
The impact of transthoracic echocardiography on the short-term prognosis of elderly patients in the intensive care unit: a retrospective analysis based on the MIMIC-III database
Introduction
Elderly patients often present to the intensive care unit (ICU) with serious and complicated conditions, and the prognosis is often poor. In fact, there is a certain controversy about the admission of elderly patients to the ICU, because studies have shown that more than half of the elderly patients admitted to the ICU are at the end of life (1). One study found that compared with staying in a standard ward, staying in an ICU did not improve the 6-month survival rate of elderly patients over 80 years old (2). Later, Guidet et al. found in a randomized controlled study that compared with standard treatment, admission to the ICU for elderly patients over the age of 75 did not reduce the 6-month mortality rate (3). In another study of health economics, the hospital mortality of non-elderly (18–65 years old) patients, elderly (65–80 years old) patients, and advanced age (>85 years old) patients increased sequentially, and the total medical expenses and daily average increased in turn (4). In addition to the economic costs and the lack of impact on the prognosis, many meaningless ICU treatments may cause a scarcity of medical resources, and other patients who need to be admitted to the ICU are delayed (5). Elderly patients admitted to the ICU often have heart disease or other heart-related problems, leading to frequent decline or deterioration of heart function in elderly patients, which increases hospital mortality and is not conducive to long-term prognosis (6). In clinical practice, doctors often perform transthoracic ultrasound examinations on these patients, as often as once a day to monitor changes in their condition. Transthoracic echocardiography (TTE) is a simple, non-invasive test that can determine whether there are abnormalities in the structure and function of the heart in elderly patients (7). Using TTE, the doctor can judge the severity of the patient’s condition and adjust the treatment plan in time. However, there is no relevant research to evaluate the rationality of TTE for middle-aged and elderly patients in ICU, and some doctors have not actively adjusted the treatment plan based on the results of ultrasound examination (8). In fact, many ICU doctors are not very familiar with the relevant guidelines, even if the guidelines may not clearly stipulate this issue (9,10). For patients who are not selected for non-cardiac surgery, studies have found that preoperative echocardiography cannot reduce mortality and reduce hospital stay (11). There are also research results that show that TTE parameters cannot improve the APACHE II score for predicting the risk of death in critically ill patients (12). The purpose of this study is to observe whether the TTE examination has an impact on the short-term prognosis and related indicators of elderly patients admitted to the ICU through retrospective analysis, so as to provide certainty for the rational application of TTE in clinical practice, reducing the excessive use of TTE, and optimizing the allocation of medical resources.
We present the following article in accordance with the STROBE reporting checklist (available at https://dx.doi.org/10.21037/apm-21-1713).
Methods
Study population
The subjects of this study are elderly patients admitted to the ICU. Inclusion criteria: (I) age ≥65 years; (II) first admission to ICU (for elderly patients who have been admitted to ICU multiple times, only the first admission data is collected); (III) stay time in ICU ≥24 h. Exclusion criteria: (I) loss of key data, such as the first sequential organ failure score (SOFA), the first simplified acute physiology score I (SAPS I), etc.; (II) lost to follow-up. All patients’ information in the MIMIC-III database is anonymous, and informed consent is not required; this study is eligible for exemption after being reviewed by the Ethics Committee of Shanxi Provincial People’s Hospital. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Data source
The data for this study was obtained from the MIMIC-III database. The MIMIC-III database is an open critical medicine database jointly released by the Massachusetts Institute of Technology Computational Physiology Laboratory, Beth Israel Dikon Medical Center and Philips Medical under the funding of the National Institutes of Health. The latest version is MIMIC-III v1.4 (13). The database collected hospitalization information of more than 50,000 patients admitted to the ICU of Beth Israel Dikang Medical Center from June 2001 to October 2012. The data includes vital signs, medications, laboratory tests results, clinical observation results, records drawn by nursing staff, fluid balance, program codes, diagnostic codes, imaging reports, hospital stay and survival data, etc. Data acquisition process and permission: The data extraction and analysis work in this study was completed by Dr. Wang. After completing the Cooperative Organization Training Initiative (CTCI) course, the access to the database was approved by the review committee of Beth Israel Dikang Medical Center and Massachusetts Institute of Technology. At the same time, Dr. Chen passed the test to protect human research participants and obtained the right to download and use the database.
