chronic apical periodontitis in man. Int Endod J 1996;29:150-5. [Crossref] [PubMed]
- Molven O, Halse A, Grung B. Incomplete healing (scar tissue) after periapical surgery--radiographic findings 8 to 12 years after treatment. J Endod 1996;22:264-8. [Crossref] [PubMed]
- Wu MK, Wesselink P, Shemesh H. New terms for categorizing the outcome of root canal treatment. Int Endod J 2011;44:1079-80. [Crossref] [PubMed]
- de Chevigny C, Dao TT, Basrani BR, et al. Treatment outcome in endodontics: the Toronto study--phase 4: initial treatment. J Endod 2008;34:258-63. [Crossref] [PubMed]
- Azim AA, Griggs JA, Huang GT. The Tennessee study: factors affecting treatment outcome and healing time following nonsurgical root canal treatment. Int Endod J 2016;49:6-16. [Crossref] [PubMed]
- Rud J, Andreasen JO, Jensen JE. Radiographic criteria for the assessment of healing after endodontic surgery. Int J Oral Surg 1972;1:195-214. [Crossref] [PubMed]
- Schloss T, Sonntag D, Kohli MR, et al. A Comparison of 2- and 3-dimensional Healing Assessment after Endodontic Surgery Using Cone-beam Computed Tomographic Volumes or Periapical Radiographs. J Endod 2017;43:1072-9. [Crossref] [PubMed]
- von Arx T, Jensen SS, Hanni S, et al. Five-year longitudinal assessment of the prognosis of apical microsurgery. J Endod 2012;38:570-9. [Crossref] [PubMed]
- Rud J, Andreasen JO, Jensen JE. A follow-up study of 1,000 cases treated by endodontic surgery. Int J Oral Surg 1972;1:215-28. [Crossref] [PubMed]
- von Arx T, Janner S, Hanni S, et al. Radiographic Assessment of Bone Healing Using Cone-beam Computed Tomographic Scans 1 and 5 Years after Apical Surgery. J Endod 2019;45:1307-13. [Crossref] [PubMed]
- Molander A, Reit C, Dahlen G, et al. Microbiological status of root-filled teeth with apical periodontitis. Int Endod J 1998;31:1-7. [Crossref] [PubMed]
- Wang J, Chen W, Jiang Y, et al. Imaging of extraradicular biofilm using combined scanning electron microscopy and stereomicroscopy. Microsc Res Tech 2013;76:979-83. [Crossref] [PubMed]
- Wu MK, Wesselink P, Shemesh H. New terms for categorizing the outcome of root canal treatment. Int Endod J 2011;44:1079-80. [Crossref] [PubMed]
- Wu MK, van der Sluis LW, Wesselink PR. Comparison of mandibular premolars and canines with respect to their resistance to vertical root fracture. J Dent 2004;32:265-8. [Crossref] [PubMed]
- Liao WC, Tsai YL, Wang CY, et al. Clinical and Radiographic Characteristics of Vertical Root Fractures in Endodontically and Nonendodontically Treated Teeth. J Endod 2017;43:687-93. [Crossref] [PubMed]
- Chan CP, Tseng SC, Lin CP, et al. Vertical root fracture in nonendodontically treated teeth--a clinical report of 64 cases in Chinese patients. J Endod 1998;24:678-81. [Crossref] [PubMed]
- Chan CP, Lin CP, Tseng SC, et al. Vertical root fracture in endodontically versus nonendodontically treated teeth: a survey of 315 cases in Chinese patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;87:504-7. [Crossref] [PubMed]
- Zandi H, Petronijevic N, Mdala I, et al. Outcome of Endodontic Retreatment Using 2 Root Canal Irrigants and Influence of Infection on Healing as Determined by a Molecular Method: A Randomized Clinical Trial. J Endod 2019;45:1089-98.e5. [Crossref] [PubMed]
- Wu MK, Shemesh H, Wesselink PR. Limitations of previously published systematic reviews evaluating the outcome of endodontic treatment. Int Endod J 2009;42:656-66. [Crossref] [PubMed]
- Garcia de Paula-Silva FW, Hassan B, Bezerra DSL, et al. Outcome of root canal treatment in dogs determined by periapical radiography and cone-beam computed tomography scans. J Endod 2009;35:723-6. [Crossref] [PubMed]
- de Paula-Silva FW, Wu MK, Leonardo MR, et al. Accuracy of periapical radiography and cone-beam computed tomography scans in diagnosing apical periodontitis using histopathological findings as a gold standard. J Endod 2009;35:1009-12. [Crossref] [PubMed]
- Kanagasingam S, Lim CX, Yong CP, et al. Diagnostic accuracy of periapical radiography and cone beam computed tomography in detecting apical periodontitis using histopathological findings as a reference standard. Int Endod J 2017;50:417-26. [Crossref] [PubMed]
- Liang YH, Jiang L, Gao XJ, et al. Detection and measurement of artificial periapical lesions by cone-beam computed tomography. Int Endod J 2014;47:332-8. [Crossref] [PubMed]
- Shemesh H, Roeleveld AC, Wesselink PR, et al. Damage to root dentin during retreatment procedures. J Endod 2011;37:63-6. [Crossref] [PubMed]
- Mollo A, Botti G, Prinicipi GN, et al. Efficacy of two Ni-Ti systems and hand files for removing gutta-percha from root canals. Int Endod J 2012;45:1-6. [Crossref] [PubMed]
- Tzanetakis GN, Azcarate-Peril MA, Zachaki S, et al. Comparison of Bacterial Community Composition of Primary and Persistent Endodontic Infections Using Pyrosequencing. J Endod 2015;41:1226-33. [Crossref] [PubMed]
- Shakiba B, Hamedy R, Pak JG, et al. Influence of increased patient age on longitudinal outcomes of root canal treatment: a systematic review. Gerodontology 2017;34:101-9. [Crossref] [PubMed]
- Rupf S, Kannengiesser S, Merte K, et al. Comparison of profiles of key periodontal pathogens in periodontium and endodontium. Endod Dent Traumatol 2000;16:269-75. [Crossref] [PubMed]
- de Souza RS, Gandini LJ, de Souza V, et al. Influence of orthodontic dental movement on the healing process of teeth with periapical lesions. J Endod 2006;32:115-9. [Crossref] [PubMed]
- Haapasalo M, Shen YA, Ricucci D. Reasons for persistent and emerging post-treatment endodontic disease. Endodontic Topics 2011;18:31-50. [Crossref]
- Liang YH, Li G, Shemesh H, et al. The association between complete absence of post-treatment periapical lesion and quality of root canal filling. Clin Oral Investig 2012;16:1619-26. [Crossref] [PubMed]
- Nascimento EH, Gaeta-Araujo H, Andrade M, et al. Prevalence of technical errors and periapical lesions in a sample of endodontically treated teeth: a CBCT analysis. Clin Oral Investig 2018;22:2495-503. [Crossref] [PubMed]
- Burry JC, Stover S, Eichmiller F, et al. Outcomes of Primary Endodontic Therapy Provided by Endodontic Specialists Compared with Other Providers. J Endod 2016;42:702-5. [Crossref] [PubMed]
- Hamasha AA, Hatiwsh A. Quality of life and satisfaction of patients after nonsurgical primary root canal treatment provided by undergraduate students, graduate students and endodontic specialists. Int Endod J 2013;46:1131-9. [Crossref] [PubMed]
- Kang M, In JH, Song M, et al. Outcome of nonsurgical retreatment and endodontic microsurgery: a meta-analysis. Clin Oral Investig 2015;19:569-82. [Crossref] [PubMed]


