
Differences in clinical features of hypertrophic cardiomyopathy with or without left ventricular enlargement
Introduction
Hypertrophic cardiomyopathy (HCM) is a myocardial disease inherited in an autosomal dominant manner (1). While most patients remain stable during their daily life, a small proportion of patients have decreased systolic function after ventricular remodeling, which will evolve into end-stage HCM (ES-HCM). Although most HCM patients have normal life expectancy and controllable symptoms, some patients have an increased risk of heart failure and sudden cardiac death (2). Pharmacological therapies, surgical interventions including septal reduction and implantable cardioverter-defibrillators are the main treatment for HCM at present (3). The most widely used medicine for HCM include β-adrenergic receptor blockers and Ca2+ channel blockers (4), and the surgical interventions is only applicable to severe cases.
The current diagnostic criteria for ES-HCM is HCM with a left ventricular ejection fraction (LVEF) of <50% (5-7), and ES-HCM patients with a left ventricular end-diastolic diameter (LVEDd) of >55 mm are diagnosed with dilated end-stage of HCM (D-ES). Most HCM patients have milder symptoms with a mortality rate of only 1% (8), but as the end-stage of HCM, ES-HCM has a significantly higher mortality than HCM (1% vs. 9%) (5). The therapeutic options for ES-HCM are very limited and patient prognosis is poor, so it is crucial to improve our understanding of ES-HCM and its early diagnosis. At present, it is considered that the echocardiographic manifestations of ES-HCM and dilated cardiomyopathy (DCM) are similar. The accurate diagnostic method to ES-HCM is echocardiography combined with other diagnostic tools such as CMR, radionuclide myocardial scintigraphy, and myocardial biopsy (1).
HCM with enlarged left ventricle (ELV) accompanied by reduced LVEF is defined as D-ES, but patients with ELV and normal LVEF are diagnosed as having HCM (9). Few studies have focused on whether HCM patients with ELV exhibit unique clinical features. HCM can be divided into two types—obstructive [hypertrophic obstructive cardiomyopathy (HOCM)] and non-obstructive (non-obstructive HCM). The majority of HCM cases with myocardial hypertrophy mainly occur in the ventricular septum, namely asymmetric septal HCM (ASHCM). Apical HCM (ApHCM) is a rare type of HCM, and its hypertrophy primarily involves the apex of the left ventricle, usually without left ventricular outflow tract obstruction and pressure gradient. A previous study compared the clinical characteristics and prognosis of patients with ApHCM and ASHCM (10), while none have reported on the clinical characteristics of patients with ELV. Thus, the present study aims to analyze and investigate the clinical features of different types of HCM in ELV patients. We present the following article in accordance with the STROBE reporting checklist (available at https://dx.doi.org/10.21037/apm-21-2304).
Methods
Subjects
A retrospective analysis was performed on patients diagnosed with HCM who visited the outpatient and inpatient departments of Peking University People’s Hospital from December 2015 to July 2018. The patients’ study data were collected from medical records and echocardiographic data recorded in the electronic medical record system. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee, and with the Helsinki Declaration (as revised in 2013). The authors confirm that the procedures followed were assessed by the Ethics Committee of the First Affiliated Hospital of Hunan Normal University (approval No. 20160528-1), and informed consent was obtained from all patients.
Study groups
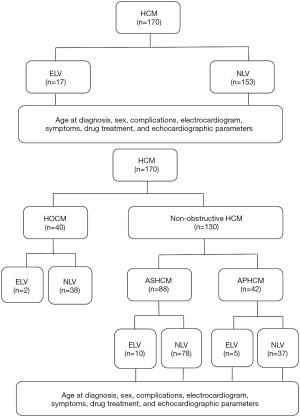
Subjects with HCM were divided into two groups: ELV and normal left ventricle (NLV), according to left ventricle size. An intergroup comparison was performed in terms of the age at disease diagnosis, sex, complications, electrocardiogram (ECG) findings, symptoms, drug treatment, and echocardiographic parameters of the subjects in both groups.
