The application effects of personalized nursing on the perioperative period of hepatobiliary surgery: a systematic review and meta-analysis
Introduction
Hepatobiliary disease, including viral hepatitis, fatty liver, cholecystitis, and cholelithiasis, is characterized by a rapid onset and development with a critical condition, and is a common chronic disease in clinical surgery (1). The clinical efficacy of hepatobiliary surgery has been greatly improved in the past 10 years, which has an incidence rate of 14.5% now (2). Additionally, due to more advanced preoperative imaging, improved extra-operative care, progressive surgical techniques, a better understanding of anatomy, technological advancements in intraoperative instruments, the early identification of disease and complication management, the postoperative mortality of hepatobiliary surgery has reduced from 20% to 3% (3). However, hepatobiliary surgery is a complex operation and has a high postoperative morbidity.
Infectious complications are one of the main causes of death. According to statistics from large studies and national databases, the incidence of concurrent surgical infections is 9.9–23% (4-6). A research (7) showed that the worsening of an infection at a surgical site can extend the hospitalization tine to 10.6 days and cost an additional US$20,842, suggesting postoperative infections increased hospitalization time, resource utilization, and readmission rates, and placed considerable economic burdens on hospitals and patients. Reasonable rehabilitation nursing plays an important role in accelerating the prognosis of patients.
Personalized nursing is a new model of nursing. In terms of nursing care, it emphasizes patient-centered services to reduce or block patients’ physiological stress responses during the operation via multidisciplinary cooperation in nursing, anesthesia, and nutrition, and ultimately promotes postoperative recovery (8). Unlike traditional disease-centered nursing, personalized nursing comprehensively considers all aspects of nursing, including patients’ personal needs, values, and preferences, and encourages patients to actively participate in making decisions to achieve goals (9). Previous studies have shown that there is a positive correlation between the application of personalized nursing and better nursing quality and recovery, and that personalized nursing increases patients’ levels of satisfaction with nursing, and their initiative and life quality (10). In addition, related studies have shown that personalized nursing can shorten hospitalization time without increasing medical expenditure (11). The benefits of personalized nursing for professionals include improved motivation and job satisfaction (12). However, no consensus on the effectiveness of personalized nursing in clinical settings has yet been reached. This meta-analysis sought to collect the current evidence on the application effects of personalized nursing on hepatobiliary surgery, and evaluate the effectiveness of personalized nursing during the perioperative period in hepatobiliary surgery.
We present the following article in accordance with the PRISMA reporting checklist (available at https://dx.doi.org/10.21037/apm-21-1923).
Methods
This study conducted a systematic review and meta-analysis of randomized controlled trials (RCTs). As this study was a literature study, patient consent and approval from an ethics committee were not required.
Literature search
The publication period was set from 2010 to 2021. Electronic databases, including the PubMed, Web of Science, Embase, CNKI, and Wanfang databases, were searched. We also reviewed the references of articles and previously related systematic reviews to find other studies. For each database, the search criteria were customized. The keywords for the searches were a combination of Medical Subject Headings (MESH) and the following entry terms: “Personalized nursing”, “Hepatobiliary surgery”, and “Perioperative period”.
Inclusion criteria
Articles were included in the meta-analysis if they met the following inclusion criteria: (I) the study examined hepatobiliary surgery nursing during the perioperative period; (II) the participants were in the perioperative period of hepatobiliary surgery; (III) different interventions were used to nurse the patients (i.e., traditional nursing and personalized nursing); (IV) the main results included any one of the following items: patients’ level of satisfaction after nursing, the incidence of adverse reactions (infection, thrombosis, bleeding, dizziness, and vomiting), postoperative recovery indicators (average hospitalization time, the time it took to get out of bed for the first time after surgery, the time it took to first eat after surgery, and the time it took to first exhaust after surgery), and patients’ level of anxiety and depression [Self-rating Anxiety Scale (SAS) and Self-rating Depression Scale (SDS) scores after nursing]; and (V) to ensure the evidence was of a high level, the study had to be a RCT or a selected article in the same disease field that had recently been published in an authoritative journal.