Data extraction
SQL language was used to extract the following data from MIMIC-III database: age, gender, weight, white blood cell count (WBC), hemoglobin (Hb), platelet count (PLT), blood urea nitrogen (BUN), blood creatinine (SCr), blood glucose (Glu), blood electrolytes (K+, Na+, Ca2+), blood HCO3-, sequential organ failure score (SOFA), ICU hospital stay, ICU deaths, other ICU data, comorbidities [hypertension, coronary heart disease, chronic obstruction pulmonary disease (COPD), and chronic kidney disease (CKD)], whether mechanical ventilation, vasoactive drugs and renal replacement therapy (RRT) were used during ICU hospitalization, and whether they were complicated by ventilator-associated pneumonia (VAP), urinary tract infection (UTI), diabetic ketoacidosis (DKA), acute myocardial infarction (AMI), etc. All laboratory test parameters are extracted from the data generated within the first 24 hours after the patient enters the ICU (i.e., the baseline value) and the extreme values during the ICU hospitalization period [i.e., the maximum value (max) and minimum value (min)].
Outcome
The primary endpoint observed in this study is the mortality rate within 28 days after the patient was admitted to the ICU. Secondary endpoints include the number of days of non-mechanical ventilation within 28 days after the patient was admitted to the ICU, the number of days without vasoactive drugs, the maximum dose of norepinephrine, the fluid input volume in the first three days after the patient was admitted to the ICU, and the decrease of serum lactic and creatinine. Calculation of the decrease in lactate and creatinine: For patients undergoing TTE examination, we used the latest test result before TTE examination minus the first test result 48 hours after TTE examination; for patients who did not undergo TTE examination, the first test after admission to the ICU minus the result of the first test results 48 h after this test.
Statistical analysis
SPSS software (version 23.0, IBM, Chicago, USA) was used to perform statistical analysis on all research data. Continuous variables are tested for normality first. If they are normally distributed, they are expressed as the mean ± standard deviation (x ± SD). The comparison between the two groups uses independent student t-test; if they are non-normally distributed, then expressed as median (quartile) [M(QL, QU)] and the Wilcoxon ran sum test was used for comparison between the two groups. Categorical variables are expressed as percentages (%), and the χ2 test is used for comparison between the two groups. Multivariate logistic regression analysis was used to analyze the risk factors related to death of elderly patients within 28 days of admission to the ICU. Doubly robust estimation was used to infer the relationship between the use of TTE and patient endpoint events (14). The gradient boosted model (GBM) was used to estimate the propensity score (PS) of patients undergoing TTE examination, so as to minimize the imbalance of variables between the TTE group and the non-TTE group. Using PS as the weight, the inverse probabilities weighting (IPW) model was used to generate a weighted cohort (15). P<0.05 indicates that the difference is statistically significant.
Results
General information
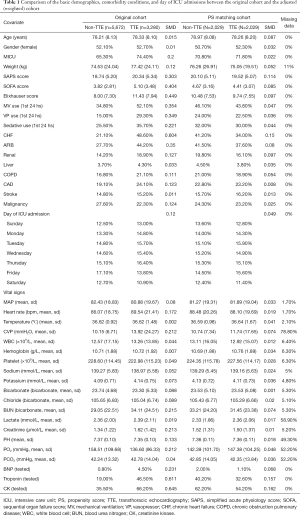
According to the inclusion and exclusion criteria, we extracted 8,952 elderly cases from the MIMIC-III database (Figure 1), and divided them into TTE and non-TTE groups. There were 3,280 cases (36.6%) in the TTE group, of which 1,729 were women (52.71%); there were 5,672 cases (63.4%) in the non-TTE group, of which 2,955 cases (52.1%) were women. The SAPS score (20.34±5.34 vs. 18.74±5.2, t=13.889, P<0.001) and SOFA score (5.10±3.38 vs. 3.82±2.81, t=19.250, P<0.001) of patients in the TTE group were higher than those of non-TTE group. The percentage of patients in the TTE group receiving mechanical ventilation (52.10% vs. 34.80%) and vasoactive drugs (29.30% vs. 15.00%) was significantly higher than that in the non-TTE group. These results suggest that patients undergoing TTE examination are more severely ill than those who are not undergoing TTE examination (For detailed information, see Table 1).