Patients with non-obstructive HCM were divided into ASHCM and ApHCM groups, and both ASHCM and ApHCM were further subdivided into two subgroups: an ELV group and an NLV group, and the above indicators were compared and analyzed (see Figure 1 for specific study procedure).
Diagnostic criteria
HCM was diagnosed based on the 2014 European Society of Cardiology guidelines (11). The diagnostic criteria were mainly based on echocardiographic findings: the presence of otherwise unexplained increased left ventricular wall and (or) ventricular septal wall thickness ≥15 mm.
Diagnostic criteria of ES-HCM
An LVEF <50% in HCM patients as indicated by echocardiography during the follow-up examination. The exclusion criteria were as follows: (I) subjects with a history of septal reduction therapy (including alcohol septal ablation and septal myectomy); (II) subjects with a history of coronary heart disease (CHD); and (III) subjects with coronary stenosis ≥50% in one or more vessels, as measured by selective coronary angiography or coronary computed tomography.
HCM with ELV
Subjects with a clear history of HCM who experienced enlargement in the left heart during disease progression, with a LVEDd >55 mm measured at the parasternal left ventricular long-axis view as indicated by a heart color ultrasound, with or without reduced LVEF.
ApHCM
The site of cardiac hypertrophy, mainly involving the left ventricular apex, with an end-diastolic apical thickness ≥15 mm or a maximum apical thickness/left ventricular posterior wall thickness (LVPWT) ≥1.5.
ASHCM
The site of hypertrophy mainly at interventricular septum, with a left ventricular end-diastolic septum thickness ≥15 mm, or a maximum interventricular septum thickness (IVST)/LVPWT ≥1.3. Patients with mixed HCM and hypertrophic HCM were excluded (12,13).
Echocardiography
Echocardiographic images and data were acquired using the Vivid 9, GE Vingmed (GE Healthcare, Little Chalfont, Buckinghamshire, UK) by an experienced physician employing 2.5- and 3.5-MHz probes. Echocardiographic images were acquired according to the 2019 American Society of Echocardiography guidelines (14).
Statistical analysis
The SPSS17.0 statistical package (IBM, Armonk, NY, USA) was used for data analysis. Measurement data were expressed as mean ± standard deviation, and enumeration data were expressed as frequency or percentage (%). Comparisons between the measurement data groups were performed using the independent t-test. Enumeration data were tested using the chi-square method or Fisher’s exact test. P<0.05 was considered to indicate a statistically significant difference.
Results
Clinical features and echocardiographic parameters of ELV and NLV in HCM patients
A total of 170 HCM patients were enrolled, including 40 with HOCM and 130 with non-obstructive HCM. Among all patients with non-obstructive HCM, 88 cases were ASHCM and 42 cases were ApHCM. Nine patients had ES-HCM, representing a morbidity rate of 5.29% in HCM. A total of 17 patients had ELV; of these, 2 had HOCM, 10 had non-obstructive ASHCM, and 5 had ApHCM. Of the 17 patients with ELV, 3 were accompanied by ES-HCM; of which, 1 was in the HOCM group (representing a morbidity rate of 2.5%), 2 were in the non-obstructive ASHCM group (representing a morbidity rate of 2.27%), and none were in the AHCM group. The ELV group exhibited a higher morbidity rate of ES-HCM than the NLV group (17.65% vs. 3.92%), and the difference was statistically significant (P=0.048). Compared to the NLV group, the ELV group exhibited no significant differences in clinical symptoms, age at disease diagnosis, hospitalization rate, complications, and ECG changes. The ELV group had a markedly higher proportion of male patients than the NLV group (94.12% vs. 60.13%, P=0.006).
