
Clinical application of NRS-2002 in nutritional risk screening of tuberculosis inpatients
Introduction
Tuberculosis (TB) is an infectious disease with high incidence and high burden. China has the second highest TB burden in the world and TB case numbers predominate statutory reports of Class A and Class B infectious diseases. In China, the prevalence of TB in the western region is higher than that of the central and eastern regions, and is also higher than the national average (1). Malnutrition and low immune function are leading factors in the development and progression TB in this population. Studies have confirmed that the incidence of nutritional risk in TB inpatients is much higher than that of other inpatients. The exacerbation of the nutritional risk status in TB patients during hospitalization may increase the incidence of complications, mortality and prolong the length of hospital stay (2).
The definition of nutritional risk from the European Society of Parenteral and Enteral Nutrition is “existing or potential nutritional and metabolic conditions caused by diseases or related clinical outcomes after surgery”. At present, there are many clinical screening methods for nutritional risk. The Chinese Medical Association Parenteral and Enteral Nutrition Branch recommends the application of the nutritional risk screening 2002 (NRS-2002) system as the preferred screening tool for nutritional status evaluation (3).
In this study, the NRS-2002 was used to screen for nutritional risk in inpatients with TB, assess the incidence of nutritional risk, and analyze the impact of nutritional risk on the complications and length of hospital stay, with an ultimate aim of providing appropriately targeted clinical interventions. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-21-610).
Methods
General information
A total of 295 inpatients with TB admitted to the Infectious Diseases Department at Suining Central Hospital from January 1, 2018 to June 30, 2018 were enrolled in the study. Inclusion criteria were: (I) inpatients diagnosed with TB (in line with the People’s Republic of China Health Industry Standards WS288-2017 “Diagnosis of Tuberculosis” and WS196-2017 “Classification of Tuberculosis” issued in 2017); (II) age ≥18 years. Exclusion criteria were: (I) patients who did not receive anti-TB treatment; (II) patients who were hospitalized for less than 1 week; (III) patients who died during hospitalization. A total of 295 cases, including 242 male and 53 female patients, with a male to female ratio of approximately 4.57:1. The patients were aged 24–65 years, with an average age of 42 years. The study was approved by the Research Ethics Committee of Suining Central Hospital (2017-18). All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). Informed consent was taken from all the patients.
Grouping criteria and study indexes
Inpatients who met the inclusion criteria were screened for nutritional risk within 2 days of admission using the NRS-2002. Patients with NRS-2002 score ≥3 were assessed as being at nutritional risk; however, this study did not interfere with the specific clinical treatment decisions and nutritional support provided to patients. After screening, these patients were divided into group A (nutritional risk group) and group B (non-nutritional risk group). Information including the subtype of TB, comorbid diseases, body mass index (BMI), serum albumin (ALB), complications, and length of hospital stay of participants was also collected. Patients who did not receive anti-TB treatment or were hospitalized for less than 1 week were excluded.
Statistical analysis
The final data was processed using SPSS 25.0 statistical software (IBM, New York, USA). Measurement data subjected to normal distribution analysis were expressed as mean ± standard deviation, and analyzed using a Student’s t-test to compare between groups. Measurement data not subjected to normal distribution analysis were described using median and interquartile range, and analyzed using a Wilcoxon rank-sum test to compare between groups. Count data was expressed as a pass rate or composition ratio, and analyzed using a chi-squared test. Results with P<0.05 were considered statistically significant.
Results
Comparison of patients’ baseline conditions
In this study, a total of 295 patients were enrolled: group A (nutritional risk group) consisted of 190 cases with NRS-2002 score ≥3, and group B (non-nutritional risk group) consisted of 105 cases with NRS-2002 score <3. The prevalence of total nutritional risk was 64.41%. There were 246 cases of simple pulmonary TB, and 49 cases of extrapulmonary TB with or without pulmonary TB. The average BMI of all patients was 19.85±2.02 kg/m2, and the average ALB was 35.12±5.40 g/L. Regarding comorbidities, 124 patients (42.03%) had either comorbid lung diseases (such as lung parenchyma damage, asthma, pneumoconiosis, bronchiectasis, and COPD) or other organ dysfunction or serious disease (such as AIDS, coronary heart disease, heart failure, cerebral infarction, systemic lupus erythematosus, diabetes, severe anemia, cachexia). There were 38 patients with diabetes, accounting for 12.88% of all patients.