Full table
Double robust analysis
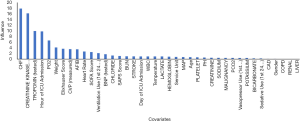
The results of PS analysis using GBM based on covariates are shown in Figure 2. The contribution of different covariates to the PS score can be observed in Figure 2. In this study, the covariates that have a greater contribution to PS include chronic heart failure (CHF), creatine kinase (CK), troponin, occupancy ICU hours, PO2, etc. In clinical practice, these indicators often prompt doctors to perform TTE examinations on patients. Based on this result, IPW was used to standardize the difference between the TTE group and the non-TTE group (15). The results are shown in Table 1. By comparing the patient cohorts derived from PS score compatibility, it was found that there are still differences in many indicators between the two groups of patients, but the results have been reversed. For example, in the original cohort, the ratio of CHF patients in the TTE group was higher than in the non-TTE group. However, in the new cohort, the rate of CHF patients in the non-TTE group was higher than in the TTE group. Similar variables include creatine kinase (CK), and troponin. Further regression analysis adjusted these variables with differences between groups.
Endpoint analysis
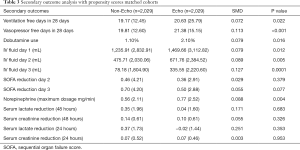
The doubly robustness estimation showed that patients in the TTE examination group had a lower risk of death within 28 after admission to the ICU than in the non-TTE group. In the PS score compatibility cohort, the 28-day mortality rate of patients in the TTE group was 23.4%, and the 28-day mortality rate of patients in the non-TTE group was 28.7%. The adjusted OR value was 0.76 (95% CI: 0.65–0.87, P<0.001). Similarly, the analysis results of the other three models are consistent with this, suggesting that TTE examination is beneficial to reduce the risk of death at 28 days (Table 2). Analysis of secondary endpoints showed that patients in the TTE group did not use mechanical ventilation and vasoactive drugs for a longer period of time than those in the non-TTE group, and the patients in the TTE group had significantly more fluid input in the first three days after admission to the ICU than patients in non-TTE group, but the former dopamine use rate and the former norepinephrine maximum use speed were higher in the TTE group. Other secondary endpoints were not statistically different between the two groups (Table 3).

Full table
Full table
Discussion
Due to advances in science and technology, increasingly precise, minimally invasive and even non-invasive examination methods are used in clinical practice. However, what follows is overuse of certain examinations and treatments, which on the one hand causes a significant increase in economic costs, and on the other hand wastes time costs (16-18). In most countries in the world, medical resources are still scarce resources, and medical costs remain a heavy burden (19-21). It is important to clarify the practical application value of auxiliary examinations for patients. First, patients who should be examined have sufficient reason to get timely examinations. Second, unnecessary examinations and occupying medical resources should be avoided, which can also reduce the economic burden of the country, society and individuals. In a multi-institution (three tertiary, four community) study, Sinvani et al. found that elderly patients undergoing cardiac ultrasonography before surgery led to prolonged preoperative waiting time, but did not reduce mortality (18). While coronary angiography in patients with stable angina pectoris cannot improve mortality, the use of intravascular ultrasound to guide drug-eluting stent implantation can further reduce patient mortality (22). Therefore, any new technology must be continuously tested in clinical practice to determine the application value of the technology in clinical practice, especially for different patients. It cannot be taken for granted that the examination must be beneficial to the diagnosis and treatment of patients.
The MIMIC-III database was established by MIT and other units based on the electronic medical record system. It is a continuously supplemented dynamic data system that reflects the diagnosis and treatment process of critically ill patients in the real world. It has become a resource that researchers in critical care medicine often utilize (23), and many important discoveries have been made and analyses have been conducted using this database (24-27). Based on the latest version of the database, we retrospectively analyzed the impact of TTE on the short-term prognosis of elderly patients admitted to the ICU. The results suggest that timely TTE examination can reduce the 28-day mortality risk of elderly critically ill patients. According to the analysis results of the PS compatibility cohort, this benefit may be related to several factors. First, in the compatibility cohort, the SAPS and SOFA scores of patients in the non-TTE group were higher than those in the TTE group, suggesting that the former is more ill than the latter, but the difference was adjusted in regression analysis; secondly, it may be due to the fact that doctors gave more fluid input and used more vasoactive drugs to patients in the TTE group based on the results of the TTE examination. Of course, further research is warranted to confirm whether these measures contributed to the decreased mortality rate of patients in the TTE group compared to that in the non-TTE group. Fluid therapy for critically ill patients has always been the focus of critical care medicine. Excessive fluid load, sodium load, and chlorine load increase the risk of death (28,29). However, in clinical practice, doctors’ concern about excess fluid may lead to insufficient fluid infusion in some critically ill patients. A study by Marik et al. found that for patients with severe sepsis and septic shock, the actual volume of fluid input was significantly lower than the volume recommended by the guidelines; on the other hand, the input of more than 5,000 mL of fluid on the first day of admission to the ICU significantly increase the risk of death and cost of hospitalization (30).