As for drug treatment, there were no significant differences between the two groups with respect to angiotensin converting enzyme inhibitor (ACEI)/angiotensin receptor blocker (ARB), β-blocker, calcium channel blocker (CCB), aspirin/clopidogrel, and statins. However, diuretics were more frequently used in the ELV group than in the NLV group (41.18% vs. 10.46%, P=0.003). The ELV group had a notably higher percentage of subjects receiving pacemaker placement compared to the NLV group (41.18% vs. 16.99%, P=0.025) (Table 1).
Table 1
| Characteristics | ELV (n=17) | NLV (n=153) | P |
|---|---|---|---|
| Male, No. (%) | 16 (94.12) | 92 (60.13) | 0.006 |
| Age at diagnosis, y | 49.87±17.606 | 56.47±18.440 | 0.194 |
| All-cause hospitalization, No. (%) | 12 (70.59) | 79 (51.63) | 0.200 |
| HCM hospitalization, No. (%) | 6 (35.29) | 31 (20.26) | 0.211 |
| Choking sensation in chest, No. (%) | 2 (11.76) | 29 (18.95) | 0.741 |
| Angina pectoris, No. (%) | 1 (5.88) | 8 (5.23) | 1.000 |
| Palpitation, No. (%) | 0 | 16 (10.46) | NA |
| Syncope, No. (%) | 2 (11.76) | 7 (4.78) | 0.240 |
| Complication, No. (%) | |||
| HTN | 5 (29.41) | 52 (33.99) | 0.793 |
| CHD | 2 (11.76) | 19 (12.42) | 1.000 |
| T2DM | 2 (11.76) | 18 (11.76) | 1.000 |
| Hyperlipemia | 4 (23.53) | 17 (11.11) | 0.233 |
| ECG, No. (%) | |||
| Af | 3 (17.65) | 18 (11.76) | 0.437 |
| Any negative T wave | 7 (41.18) | 56 (36.60) | 0.793 |
| LVHV | 2 (11.76) | 19 (12.42) | 1.000 |
| Abnormal Q wave | 1 (5.88) | 4 (2.61) | 0.413 |
| LBBB | 0 | 3 (1.96) | NA |
| RBBB | 0 | 10 (6.53) | NA |
| Medications, No. (%) | |||
| ACEI/ARB | 8 (47.06) | 50 (32.68) | 0.283 |
| β-blocker | 12 (70.59) | 77 (50.33) | 0.131 |
| Diuretics | 7 (41.18) | 16 (10.46) | 0.003 |
| CCB | 6 (35.29) | 45 (29.41) | 0.589 |
| Aspirin/clopidogrel | 7 (41.18) | 40 (26.14) | 0.251 |
| Statin | 3 (17.65) | 28 (18.30) | 1.000 |
| Procedures, No. (%) | |||
| Pacemaker | 7 (41.18) | 26 (16.99) | 0.025 |
| ICD | 3 (17.65) | 8 (5.23) | 0.083 |
| LVEF <50%, No. (%) | 3 (17.65) | 6 (3.92) | 0.048 |
HCM, hypertrophic cardiomyopathy; ELV, enlarged left ventricle; NLV, normal left ventricle; HTN, hypertension; CHD, coronary heart disease; T2DM, type 2 diabetes mellitus; ECG, electrocardiogram; Af, atrial fibrillation; LVHV, left ventricular high voltage; LBBB, left bundle branch block; RBBB, right bundle branch block; ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin receptor blocker; CCB, calcium channel blocker; ICD, implantable cardioverter defibrillator; LVEF, left ventricular ejection fraction; NA, data not available.
The ELV group had significantly lower aortic max velocity (AoVmax), left ventricular outflow tract pressure gradient (LVOT PG), and peak end-diastolic mitral flow velocity (VA) than the NLV group (P=0.014, 0.032, and 0.026, respectively). Moreover, the ELV group also had markedly larger end-diastolic volume (EDV), end-systolic volume (ESV), LVEDd, and left ventricular end-systolic diameter (LVESd) (P=0.000, 0.000, 0.000, and 0.004, respectively), and significantly smaller LVEF (P=0.000) than the NLV group. Furthermore, the ELV group had a notably larger left atrial diameter (LAd) than the NLV group (43.77±7.23 vs. 39.77±6.32 mm, P=0.016). There were no significant differences between the two groups with respect to IVST, LVPWT, ascending aortic diameter, peak early-diastolic mitral flow velocity (VE), aortic max pressure gradient (AomaxPG), and left ventricular outflow tract velocity (LVOTV) (Table 2).