Exclusion criteria
Articles were excluded from the meta-analysis if: (I) the article failed to meet the inclusion criteria; (II) the article was obsolete; and/or (III) the research findings detailed in the article had been published previously.
Research selection and data extraction
The articles were screened and selected by 2 team members independently. All search records were imported into EndNote X9 to avoid to duplication. To further evaluate the eligibility of some studies, the full texts were obtained and disagreements were discussed with a 3rd member. Information about the author, publication year, trial time, sample size, age, and gender of the participants, study type, and outcome indicators were extracted from the included articles.
Data analysis
Stata 16.0 (meta package) was used for the meta-analysis. When studying the clinical effects of different types of nursing, the standardized mean difference (SMD) or odds ratio (OR) with a 95% confidence interval (CI) was used to present the data. I2 and Q tests were used to detect the level of heterogeneity. An I2>50% or a P<0.05 was considered to indicate significant heterogeneity. If there was significant heterogeneity, a fixed-effects model was applied to calculate the pooled effect size; otherwise, a random-effects model was used. A P value <0.05 was considered statistically significant.
Sensitivity analysis
To perform the sensitivity analysis, all the studies included were deleted 1 by 1 in this meta-analysis to confirm whether these studies were significantly affected by any individual study.
Results
Literature screening
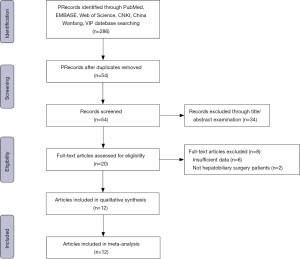
In the final screening, a total of 286 records were identified from the electronic database. After deleting duplicate and obviously irrelevant studies, and excluding 34 studies by reading titles and abstracts, the full text of 20 articles were read to further evaluate the articles (see Figure 1). In the end, a total of 12 studies (13-24), comprising 1,039 hepatobiliary patients in the perioperative, period, were included in this systematic review. There were 520 patients in the treatment group and 519 patients in the control group.
Research characteristics
The number of participants in each study ranged from 70 to 115. The duration of the interventions ranged from 1 to 2 years and 10 months. There was no significant difference in the baseline data of the patients in terms of age and gender between the treatment group and the control group. This study only included RCTs. The main characteristics of the included studies are set out in Table 1.
Table 1
| Study | Year | Sample time | Cases treat/con | Age (years) | Sex ratio (M/F) | Study design | Outcome measures | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Treat | Con | Treat | Con | |||||||
| Ge Lulu | 2016 | Jan 2013 to Apr 2015 | 43/43 | 48.3±8.9 | 47.8±9.2 | 30/13 | 31/12 | RCT | ①②③④⑤⑥⑦⑧ | |
| Zhang Chunyuan | 2016 | May 2013 to Apr 2015 | 43/43 | 48.3±8.9 | 47.8±9.2 | 33/10 | 29/14 | RCT | ①③④⑤⑥⑦⑧ | |
| Huo Xiaoyan | 2017 | Jul 2015 to Aug 2016 | 54/54 | 50.8±7.5 | 50.3±7.6 | 35/19 | 32/22 | RCT | ②③④⑤⑥⑦⑧ | |
| Shan Haixia | 2017 | Mar 2014 to Mar 2016 | 37/38 | 46.1±8.5 | 45.1±7.5 | 20/17 | 21/17 | RCT | ①②③④⑤⑥⑦⑧ | |
| Zheng Jiaxin | 2019 | Apr 2017 to Jul 2018 | 58/57 | 44.9±3.4 | 44.9±3.4 | 32/26 | 33/24 | RCT | ①②③④⑤⑥⑦⑧ | |