According to our results, we believe that when elderly patients are admitted to the ICU, TTE examinations should be performed in a timely manner according to the patient’s specific condition, especially when the effective circulating blood volume of the patient is insufficient. Depending on the examination results and the specific condition of the patient, appropriate vasoactive drugs and fluid treatments should be given in time. Clinicians should not worry too much about the patient’s cardiopulmonary function, leading to insufficient fluid administration. This situation requires special attention in elderly patients with cardiopulmonary diseases.
This study has some limitations: First, although this study is based on real-world data with a large sample size, the data comes from a single medical center, which may have various biases such as medical level, habits, and population; secondly, this study is a retrospective analysis, and due to the lack of key information and other reasons in the data extraction process, a large number of patient data may be excluded, and there may be selection bias; in addition, although TTE is non-invasive and convenient, its reproducibility is relatively poor. The consistency of TTE examination in this study cannot be evaluated, and there may be measurement bias. Therefore, we suggest designing a prospective, multi-center study based on similar studies to further observe the impact of TTE on elderly patients with severe illness.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://dx.doi.org/10.21037/apm-21-1713
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/apm-21-1713). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All patients’ information in the MIMIC-III database is anonymous, and informed consent is not required; this study is eligible for exemption after being reviewed by the Ethics Committee of Shanxi Provincial People’s Hospital. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ritzema J, Young P. Admitting elderly patients to ICU: is it just about survival? N Z Med J 2017;130:8-10. [PubMed]
- Boumendil A, Latouche A, Guidet B, et al. On the benefit of intensive care for very old patients. Arch Intern Med 2011;171:1116-7. [Crossref] [PubMed]
- Guidet B, Leblanc G, Simon T, et al. Effect of Systematic Intensive Care Unit Triage on Long-term Mortality Among Critically Ill Elderly Patients in France: A Randomized Clinical Trial. JAMA 2017;318:1450-9. [Crossref] [PubMed]
- Haas LEM, van Beusekom I, van Dijk D, et al. Healthcare-related costs in very elderly intensive care patients. Intensive Care Med 2018;44:1896-903. [Crossref] [PubMed]
- Zivot JB. Elderly Patients in the ICU: Worth It or Not? Crit Care Med 2016;44:842-3. [Crossref] [PubMed]
- Gayat E, Cariou A, Deye N, et al. Determinants of long-term outcome in ICU survivors: results from the FROG-ICU study. Crit Care 2018;22:8. [Crossref] [PubMed]
- Si X, Ma J, Cao DY, et al. Transesophageal echocardiography instead or in addition to transthoracic echocardiography in evaluating haemodynamic problems in intubated critically ill patients. Ann Transl Med 2020;8:785. [Crossref] [PubMed]
- Matulevicius SA, Rohatgi A, Das SR, et al. Appropriate use and clinical impact of transthoracic echocardiography. JAMA Intern Med 2013;173:1600-7. [Crossref] [PubMed]
- Frankel HL, Kirkpatrick AW, Elbarbary M, et al. Guidelines for the Appropriate Use of Bedside General and Cardiac Ultrasonography in the Evaluation of Critically Ill Patients-Part I: General Ultrasonography. Crit Care Med 2015;43:2479-502. [Crossref] [PubMed]
- Levitov A, Frankel HL, Blaivas M, et al. Guidelines for the Appropriate Use of Bedside General and Cardiac Ultrasonography in the Evaluation of Critically Ill Patients-Part II: Cardiac Ultrasonography. Crit Care Med 2016;44:1206-27. [Crossref] [PubMed]