Among the 190 patients in the nutritional risk group, there were 158 males and 32 females, with an age range of 28–65 years old (average age 52 years) and average BMI was 19.15±2.01 kg/m2. In the nutritional risk group, 149 patients had simple TB and 41 had extrapulmonary TB with or without pulmonary TB; 105 patients had underlying diseases (including 31 patients with diabetes) and 85 patients did not have underlying diseases. Among 105 patients in the non-nutritional risk group, there were 84 males to and 21 females, with an age range of 24–45 years old (average age 31 years) and average BMI of 21.13±1.28 kg/m2. In this group, there were 97 patients with simple TB and 8 patients with extrapulmonary TB with or without pulmonary TB; 19 patients had underlying diseases (including 7 patients with diabetes) and 86 patients did not have underlying diseases. Details are shown in Table 1.
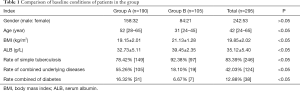
Full table
Comparison of clinical conditions of patients after admission
The average length of hospital-stay of all patients enrolled in the study was 17.07±7.04 days. Among them, 163 patients (55.25%) had complications during their hospitalization, including secondary infection, respiratory failure, pneumothorax, hemoptysis, and hypohepatia. Of these complications, secondary infections and hypohepatia were most common, with a total of 127 patients (43.05%) developing secondary infections and a total of 40 patients (13.56%) developing hypohepatia during hospitalization.
The average hospital-stay of the nutritional risk group was 19.55±7.33 days. In this group, 133 patients (70%) had complications during hospitalization, 107 patients (56.31%) had secondary infections, and 31 patients (16.32%) developed hypohepatia. In the non-nutrition risk group, the average hospital stay was 12.60±3.34 days. In this group, 30 cases (28.57%) developed complications, 20 patients (19.05%) developed secondary infections, and 9 patients (8.57%) developing hypohepatia. The differences between the above two groups of patients for various indicators were statistically significant (Table 2).
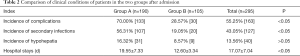
Full table
Conclusions
Incidence of nutritional risk among hospitalized TB patients was 64.41%. Men were more likely to have nutritional risk than women (65.20% vs. 60.28%); however, this difference was not statistically significant. Older patients were more likely to be at nutritional risk; patients with lower BMI and ALB levels were also more likely to be at nutritional risk. Compared with simple TB cases, patients with extrapulmonary TB with or without pulmonary TB had a higher incidence of nutritional risk (83.67% vs. 60.57%). The incidence of nutritional risk in patients with underlying diseases was also higher than that of patients without underlying disease (84.68% vs. 49.71%). The incidence of nutritional risk in patients with both diabetes and TB was higher than that of patients only with TB (81.58% vs. 61.87%) that there were 31 cases with nutritional risk among the 38 cases with both diabetes and TB.
Patients with longer hospital stays were also more likely to be at nutritional risk and the incidence of complications in the nutritional risk population (70%) was higher than that of seen in the non-nutritional risk group (28.57%). Among all patients, there were 127 patients with secondary infections, with an incidence rate of 43.05%. Notably, the incidence of secondary infections in patients with nutritional risk was higher than that of patients without nutritional risk (56.31% vs. 19.05%). In the total study population, there were 40 patients with hypohepatia (13.56%); the incidence of hypohepatia in patients with nutritional risk was higher than that of patients without nutritional risk (16.32% vs. 8.57%) but this difference was not statistically significant. In general, patients with nutritional risk had an increased incidence of complications and longer hospital stays.
Discussion
TB is one of the common infectious diseases in the western region of China. Patients with TB often suffer from decreased appetite and gastrointestinal disorders, resulting in insufficient nutrient intake and decreased anabolism. In addition, protein in the body could be metabolized by Mycobacterium TB, which increases catabolism; and this continuous excretion of toxins forms pathogenic bacteria, resulting in night sweats, fever, and weight loss. Ultimately, TB causes an increase in the body’s catabolism, damages of the body’s nutritional and energy status, and causes protein malnutrition and other conditions.