| Li Teng | 2016 | Jul 2011 to Jul 2012 | 48/48 | 25–57 | 25–58 | NP | NP | RCT | ②③④⑤⑥⑦⑧ | |
| Liao Chunmei | 2014 | Jun 2011 to Apr 2013 | 40/40 | 47.2±3.5 | 48.0±2.6 | 27/13 | 29/11 | RCT | ①②⑦⑧ | |
| Liu Hui | 2015 | Oct 2013 to Dec 2014 | 38/37 | 43.1±11.5 | 43.1±11.5 | 21/17 | 20/17 | RCT | ①②⑦⑧ | |
| Zhang Limin | 2017 | May 2013 to Mar 2016 | 38/38 | 48.5±8.6 | 48.6±8.2 | 28/10 | 26/12 | RCT | ②③④⑤⑥⑦⑧ | |
| Chen Yanjie | 2019 | Jan 2018 to Dec 2018 | 43/43 | 53.7±9.5 | 55.9±9.6 | 22/21 | 24/16 | RCT | ②③④⑤⑥⑦⑧ | |
| Zhou Chunmei | 2020 | May 2018 to Sep 2019 | 43/43 | 54.8±6.3 | 54.8±6.3 | 28/15 | 27/16 | RCT | ①②③④⑦⑧ | |
| Shen Yanlibg | 2020 | Feb 2018 to Jan 2019 | 35/35 | 43.7±7.0 | 45.6±7.9 | 21/14 | 20/15 | RCT | ②③④⑤⑥⑦⑧ | |
①: post-nursing level of satisfaction; ②: incidence of adverse reactions; ③: hospitalization time; ④: the time it took to get out of bed for the first time after surgery; ⑤: the time it took to first eat after surgery; ⑥: the time it took to first exhaust after surgery; ⑦: SAS score after nursing; ⑧: SDS score after nursing. Treat, Treatment group; Con, Control group; M, male; FM, female; NP, not reported; RCT, randomized controlled trial.
Data analysis
Eight indicators that frequently appeared in the literature were selected for the meta-analysis. Patients’ level of satisfaction post-nursing and the incidence of adverse reactions were the main clinical indicators. The secondary outcome indicators were the postoperative recovery indicators (i.e., average hospitalization time, the time it took to get out of bed for the first time after surgery, the time it took to first eat after surgery, and the time it took to first exhaust after surgery), and patients’ levels of anxiety and depression (i.e., SAS and SDS scores after nursing).
Indicators of application effect
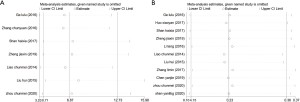
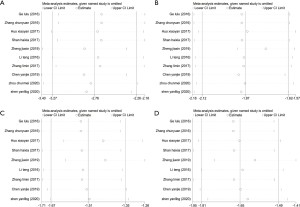
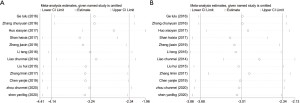
Seven studies reported on patients’ level of post-nursing satisfaction for the treatment group and the control group. Ten studies reported on the incidence of adverse reactions. The results of the meta-analysis of patients’ level of post-nursing satisfaction and the incidence of adverse reactions are shown in Figure 2A,2B. A heterogeneity analysis was performed, and it was reported that neither the heterogeneity of patients’ level of satisfaction with nursing (I2=0.0%; P=0.811, fixed-effects model) nor the heterogeneity of the incidence of adverse reactions (I2=0.0%; P=0.999; fixed-effects model) were significantly different. Compared to traditional nursing, patients who received personalized nursing had significantly higher levels of satisfaction (OR =6.871; 95% CI: 3.708–12.734), and the incidence of adverse reactions was distinctly lower (OR =0.234; 95% CI: 0.153–0.357). To further confirm the stability of the results of the 2 indicators, a sensitivity analysis was performed. After deleting the included articles 1 by 1, the confidence intervals of the effect values of patients’ post-nursing levels of satisfaction (see Figure 3A) and the incidence of adverse reactions (see Figure 3B) fluctuated in a small arrangement around the pooled effect size, indicating that the results were stable.