- Wijeysundera DN, Beattie WS, Karkouti K, et al. Association of echocardiography before major elective non-cardiac surgery with postoperative survival and length of hospital stay: population based cohort study. BMJ 2011;342:d3695. [Crossref] [PubMed]
- Sawchuk CW, Wong DT, Kavanagh BP, et al. Transthoracic echocardiography does not improve prediction of outcome over APACHE II in medical-surgical intensive care. Can J Anaesth 2003;50:305-10. [Crossref] [PubMed]
- Johnson AE, Pollard TJ, Shen L, et al. MIMIC-III, a freely accessible critical care database. Sci Data 2016;3:160035 [Crossref] [PubMed]
- Dukes O, Martinussen T, Tchetgen Tchetgen EJ, et al. On doubly robust estimation of the hazard difference. Biometrics 2019;75:100-9. [Crossref] [PubMed]
- Matsouaka RA, Atem FD. Regression with a right-censored predictor using inverse probability weighting methods. Stat Med 2020;39:4001-15. [Crossref] [PubMed]
- Schmidt T, Maag R, Foy AJ. Overdiagnosis of Coronary Artery Disease Detected by Coronary Computed Tomography Angiography: A Teachable Moment. JAMA Intern Med 2016;176:1747-8. [Crossref] [PubMed]
- Herwig A, Dehnen D, Weltermann B. Patient factors driving overuse of cardiac catheterisation: a qualitative study with 25 participants from two German teaching practices. BMJ Open 2019;9:e024600 [Crossref] [PubMed]
- Sinvani L, Mendelson DA, Sharma A, et al. Preoperative Noninvasive Cardiac Testing in Older Adults with Hip Fracture: A Multi-Site Study. J Am Geriatr Soc 2020;68:1690-7. [Crossref] [PubMed]
- Morgan DJ, Dhruva SS, Coon ER, et al. 2019 Update on Medical Overuse: A Review. JAMA Intern Med 2019;179:1568-74. [Crossref] [PubMed]
- Hall SF, Griffiths R. Use and overuse of diagnostic neck ultrasound in Ontario: Retrospective population-based cohort study. Can Fam Physician 2020;66:e62-8. [PubMed]
- Mendelson RM. Diagnostic imaging: Doing the right thing. J Med Imaging Radiat Oncol 2020;64:353-60. [Crossref] [PubMed]
- Mintz GS. Intravascular ultrasound guidance improves patient survival (mortality) after drug-eluting stent implantation: review and updated bibliography. Cardiovasc Interv Ther 2020;35:37-43. [Crossref] [PubMed]
- Weeks HL, Beck C, McNeer E, et al. medExtractR: A targeted, customizable approach to medication extraction from electronic health records. J Am Med Inform Assoc 2020;27:407-18. [Crossref] [PubMed]
- Feng M, McSparron JI, Kien DT, et al. Transthoracic echocardiography and mortality in sepsis: analysis of the MIMIC-III database. Intensive Care Med 2018;44:884-92. [Crossref] [PubMed]
- Meyer A, Zverinski D, Pfahringer B, et al. Machine learning for real-time prediction of complications in critical care: a retrospective study. Lancet Respir Med 2018;6:905-14. [Crossref] [PubMed]
- Gordon DD, Patel I, Pellegrini AM, et al. Prevalence and Nature of Financial Considerations Documented in Narrative Clinical Records in Intensive Care Units. JAMA Netw Open 2018;1:e184178 [Crossref] [PubMed]
- Gao S, Wang Y, Yang L, et al. Characteristics and clinical subtypes of cancer patients in the intensive care unit: a retrospective observational study for two large databases. Ann Transl Med 2021;9:13. [Crossref] [PubMed]
- Van Regenmortel N, Verbrugghe W, Roelant E, et al. Maintenance fluid therapy and fluid creep impose more significant fluid, sodium, and chloride burdens than resuscitation fluids in critically ill patients: a retrospective study in a tertiary mixed ICU population. Intensive Care Med 2018;44:409-17. [Crossref] [PubMed]
- Hernández G, Ospina-Tascón GA, Damiani LP, et al. Effect of a Resuscitation Strategy Targeting Peripheral Perfusion Status vs Serum Lactate Levels on 28-Day Mortality Among Patients With Septic Shock: The ANDROMEDA-SHOCK Randomized Clinical Trial. JAMA 2019;321:654-64. [Crossref] [PubMed]
- Marik PE, Linde-Zwirble WT, Bittner EA, et al. Fluid administration in severe sepsis and septic shock, patterns and outcomes: an analysis of a large national database. Intensive Care Med 2017;43:625-32. [Crossref] [PubMed]
(English Language Editor: G. Stone)