In recent years, the incidence of TB has continued to rise and clinical studies in this population have also increased. Therefore, the nutritional status of TB patients has gradually received more attention. The NRS-2002, a screening tool for nutritional risk, is often used to assess for malnutrition in hospitalized patients and potential risk of developing malnutrition. NRS-2002 screening does not require additional blood samples to be collected, is simple and easy to administer, and has a high predictive value for nutritional status in hospitalized patients (4-6). Therefore, it is an important tool to assess whether hospitalized patients with various diseases have nutritional risk and whether they need additional nutritional intervention (7).
This study confirmed that nutritional risk is common in hospitalized TB patients, with an incidence of 64.41%, similar to that reported in previous literatures (54.24–86.25%) (8-11). Patients with increased age, lower BMI or lower ALB values have a higher incidence of nutritional risk. The incidence of nutritional risk is higher in patients with underlying disease, and is more common in patients with comorbid diabetes. And the common complications include chronic obstructive pulmonary disease, bronchiectasis, pneumoconiosis, diabetes mellitus, hypertension, coronary heart disease, alcoholic liver disease, hepatitis B carriers, chronic hepatitis, autoimmune diseases, and other chronic disease. Accurate diagnosis of the complications is of great significance to the judgment of the basic condition of tuberculosis patients, and also has certain guiding value to the treatment of tuberculosis patients. For example, patients with basic pulmonary diseases (such as chronic obstructive pulmonary disease, bronchiectasis, and pneumoconiosis) who are infected with tuberculosis are more likely to suffer from respiratory failure, pneumothorax, hemoptysis and other complications. Patients with autoimmune disease may be affected by the treatment of autoimmune disease drugs (such as hormones and immunosuppressants); Patients with chronic liver disease are at greater risk of drug-induced liver injury during anti-TB treatment. And among these comorbidities, the combination of diabetes has a significant impact on the nutritional status of TB patients. There are reports indicating that diabetes patients with insulin resistance, hyperglycemia, nutrient metabolism disorders, and decreased lymphocyte immune function are more vulnerable to developing pulmonary TB. Therefore, these patients are often prone to be malnourished due to diet, and needs more specific dietary guidance and nutritional support to correct their malnutrition status. Given the indicators used by NRS-2002 to assess nutritional risk include disease status, nutritional status (including measures of eating, weight loss, BMI, ALB), and age, it is suggested that NRS-2002 is well-designed to assess the nutritional risk of TB inpatients.
Patients with extrapulmonary TB had a higher incidence of nutritional risk, which may have been due to that the severity of the types of extrapulmonary TB that were observed in this study population—including tuberculous meningitis, abdominal TB, tuberculous pericarditis, spinal TB, and other serious conditions—and that many patients presented with combinations of TB, especially with hematogenous pulmonary TB. Patients with these types of TB often eat less but can consume more nutrition than patients with simple TB due to serious TB poisoning symptoms. Among tuberculosis patients, the more severe patients diagnosed by imaging findings, the higher rate of nutritional risk. The common imaging characteristics include invasive pulmonary tuberculosis, pneumonia, tuberculosis, cheese balls, chronic damaged fiber cavity tuberculosis, lung and blood line disseminated tuberculosis, primary pulmonary tuberculosis, and other tuberculosis. In these types of tuberculosis, it seems that patients will get higher rate of nutritional risk when they are suffered from cheese pneumonia, chronic damaged fiber cavity tuberculosis, lung and blood line disseminated tuberculosis. However, this conclusion still remains to be further studied.
