
Pathoanatomy and clinical outcomes following operative treatment of supination adduction type II medial malleolus fractures—a cohort study
Introduction
Ankle fracture is a common injury addressed by orthopedic surgeons, with an estimated 260,000 Americans sustaining an ankle fracture annually (1). However, supination adduction (SAD) ankle fracture does not present as commonly, and has been reported to comprise 4–5% of all ankle fractures (2,3). Additionally, vertical type medial malleolar fracture (MMF) has been shown to account for about 6% of all MMFs (4). Although surgical treatment with open reduction and internal fixation (ORIF) is generally the accepted form of treatment for intraarticular fractures, clinical research focused on SAD is scarce.
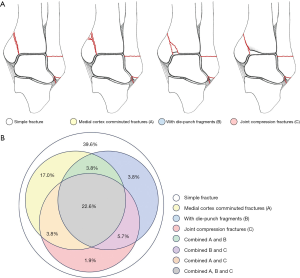
The main cause of SAD type II MMFs is vertical Violence, the injury mechanism is similar to that of pilon fractures, especially posterior pilon fracture (5-7). This type of MMF presents with relatively vertical fracture lines, and may sometimes be characterized by a proximal medial cortical comminuted fracture (Figure 1A), a die-punch fragment (Figure 1B), compression and collapse of the medial part of distal tibial articular surface (DTAS) (Figure 1C), and sometimes these characteristics may coexist. High surgical technical expertise is required for the treatment of this type of MMFs, and the internal fixation methods are controversial. A biomechanical study reported that both simple screws fixation and buttress plate fixation could attain a similar mechanical strength for this type of fracture (8), but some others have reported that the buttress plate provided better support to vertical MMFs in comparison with unicortical or bicortical screws fixation (9). To date, no clinical comparative study has been reported that has solely focused on the internal fixation methods for SAD type II MMFs. The purpose of the current study was to retrospectively clarify the anatomic characters and compare the functional outcomes and complications of pathoanatomic features and different internal fixations in the treatment of SAD type II MMFs.

We present the following article in accordance with the STROBE reporting checklist (available at https://dx.doi.org/10.21037/apm-21-1505).
Methods
All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of the Honghui Hospital Affiliated to Medical College of Xi’an Jiaotong University (No.: 20170003). Individual consent for this retrospective analysis was waived. The authors retrospectively analyzed the characteristics of SAD type II MMFs thorough X-ray and computed tomography (CT), and the outcomes of buttress plate fixation or screws fixation between March 2009 and June 2013. The inclusion criteria were as follows: (I) adults over 18 years old; (II) acute SAD type II ankle fracture; (III) MMF was treated with open reduction and buttress plate fixation or screws fixation; (IV) at least 2 years follow up. The exclusion criteria were as follows: (I) surgical fixation beyond 14 days from the time of injury; (II) grade II or III open ankle fractures according to Gustilo-Anderson classification (10); (III) combined with talus body fracture requiring fixation; (IV) pathological fractures; (V) preoperative dysfunction of the injured limb; (VI) no preoperative or follow-up X-ray and CT.
Treatment methods
For the MMFs, an anteromedial incision was made. The incision enabled a view of the anteromedial aspect of the joint, permitting accurate alignment of the fracture. For patients with a die-punch fragment, or compression and collapse of the medial part of DTAS, an anatomical reduction under direct vision from this incision was able to be achieved. Cancellous allograft was used in the case of bone defect after the DTAS reduction. Finally, the MMF was fixed either with screws (Figure 2A) or a buttress plate (Figure 2B). Then, fluoroscopy was used to ensure the reduction and positioning of the hardware.

Postoperative management
The postoperative rehabilitation protocol for all participants included active and passive motion exercises of the ankle and mid- and forefoot joints, isotonic and isometric exercises of the leg, and a night splint, commencing on the second postoperative day. Full weight-bearing (FWB) was initiated after the fracture site had reached bony union radiographically.