Table 2
| Characteristics | ELV (n=17) | NLV (n=153) | P |
|---|---|---|---|
| AOVmax, cm/s | 118.69±54.95 | 152.67±53.03 | 0.014 |
| AOmaxPG, mmHg | 7.69±3.93 | 10.48±9.39 | 0.243 |
| ascAorta, mm | 31.00±4.06 | 30.44±6.23 | 0.721 |
| LVOTV, cm/s | 161.25±95.38 | 245.76±153.44 | 0.174 |
| LVOT PG, mmHg | 13.21±13.48 | 35.46±36.81 | 0.032 |
| EDV, mL | 173.85±21.92 | 97.94±25.74 | 0.000 |
| ESV, mL | 69.13±24.17 | 31.23±11.85 | 0.000 |
| LVEF, % | 59.04±12.73 | 68.14±8.32 | 0.000 |
| IVST, mm | 17.32±10.54 | 16.25±5.84 | 0.517 |
| LAd, mm | 43.77±7.23 | 39.77±6.32 | 0.016 |
| LVEDd, mm | 59.20±3.20 | 45.67±5.52 | 0.000 |
| LVESd, mm | 37.03±10.82 | 28.33±4.39 | 0.004 |
| LVPWT, mm | 10.55±1.86 | 10.64±2.48 | 0.888 |
| VE, cm/s | 68.28±28.16 | 78.23±26.79 | 0.162 |
| VA, cm/s | 62.70±22.87 | 81.34±31.13 | 0.026 |
HCM, hypertrophic cardiomyopathy; ELV, enlarged left ventricle; NLV, normal left ventricle; AOVmax, aortic max velocity; AOmaxPG, aortic max pressure gradient; ascAorta, ascending aorta; LVOTV, left ventricular outflow tract velocity; LVOT PG, left ventricular outflow tract pressure gradient; EDV, end-diastolic volume; ESV, end-systolic volume; LVEF, left ventricular ejection fraction; IVST, interventricular septum thickness; LAd, left atrial diameter; LVEDd, left ventricular end-diastolic diameter; LVESd, left ventricular end-systolic diameter; LVPWT, left ventricular posterior wall thickness; VE, peak early-diastolic mitral flow velocity; VA, peak end-diastolic mitral flow velocity.
Clinical features and echocardiographic parameters of ELV and NLV in patients with non-obstructive ASHCM
Of the patients with non-obstructive ASHCM, 10 had ELV and 78 had NLV. The ELV group had a significantly higher proportion of male patients than the NLV group (100% vs. 65.38%, P=0.028). There were no notable differences between the two groups in terms of clinical symptoms, age at disease diagnosis, hospitalization rate, complications, and ECG changes.
As for drug treatment, there was no significant differences between the two groups with respect to ACEI/ARB, β-blocker, CCB, aspirin/clopidogrel, and statins, but diuretics were more frequently used in the ELV group than in the NLV group (50% vs. 11.54%, P=0.008). The ELV group had a markedly higher percentage of subjects receiving implantable cardioverter defibrillator (ICD) placement compared to the NLV group (30% vs. 6.41%, P=0.044) (Table 3).