Postoperative recovery indicators
Postoperative recovery comprised the following 4 aspects: (I) average hospitalization time; (II) the time it took to get out of bed for the first time after surgery; (III) the time it took to first eat after surgery; and (IV) the time it took to first exhaust after surgery. 10 studies reported data on the average hospitalization time and the time it took to get out of bed for the first time after surgery. The heterogeneity analysis indicated that the heterogeneity of the average hospitalization time (I2=86.7%; P<0.001, random-effects model) was significantly distinct from the time it took to get out of bed for the first time after surgery (I2=59.6%; P=0.008; random-effects model). After personalized nursing, the average hospitalization time and the time it took to get out of bed for the first time after surgery were significantly reduced. Specifically, the average hospitalization time was shortened by 2.763 days (SMD =−2.763; 95% CI: −3.269–2.257; see Figure 4A), and the time it took to get out of bed for the first time after surgery was shortened by 1.868 days (SMD =−1.868; 95% CI: −2.120–−1.617; see Figure 4B).
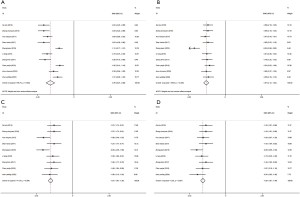
9 studies reported data on the time it took to first eat after surgery and the time it took to first exhaust after surgery. The heterogeneity analysis showed that the heterogeneity of the time it took to first eat after surgery (I2=41.0%; P=0.094, fixed-effects model) and time it took to first exhaust after surgery (I2=6.2%; P=0.384, fixed-effects model) had no significant difference. The results in relation to the time it took to first eat after surgery and the time it took to first exhaust after surgery for patients who received personalized nursing were better than those for patients who received traditional nursing. Specifically, the time it took to first eat after surgery was shortened by 1.507 days (SMD =−1.507; 95% CI: −1.665–−1.349; see Figure 4C), and the time it took to first exhaust after surgery was shortened by 1.648 days (SMD =−1.648; 95% CI: −1.810–−1.487; see Figure 4D). The results of the sensitivity analysis showed that after excluding the included articles 1 by 1, the pooled effect size and CI of the average hospitalization time (see Figure 5A), the time it took to get out of bed for the first time after surgery (see Figure 5B), the time it took to first eat after surgery (see Figure 5C), and the time it took to first exhaust after surgery (see Figure 5D) did not change significantly, suggesting that the meta-analysis was stable.
Anxiety and depression indicators of patients
The 12 included articles used post-nursing SAS and SDS scores to assess patients’ anxiety and depression levels. The results of the heterogeneity analysis showed that the heterogeneity of the SAS score (I2=96.2%; P<0.001, random-effects model) based on these 12 studies was not significant, while the heterogeneity of SDS score (I2=93.2%; P<0.001; random-effects model) was significant. The results of the meta-analysis showed that compared to patients who received traditional nursing, the SAS and SDS scores of patients who received personalized nursing were reduced. Specifically, patients’ SAS score after personalized nursing was reduced by 3.241 points (SMD =−3.241; 95% CI: −4.141–−2.341; Figure 6A), and their SAS score was decreased by 3.007 points (SMD =−3.007; 95% CI: −3.677–−2.338; Figure 6B). The sensitivity analysis showed that the pooled effect size and CI of patients’ SAS score (see Figure 7A) and SDS score (see Figure 7B) after personalized nursing did not fluctuate significantly, suggesting that the meta-analysis was stable.

Discussion
Our systematic review included 12 related articles on the effects of personalized nursing during the perioperative period of hepatobiliary surgery. Unlike previous reviews in this field, this review not only explored the clinical efficacy of personalized nursing in the perioperative period and the postoperative recovery of patients, but also examined patients’ psychological status.
According to the results of this meta-analysis, personalized nursing improved patients’ level of satisfaction. The level of nursing satisfaction of the treatment group was between 92.11–97.67%, while that of the control group was between 74.42–78.38%. An analysis of the factors affecting patients’ levels satisfaction also showed that personalized nursing strengthened the communication between nurses and patients and provided patients with required decision-making information (25). Additionally, hospitalization time had a significant effect on patients’ levels of satisfaction with nursing. The longer patients stayed in hospital, the more satisfied they were with the nursing (26). Continuous personalized nursing made patients believe that their individuality was truly recognized and considered.