Radiographic and clinical evaluation
The pre-operative X-rays and CT scans were retrospectively analyzed. The characteristics of MMFs were evaluated on coronal CT scans. The medial malleolus fracture line angle (FLA) was defined as the angle between major fracture line and DTAS line (Figure 3A) on the anterior-posterior ankle X-ray. The method of DTAS% involvement on anterior-posterior ankle X-ray was calculated with the method on Figure 3B. Radiographs taken at the final follow-up time were compared with immediate postoperative radiographs for evidence of screw loosening, loss of reduction (LoR), and nonunion. LoR was defined as any shift in fracture position greater than 1 mm (Figure 3C). The final radiographs were also used to evaluate osteoarthritis; according to the van Dijk ankle osteoarthritis classification (11), stage-II and stage-III were defined as traumatic osteoarthritis (TOA) change.

The American Orthopedic Foot and Ankle Society (AOFAS) ankle-hindfoot score (12), and the visual analogue scale (VAS) were used for functional evaluation at the final follow-up time. The AOFAS scoring scale has a maximum of 100 points (>91 indicates an excellent result, 75–90= good result, 50–75= fair result, and <50= poor result). LoR was defined as any shift in fracture position greater than 2 mm. Treatment failure was defined as fracture nonunion, malunion, or fixation failure requiring reoperation. Wound complication included dehiscence, skin edge necrosis, and delayed healing.
Statistical analyses
Descriptive statistics were calculated as mean ± standard deviation (SD). Student’s t-test was used to compare differences between groups for continuous variables; Pearson’s chi-square test and Fisher’s exact test were used for comparison of dichotomous variables. The level of significance was set at P=0.05. Statistical analyses were performed with the software SPSS 17.0 (SPSS Inc., Chicago, IL, USA).
Results
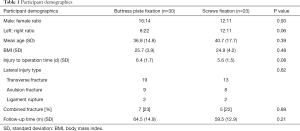
The basic informations
Total of 53 participants, with 28 males and 25 females, were included in this study. The average age was 38.5±16.1 [18–78] years. The mean follow up time was 62.4±14.1 [44–91] months. Causes of fracture included 24 falls from a height, 17 sprains, and 12 motor cycle accidents. Combined injuries included 6 fifth metatarsal base fractures, 2 Lisfranc injuries, 3 distal radius fractures, and 1 femoral shaft fracture. A total of 30 MMFs were fixed with a buttress plate, and 23 were fixed with screws. No significant difference of basic information was detected between the two groups (Table 1).
Full table
MMF characters
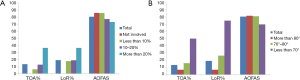
For the included patients, 21 (39.6%) cases with simple vertical MMFs; 25 (47.2%) cases with medial cortex comminuted fractures; 19 (35.8%) cases with die-punch fragments; and 18 (34.0%) cases with medial joint compression. Actually, 19 (35.8%) cases coexisted two or three of the characteristics; 2 (3.8%) cases coexisted with medial cortex comminuted fractures and die-punch fragments; 2 (3.8%) cases coexisted with medial cortex comminuted fractures and joint compression; 3 (5.7%) cases coexisted with die-punch fragments and joint compression; and 12 (22.6%) cases coexisted with the three characteristics (Figure 4).
The effects on prognosis of different MMF
The AOFAS score in patients with medial cortex comminuted fractures was significantly lower than whose patients without these characteristics (P=0.01); as well as those patients with die-punch fragments and medial joint compression (P<0.01). The LoR rate was significantly higher in patients with die-punch fragments (P=0.03); and the TOA rate was significantly higher in patients with medial joint compression (P=0.04) (Table 2).