TB patients are prone to get various complications during hospitalization, such as secondary bacterial infection, hypohepatia, respiratory failure, pneumothorax, and hemoptysis. Patients with nutritional risk have a higher incidence of complications during hospitalization. The occurrence of these complications may be related to the underlying diseases, nutritional status, drug use and other factors of the patients. In this study, the incidence of complications during hospitalization in TB patients was 55.25%, which may be related to the fact that patients with mild TB are mostly treated in outpatient clinics rather than an inpatient setting. Secondary infections are common complications for TB inpatients, including secondary bacterial and fungal infections. In this study, the incidence of secondary infections was 43.05%, which is similar to previous literature (12). Secondary bacterial and/or fungal infections in TB patients may aggravate the existing pulmonary lesions and impair lung function, and the infections of some patients may be neglected and delayed for treatment due to immunodeficiency and atypical symptoms. In addition, as a result of pulmonary cavity lesions characteristic, the infection may be not easy to control. Therefore, powerful anti-infection treatment must be conducted, especially for patients with secondary fungus infection, appropriate antifungal drugs need to be used according to fungal species (such as fluconazole, voriconazole, mooring Finn net card, amphotericin B), with sufficient courses of treatment. Inevitably, some adverse drug reactions may occur and even affect the treatment of tuberculosis. The incidence of secondary infections in patients with nutritional risk is higher than those without nutritional risk, which suggests that improving the nutritional status of patients may reduce the risk of secondary infections in TB patients. Hypohepatia is a common complication seen in TB patients undergoing anti-TB chemotherapy. This study noted that the incidence of hypohepatia in patients with nutritional risk was higher than that in patients without nutritional risk; however, this difference was not statistically significant and a larger sample size or follow-up period is required to further explore this relationship. Studies have shown that patients with malnutrition are prone to liver ischemia and hypoxia, as well as hepatocyte necrosis (13,14). The hepatic impairment in TB patients is related to host genetic factors (such as drug metabolism enzymes, drug transporter, oxidation reaction and the immune response), host non-genetic factors (such as age, history of liver disease, malnutrition, history of alcoholism, severe tuberculosis), drug interactions, and other factors. The innate mechanism is not entirely clear, mainly related to drug metabolism, mitochondrial damage, immune function damage and abnormal factors, which can be usually summarized as the direct toxic effect of TB drugs and specificity acetaminophen-mediated hepatotoxicity. However, malnutrition patients are prone to liver ischemia and hypoxia and liver cell necrosis (15), which leads to a higher risk of drug-induced liver injury. The mild cases of drug-induced liver injury are manifested as transient transaminase increase, while the severe cases can suffer from liver failure and even threaten life. Therefore, anti-tuberculosis treatment has to be stop for some patients. Clinical studies have confirmed that drug-induced liver injury in the process of anti-tuberculosis treatment will reduce the success rate of treatment and delay the outcome of the disease. Among these predisposing factors of liver injury, malnutrition is easy to intervene. Results in this study indicate that the incidence of hypohepatia in TB patients may be reduced by improving the nutritional status of patients, which could result in less-interrupted treatment plans for TB patients. However, this study only observed the occurrence of hypohepatia in TB patients during hospitalization—that is, short-term rather than long-term incidence of hypohepatia—and longer follow-up observation is required to better understand how this may affect patient treatment.
Additionally, due to the long-term observation required to assess the efficacy of anti-TB chemotherapy, the final clinical outcome of patients with tuberculosis, and the multifactorial nature of treatment efficacy (including considerations of drug resistance and medication compliance). Although the conclusions of this study are limited, the results indicate that patients at nutritional risk in this study had longer hospital stays, more complications, and a poorer short-term prognosis. Therefore, future studies should include regular nutritional risk assessment for TB outpatients to further explore the correlation in patients’ nutritional status, the treatment efficacy, long-term prognosis and final clinical outcome
Results of this study showed that TB patients have a high incidence of nutritional risk. Patients with increased age, lower BMI, and comorbidities had a higher incidence of nutritional risk, which was associated with more complications and longer hospital stays. These findings suggest that nutritional status of TB inpatients is related to the disease progression and prognosis. For patients with nutritional risk, there is limited potential to improve their nutritional risk during a brief inpatient admission, thus future research should investigate inpatient interventions that could assist patients to improve their nutritional status after hospitalization and reduce nutritional risks in the long-term. Previous clinical studies have shown that the nutritional risk ratio of TB patients at discharge or 2 weeks after admission is higher than that at admission (8), potentially increasing the risk of complications and reducing quality of life for TB patients. Clinically, the nutritional support rate for TB patients is very low (8), and the lack of attention placed on this aspect of TB patient care could explain the low rate of potentially appropriate interventions, including enteral nutrition; nutritional support also has important implications for other aspects of patient care, including rehabilitation. In follow-up studies, we will continue to analyze the nutritional support of TB patients during hospitalization and evaluate ways of providing appropriate nutritional support where clinically indicated, in order to improve the nutritional status of the patients, reduce incidence of complications, shorten hospital stay, improve prognosis, and provide a stronger scientific basis for nutritional support strategies in this population.