Personalized nursing also reduced the incidence of adverse reactions. The incidence of adverse reactions in the treatment group was 4.64–8.57%, while the incidence in the control group was 23.25–28.57%. Patients’ postoperative recovery improved significantly. Clinical curative and prognostic indicators, including the average hospitalization time, the time it took to get out of bed for the first time after surgery, the time it took to first eat after surgery, and time it took to first exhaust after surgery were all notably shortened. As part of the process of personalized nursing, nurses formulate personalized health care plans, and determine the best treatment and nursing method by cooperating and exchanging opinions with patients and doctors (27).
The results of the 12 studies also indicated that personalized nursing has potential benefits for the anxiety and depression of patients in the perioperative period of hepatobiliary surgery. It may be that personalized nursing expands patients’ disease-related knowledge and nursing skills, thereby enhancing their confidence in nursing and alleviating their negative emotions of anxiety and depression (28).
This systematic review emphasized the clinical efficacy and postoperative recovery effects of personalized nursing, but also examined the anxiety and depression of these patients. In addition, this analysis only included RCTs with rigorous designs to ensure that the quality of the data was relatively high. However, this review had some limitations. First, personalized nursing is not clearly defined, the content and degree of personalized nursing vary greatly, and the tools for measuring outcome variables are also diverse. Second, some indicators of the included studies were significantly heterogeneous. Due to the limited number of studies, it was not possible to conduct further subgroup analyses to investigate the potential confounding factors of studies with high heterogeneity.
In short, the application of personalized nursing to patients undergoing hepatobiliary surgery during the perioperative period improved patients’ levels of satisfaction with nursing, effectively reduced the incidence of adverse reactions, accelerated the recovery of hepatobiliary function after surgery, and relieved anxiety and depression. Thus, it is worthy of clinical application, and should be adopted in clinical settings in the future to promote treatment and recovery.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://dx.doi.org/10.21037/apm-21-1923
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/apm-21-1923). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Liu J, Liu X. Abdominal abscess caused by acute cholecystitis. Hepatobiliary Surg Nutr 2019;8:677-8. [Crossref] [PubMed]
- Sato M, Tateishi R, Yasunaga H, et al. Mortality and morbidity of hepatectomy, radiofrequency ablation, and embolization for hepatocellular carcinoma: a national survey of 54,145 patients. J Gastroenterol 2012;47:1125-33. [Crossref] [PubMed]
- Kimura W, Miyata H, Gotoh M, et al. A pancreaticoduodenectomy risk model derived from 8575 cases from a national single-race population (Japanese) using a web-based data entry system: the 30-day and in-hospital mortality rates for pancreaticoduodenectomy. Ann Surg 2014;259:773-80. [Crossref] [PubMed]
- Edwards JR, Peterson KD, Mu Y, et al. National Healthcare Safety Network (NHSN) report: data summary for 2006 through 2008, issued December 2009. Am J Infect Control 2009;37:783-805. [Crossref] [PubMed]
- Nakahira S, Shimizu J, Miyamoto A, et al. Proposal for a sub-classification of hepato-biliary-pancreatic operations for surgical site infection surveillance following assessment of results of prospective multicenter data. J Hepatobiliary Pancreat Sci 2013;20:504-11. [Crossref] [PubMed]
- Yang T, Tu PA, Zhang H, et al. Risk factors of surgical site infection after hepatic resection. Infect Control Hosp Epidemiol 2014;35:317-20. [Crossref] [PubMed]
- Al-Mukhtar A, Wong VK, Malik HZ, et al. A simple prophylaxis regimen for MRSA: its impact on the incidence of infection in patients undergoing liver resection. Ann R Coll Surg Engl 2009;91:35-8. [Crossref] [PubMed]
- Wright AR, Richardson AB, Kikuchi CK, et al. Effectiveness of Accelerated Recovery Performance for Post-ACL Reconstruction Rehabilitation. Hawaii J Health Soc Welf 2019;78:41-6. [PubMed]
- American Geriatrics Society Expert Panel on Person-Centered Care. Person-Centered Care: A Definition and Essential Elements. J Am Geriatr Soc 2016;64:15-8. [Crossref] [PubMed]
- Berg A, Suhonen R, Idvall E. A survey of orthopaedic patients' assessment of care using the Individualised Care Scale. Journal of Orthopaedic Nursing 2007;11:185-93. [Crossref]
- Charalambous A, Katajisto J, Välimäki M, et al. Individualised care and the professional practice environment: nurses' perceptions. Int Nurs Rev 2010;57:500-7. [Crossref] [PubMed]
- Suhonen R, Efstathiou G, Tsangari H, et al. Patients' and nurses' perceptions of individualised care: an international comparative study. J Clin Nurs 2012;21:1155-67. [Crossref] [PubMed]
- Ge LL. AppIication of the individuaIized nursing strategy in patients with hepatobiIiary surgery. Journal of Qilu Nursing 2016;22:33-4.