Full table
The data about the DTAS% and FLA
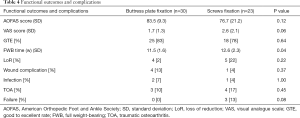
The mean DTAS% was 16.5%±11.6% (range, 0–47%). Nine (17.0%) cases without involved of DTAS; 17 (32.1%) cases involved less than 10%; 16 (30.2%) cases involved between 10% and 20%; and 11 (20.8%) cases involved more than 20%. The mean medial malleolus FLA was 80.8°±6.1° (range, 58°–90°). Thirty (56.6%) cases were with FLA more than 80°; and 19 (35.8%) cases between 70° and 80°; and 4 (7.5%) cases less than 70°.
The relationship between prognosis and the DTAS% and FLA
LoR was detected in 7 cases during follow up, along with 7 cases of TOA. The TOA incidence increased and positively correlated with the increase of DTAS% involvement, as well as the LoR incidence (Figure 5A); and the mean AOFAS decreased with the increase of DTAS% involvement. However, no significant difference was detected with the numbers available (Table 3). The TOA and LoR incidence increased and with the decrease of medial malleolus FLA (Figure 5B), and the LoR incidence was significantly increased in cases with FLA less than 70° while compared with overall mean (P=0.03). The mean AOFAS decreased with the decrease of medial malleolus FLA, but no significant difference was detected with the numbers available (Table 3).

Full table
The comparison between the buttress plate and screws fixation
The mean AOFAS ankle and hindfoot score at final follow up or before revision surgery was 80.6±15.8 [12–97] points. The mean VAS score during walking was 2.1±1.7 [0–8] points. The good to excellent rate (GTE) was 81.1% (43/53). With the numbers available, no significant difference was detected when comparing the functional outcomes between the buttress plate fixation and screws fixation groups (Table 4). However, the mean FWB time was significantly shorter in the buttress plate fixation group (P=0.04).
Full table
The complication data
There were 5 wound complications, 3 superficial infections, and all were treated conservatively without further surgical intervention. Surgical failure was diagnosed in 3 cases, all of which were fixed with screws for the MMFs. No significant difference was detected when comparing the complication rates between groups (Table 4).
Discussion
The Lauge-Hansen classification system was intended to predict mechanism of injury based on ankle fracture radiographs. Although the consistency of the Lauge-Hansen system (65%) was reported as lower than that of the AO classification system (81%) (13), all SAD injuries were correlated between videos and radiographs (13,14). Type II SAD MMFs result from forced talar adduction. Failure of the lateral side combined with a vertical axial load causes the talus to tilt, and a subsequent shearing compression fracture of the medial malleolus. This type of MMF is characterized by relatively vertical fracture lines, and in some cases may present with a proximal medial cortical comminuted fracture (Figure 1A), a die-punch fragment (Figure 1B), compression and collapse of the medial part of DTAS (Figure 1C), and sometimes these characteristics may present simultaneously.
To our knowledge, no previous study has focused on the characteristics of vertical MMFs. The purpose of current study is to bring attention to the pathoanatomical characteristics and the different injury patterns associated with SAD type-II MMFs. The fractures associated with vertical MMFs are not so much simple. According to current results, the simple vertical MMF with one fracture line just accounted 39.6% of all fractures. Medial cortex comminuted fractures were much more common and accounted almost half of all this type MMFs. The TOA and LoR rate were not significantly increased in medial cortex comminuted MMFs while compared with others. However, the mean post-operative AOFAS score was significantly lower in these cases. That might because of the three failure cases were all characteristics with comminuted medial cortex. If the three failure cases were excluded, the mean AOFAS increased to 81.4±9.3 points, and no significant was reached any more (P=0.08). The die-punch fragment and medial articular surface compression were coexisted in most of these types’ cases (68%, Figure 4). McConnell and Tornetta (3) reported eight SAD type-II cases with marginal impaction of the medial tibial plafond, and emphasized that anatomic reduction was essential to the prevention of early arthrosis for this type of fractures. According to current results, vertical MMF with die-punch fragment was correlated with higher rate of LoR and lower AOFAS scores; and the joint compression was correlated with higher TOA and LoR rate, and with lower AOFAS scores. After the three failure cases were excluded, the mean AOFAS scores were still lower in the two groups (P<0.05).