Acknowledgments
Funding: This study was kindly approved by Sichuan Medical Research Youth Innovation Project (Q17077).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-21-610
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-21-610
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-21-610). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the Research Ethics Committee of Suining Central Hospital (2017-18). All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). Informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yang C, Gao Q. Recent transmission of Mycobacterium tuberculosis in China: the implication of molecular epidemiology for tuberculosis control. Front Med 2018;12:76-83. [Crossref] [PubMed]
- Hayashi S, Takeuchi M, Hatsuda K, et al. The impact of nutrition and glucose intolerance on the development of tuberculosis in Japan. Int J Tuberc Lung Dis 2014;18:84-8. [Crossref] [PubMed]
- Wang F, Chen W, Bruening KS, et al. Nutrition Screening Tools and the Prediction of Clinical Outcomes among Chinese Hospitalized Gastrointestinal Disease Patients. PLoS One 2016;11:e0159436 [Crossref] [PubMed]
- Kyle UG, Kossovsky MP, Karsegard VL, et al. Comparison of tools for nutritional assessment and screening at hospital admission: a population study. Clin Nutr 2006;25:409-17. [Crossref] [PubMed]
- Barbosa AAO, Vicentini AP, Langa FR. Comparison of NRS-2002 criteria with nutritional risk in hospitalized patients. Cien Saude Colet 2019;24:3325-34. [Crossref] [PubMed]
- Miao JP, Quan XQ, Zhang CT, et al. Comparison of two malnutrition risk screening tools with nutritional biochemical parameters, BMI and length of stay in Chinese geriatric inpatients: a multicenter, cross-sectional study. BMJ Open 2019;9:e022993 [Crossref] [PubMed]
- Liu G, Zhang S, Mao Z, et al. Clinical significance of nutritional risk screening for older adult patients with COVID-19. Eur J Clin Nutr 2020;74:876-83. [Crossref] [PubMed]
- Kim HJ, Lee CH, Shin S, et al. The impact of nutritional deficit on mortality of in-patients with pulmonary tuberculosis. Int J Tuberc Lung Dis 2010;14:79-85. [PubMed]
- Lazzari TK, Forte GC, Silva DR. Nutrition Status Among HIV-Positive and HIV-Negative Inpatients with Pulmonary Tuberculosis. Nutr Clin Pract 2018;33:858-64. [Crossref] [PubMed]
- Hatsuda K, Takeuchi M, Ogata K, et al. The impact of nutritional state on the duration of sputum positivity of Mycobacterium tuberculosis. Int J Tuberc Lung Dis 2015;19:1369-75. [Crossref] [PubMed]
- Ali N, Gupta N, Saravu K. Malnutrition as an important risk factor for drug-induced liver injury in patients on anti-tubercular therapy: an experience from a tertiary care center in South India. Drug Discov Ther 2020;14:135-8. [Crossref] [PubMed]
- Tang J, Yam WC, Chen Z. Mycobacterium tuberculosis infection and vaccine development. Tuberculosis (Edinb) 2016;98:30-41. [Crossref] [PubMed]
- Sun Q, Zhang Q, Gu J, et al. Prevalence, risk factors, management, and treatment outcomes of first-line antituberculous drug-induced liver injury: a prospectivecohort study. Pharmacoepidemiol Drug Saf 2016;25:908-917. [Crossref] [PubMed]
- Singla R, Sharma SK, Mohan A, et al. Evaluation of riskfactors for antituberculosis treatment induced hepatotoxicity. Indian J Med Res 2010;132:81-86. [PubMed]
- Giordano F, Arnone S, Santeusanio F, et al. Brief elevation of hepatic enzymes due to liver ischemia in anorexia nervosa. Eat Weight Disord 2010;15:e294-7. [Crossref] [PubMed]
(English Language Editor: M. Hawkins)