- Zhang CY. Application value analysis of individualized nursing strategy in perioperative period of hepatobiliary surgery. Hebei Medical Journal 2016;38:631-3.
- Huo XY. Application value of individualized nursing strategy in perioperative period of hepatobiliary surgery. Capital Medicine 2017;24:93-4.
- Shan HX, Zhou F. Application value of individualized nursing strategy in perioperative period of hepatobiliary surgery. Clinical Research and Practice 2017;2:149-50.
- Zheng JX, Jiang XQ. Observation on the application effect of individualized nursing strategy in perioperative period of hepatobiliary surgery. Guide of China Medicine 2019;17:367-8.
- Li T. Application value of individualized nursing countermeasures in perioperative period of hepatobiliary surgery. World Latest Medicine Information 2016;16:242-3.
- Liao CM. Study on the value of individualized nursing intervention in perioperative patients of hepatobiliary surgery. Jilin Medical Journal 2014;35:7936-7.
- Liu H, Liao LR, Luo WY, et al. Application of individualized nursing intervention in patients with perioperative period in department of hepatobiliary surgery. China Medicine and Pharmacy 2015;5:119-21.
- Zhang LM. Observation on the effect of individualized nursing in perioperative period of hepatobiliary surgery. Gansu Medical Journal 2017;36:158-9.
- Chen YJ. Discuss the Effect of Personalized Nursing Combined with Psychological Behavior Intervention on Postoperative Recovery of Patients with Hepatobiliary Surgery During Perioperative Period. Medical Innovation of China 2019;16:99-102.
- Zhou CM, Liu N. Application value of individualized nursing strategy in perioperative nursing of Hepatobiliary Surgery. Cardiovascular Disease Journal of Integrated Traditional Chinese and Western Medicine (Electronic) 2020;8:6-7, 9.
- Shen YL, Ma Qianhong, Wang YY, et al. The clinical application of perioperative individualized nursing intervention in the nursing of hepatobiliary surgery. Journal of General Surgery for Clinicians 2020;8:37-40. (Electronic Version).
- Willems S, De Maesschalck S, Deveugele M, et al. Socio-economic status of the patient and doctor-patient communication: does it make a difference? Patient Educ Couns 2005;56:139-46. [Crossref] [PubMed]
- Charalambous A. Variations in patient satisfaction with care for breast, lung, head and neck and prostate cancers in different cancer care settings. Eur J Oncol Nurs 2013;17:588-95. [Crossref] [PubMed]
- Beck SL, Brant JM, Donohue R, et al. Oncology Nursing Certification: Relation to Nurses' Knowledge and Attitudes About Pain, Patient-Reported Pain Care Quality, and Pain Outcomes. Oncol Nurs Forum 2016;43:67-76. [Crossref] [PubMed]
- Wang QC. The construction of demand-oriented clinical nurses' psychological nursing training knowledge system. The Second Military Medical University, 2020.
(English Language Editor: L. Huleatt)