Even though there have been many published reports of operative treatment of MMFs, very few comparative clinical studies have focused on comparison of internal fixation methods for the MMFs. Mohammed et al. (15) reported the only clinical comparative study focused on tension bands wiring and screw fixation; however, the participants were all Weber type B or C fractures. To the best of our knowledge, ours is the first clinical study focused on the functional outcomes and complications of two fixation methods for SAD type II MMFs.
Various fixation methods for MMFs have been reported in the literature. However, for SAD type II MMFs, the most commonly used fixation methods can be classified into two groups, lag screws fixation or buttress plate fixation (16,17). Because of the relatively vertical fracture line, tension band wiring fixation has rarely been applied in such cases. Some biomechanical studies have compared the two fixation methods for vertical MMFs (8,9,18). Toolan et al. (8) compared five fixation methods for vertical MMFs, and reported that the use of a buttress plate, with or without a distal lag screw, did not offer any advantage over lag screw fixation alone. However, other biomechanical studies have supported the use of a buttress plate for vertical shearing intraarticular fractures (9,18,19). Wegner et al. (9) reported that the buttress plate fixation of vertical medial malleolus fractures provides stiffer initial fixation than bicortical or unicortical screw fixation. Jones et al. (20) reported that the buttress plate (a 1/3 tubular plate was used) exhibited a stable, strong construct for fixation of vertical MMFs when compared with a hook plate. However, if a lag screw was combined with the buttress plate, the results were biomechanically superior to those of simple buttress plate fixation or hook plate fixation (20).
Nondisplaced medial malleolus fractures can usually be treated with cast immobilization; however, nondisplacement is rare in SAD type II injury because of the associated vertical violent force. Surgical reduction is necessary in this type of fracture because persistent displacement allows the talus to tilt into varus (21). Our mean 5 years follow up showed that ORIF of SAD type II MMF achieved good functional outcomes, and had a GTE of 81%. If the 3 cases of failure were excluded, the mean AOFAS score could reach a mean of 83.8 [63–97] points, with a GTE of 86%. Yu et al. (22) followed 23 SAD type II cases wherein 17 MMFs were fixed with buttress plate, and 6 with lag screws, and reported 1 instance of hardware loosening in the lag screws group. Ricci et al. (23) reported the loosening rate of lag screws fixation for MMF was as high as 13% (12/92), and was especially prevalent among those with partially threaded cancellous lag screws (24%). Ebraheim et al. (4) reported that among 111 MMFs, buttress plate fixations were used in 7 vertical fractures with no incidence of failure, and the mean AOFAS score was 84 points. The fracture mechanism and characteristics of SAD type II MMF are similar to those of posterior pilon fracture. Retrospective comparative studies have reported that buttress plate fixation for posterior pilon fractures showed better functional outcomes and less complications in comparison with lag screws fixation (18,24,25).
According to the current results, participants who underwent fixation of vertical MMFs with a buttress plate could commence FWB exercises earlier than those who received with lag screws fixation (P=0.04). Tan et al. (26) reported that no significant fracture displacement, hardware failure, or new fractures occurred in a cadaveric model of early weight-bearing on an unstable ankle fracture after ORIF. However, for ankle fractures caused by vertical violence, no matter medial or posterior malleolus, the injury mechanisms are more similar to pilon fractures, with a relative vertical fracture line and a small angle to the axis of tibia which cause a larger shear force between the fracture fragment and distal tibia. Many biomechanical studies have confirmed that buttress plate fixation for this type of intraarticular fracture achieves better stabilization than that of lag screws fixation (9,18-20). In our lag screw fixation group, 3 cases were diagnosed as failures and were further treated with revision surgeries. There was 1 case of fracture nonunion and fixation failure, and the other 2 cases were LoR with medial malleolus varus malunion. Although statistical analysis of failure rate detected no significant difference between groups, a failure rate as high as 13% was unacceptable, and such failure might bring disastrous ramifications to the patient. For intraarticular fractures, late TOA is unavoidable. Lübbeke et al. (27) reported that ankle fracture associated with medial malleolus has significantly large relative risks (RRs =2.5) and 95% confidence intervals (95% CIs: 1.5 to 4.4); thus, anatomical reduction and rigid fixation is of vital importance in the treatment of SAD type II MMF. Among our participants, TOA change radiographically detected in 7 cases; 4 of whom had no clinical symptoms, and the other 3 were treated conservatively.
The limitations of current study include the retrospective design, and the lack of random group allocation. We do agree that robust study design can yield a high level of evidence for treatment decision making; however, SAD type II injury is less common than other types of ankle fractures (2-4), and the baselines of the two groups were similar in our study. Our results confirmed the findings of previous biomechanical studies that buttress plate fixation of vertical MMF provides better mechanical support and stable fixation. The participants with buttress plate fixation could start FWB earlier, and had a lower rate of hardware failure. According to the current results, further well designed prospective comparative studies focused on the different fixation methods for vertical MMFs are still needed.
In conclusion, according to current study, more than 60% of vertical MMFs are with one or more characteristics of medial cortex comminuted fractures, or die-punch fragments, or medial joint compression. And patients with die-punch fragment, medial joint compression, LoR, large DTAS involvement and small FLA were positively correlated with the fair to poor clinical results. Lag screws and buttress plate fixation both can be used in this type MMFs, but the lag screw should be cautiously used in patients with comminuted medial cortex.
Acknowledgments
Funding: HZ, Key R & D plan of Shaanxi Province (No. 2021SF-025), Scientific research projects of Xi’an Health Commission (No. 2021ms07).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://dx.doi.org/10.21037/apm-21-1505
Data Sharing Statement: Available at https://dx.doi.org/10.21037/apm-21-1505
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/apm-21-1505). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of the Honghui Hospital Affiliated to Medical College of Xi’an Jiaotong University (No.: 20170003). Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Scott AM. Diagnosis and treatment of ankle fractures. Radiol Technol 2010;81:457-75. Erratum in: Radiol Technol 2011;83:56. [PubMed]
- Warner SJ, Garner MR, Hinds RM, et al. Correlation between the Lauge-Hansen classification and ligament injuries in ankle fractures. J Orthop Trauma 2015;29:574-8. [Crossref] [PubMed]
- McConnell T, Tornetta P 3rd. Marginal plafond impaction in association with supination-adduction ankle fractures: a report of eight cases. J Orthop Trauma 2001;15:447-9. [Crossref] [PubMed]
- Ebraheim NA, Ludwig T, Weston JT, et al. Comparison of surgical techniques of 111 medial malleolar fractures classified by fracture geometry. Foot Ankle Int 2014;35:471-7. [Crossref] [PubMed]
- Amorosa LF, Brown GD, Greisberg J. A surgical approach to posterior pilon fractures. J Orthop Trauma 2010;24:188-93. [Crossref] [PubMed]
- Wang L, Shi ZM, Zhang CQ, et al. Trimalleolar fracture with involvement of the entire posterior plafond. Foot Ankle Int 2011;32:774-81. [Crossref] [PubMed]
- Erdem MN, Erken HY, Burc H, et al. Comparison of lag screw versus buttress plate fixation of posterior malleolar fractures. Foot Ankle Int 2014;35:1022-30. [Crossref] [PubMed]
- Toolan BC, Koval KJ, Kummer FJ, et al. Vertical shear fractures of the medial malleolus: a biomechanical study of five internal fixation techniques. Foot Ankle Int 1994;15:483-9. [Crossref] [PubMed]
- Wegner AM, Wolinsky PR, Robbins MA, et al. Antiglide plating of vertical medial malleolus fractures provides stiffer initial fixation than bicortical or unicortical screw fixation. Clin Biomech (Bristol, Avon) 2016;31:29-32. [Crossref] [PubMed]
- Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma 1984;24:742-6. [Crossref] [PubMed]
- van Dijk CN, Verhagen RA, Tol JL. Arthroscopy for problems after ankle fracture. J Bone Joint Surg Br 1997;79:280-4. [Crossref] [PubMed]
- Kitaoka HB, Alexander IJ, Adelaar RS, et al. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 1994;15:349-53. [Crossref] [PubMed]
- Rodriguez EK, Kwon JY, Herder LM, et al. Correlation of AO and Lauge-Hansen classification systems for ankle fractures to the mechanism of injury. Foot Ankle Int 2013;34:1516-20. [Crossref] [PubMed]
- Kwon JY, Chacko AT, Kadzielski JJ, et al. A novel methodology for the study of injury mechanism: ankle fracture analysis using injury videos posted on YouTube.com. J Orthop Trauma 2010;24:477-82. [Crossref] [PubMed]
- Mohammed AA, Abbas KA, Mawlood AS. A comparative study in fixation methods of medial malleolus fractures between tension bands wiring and screw fixation. Springerplus 2016;5:530. [Crossref] [PubMed]
- Chen Y, Zhang H, Huang F, et al. Application of lateral malleolus hook-plate in treatment of stage II supination-adduction type medial malleolus fracture. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2014;28:1077-81. [PubMed]
- Blake S, Yakubek G, Shaer J. Use of a locked fibular plate for fixation of a vertical shear medial malleolus fracture: a case report. J Foot Ankle Surg 2015;54:1202-5. [Crossref] [PubMed]
- Zhao H, Liang X, Yu G, et al. Effectiveness and biomechanical analysis of three fixation methods in treatment of posterior Pilon fractures. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2013;27:1190-5. [PubMed]
- Bennett C, Behn A, Daoud A, et al. Buttress plating versus anterior-to-posterior lag screws for fixation of the posterior malleolus: a biomechanical study. J Orthop Trauma 2016;30:664-9. [Crossref] [PubMed]
- Jones DA, Cannada LK, Bledsoe JG. Are hook plates advantageous compared to antiglide plates for vertical shear malleolar fractures? Am J Orthop (Belle Mead NJ) 2016;45:E98-102. [PubMed]
- Michelson JD. Fractures about the ankle. J Bone Joint Surg Am 1995;77:142-52. [Crossref] [PubMed]
- Yu GR, Fan J, Zhou JQ, et al. Treatment strategies for grade II supination adduction ankle fractures. Chin J Trauma 2011;27:336-40.
- Ricci WM, Tornetta P, Borrelli J Jr. Lag screw fixation of medial malleolar fractures: a biomechanical, radiographic, and clinical comparison of unicortical partially threaded lag screws and bicortical fully threaded lag screws. J Orthop Trauma 2012;26:602-6. [Crossref] [PubMed]
- Huber M, Stutz P, Gerber C. Open reduction and internal fixation of the posterior malleolus with a posterior antiglide plate using a postero-lateral approach: a preliminary report. J Foot Ankle Surg 1996;2:95-103. [Crossref]
- De Vries JS, Wijgman AJ, Sierevelt IN, et al. Long-term results of ankle fractures with a posterior malleolar fragment. J Foot Ankle Surg 2005;44:211-7. [Crossref] [PubMed]
- Tan EW, Sirisreetreerux N, Paez AG, et al. Early weightbearing after operatively treated ankle fractures: a biomechanical analysis. Foot Ankle Int 2016;37:652-8. [Crossref] [PubMed]
- Lübbeke A, Salvo D, Stern R, et al. Risk factors for post-traumatic osteoarthritis of the ankle: an eighteen year follow-up study. Int Orthop 2012;36:1403-10. [Crossref] [PubMed]
(English Language Editor: J. Jones)