Table 3
| Characteristics | ASHCM | ApHCM | |||||
|---|---|---|---|---|---|---|---|
| ELV (n=10) | NLV (n=78) | P | ELV (n=5) | NLV (n=37) | P | ||
| Male, no. (%) | 10 (100.00) | 51 (65.38) | 0.028 | 4 (80.00) | 22 (59.46) | 0.633 | |
| Age at diagnosis, y | 50.75±14.695 | 54.16±18.122 | 0.616 | 54.40±12.198 | 61.14±18.719 | 0.453 | |
| All-cause hospitalization, no. (%) | 6 (60.00) | 41 (52.56) | 0.745 | 4 (80.00) | 14 (37.84) | 0.146 | |
| HCM hospitalization, no. (%) | 4 (40.00) | 13 (16.67) | 0.096 | 1 (20.00) | 1 (2.70) | 0.226 | |
| Choking sensation in chest, no. (%) | 1 (10.00) | 14 (17.95) | 1.000 | 1 (20.00) | 3 (8.11) | 0.41 | |
| Angina pectoris, no. (%) | 0 | 2 (2.56) | NA | 0 | 4 (10.81) | NA | |
| Palpitation, no. (%) | 0 | 6 (7.69) | NA | 0 | 6 (16.22) | NA | |
| Syncope, no. (%) | 1 (10.00) | 5 (6.41) | 0.526 | 0 | 0 | NA | |
| Complication, no. (%) | |||||||
| HTN | 3 (30.00) | 28 (35.90) | 1.000 | 1 (20.00) | 14 (37.84) | 0.639 | |
| CHD | 1 (10.00) | 13 (16.67) | 1.000 | 1 (20.00) | 3 (8.11) | 0.41 | |
| T2DM | 1 (10.00) | 13 (16.67) | 1.000 | 1 (20.00) | 1 (2.70) | 0.226 | |
| Hyperlipemia | 3 (30.00) | 9 (11.54) | 0.134 | 2 (40.00) | 5 (13.51) | 0.188 | |
| ECG, no. (%) | |||||||
| Af | 1 (10.00) | 6 (7.69) | 0.584 | 3 (60.00) | 5 (13.51) | 0.04 | |
| Any negative T wave | 3 (30.00) | 28 (35.90) | 1.000 | 5 (100.00) | 14 (37.84) | 0.014 | |
| LVHV | 2 (20.00) | 8 (10.26) | 0.317 | 0 | 6 (16.22) | NA | |
| Abnormal Q wave | 1 (10.00) | 4 (5.13) | 0.461 | 0 | 0 | NA | |
| LBBB | 0 | 0 | NA | ||||
| RBBB | 0 | 5 (6.41) | NA | 1 (20.00) | 2 (5.41) | 0.323 | |
| Medications, no. (%) | |||||||
| ACEI/ARB | 1 (10.00) | 30 (38.46) | 0.091 | 5 (100.00) | 15 (40.54) | 0.018 | |
| β-blocker | 6 (60.00) | 40 (51.28) | 0.742 | 4 (80.00) | 16 (43.24) | 0.174 | |
| Diuretics | 5 (50.00) | 9 (11.54) | 0.008 | 1 (20.00) | 3 (8.10) | 0.41 | |
| CCB | 2 (20.00) | 26 (33.33) | 0.493 | 3 (60.00) | 11 (29.73) | 0.313 | |
| Aspirin/clopidogrel | 3 (30.00) | 18 (23.08) | 0.697 | 3 (60.00) | 13 (35.14) | 0.352 | |
| Statin | 1 (10.00) | 16 (20.51) | 0.679 | 2 (40.00) | 8 (21.62) | 0.577 | |
| Procedures, no. (%) | |||||||
| Pacemaker | 4 (40.00) | 18 (23.08) | 0.260 | 2 (40.00) | 3 (8.10) | 0.099 | |
| ICD | 3 (30.00) | 5 (6.41) | 0.044 | 0 | 0 | NA | |
ASHCM, asymmetric septal HCM; ApHCM, apical HCM; HCM, hypertrophic cardiomyopathy; ELV, enlarged left ventricle; NLV, normal left ventricle; HTN, hypertension; CHD, coronary heart disease; T2DM, type 2 diabetes mellitus; ECG, electrocardiogram; Af, atrial fibrillation; LVHV, left ventricular high voltage; LBBB, left bundle branch block; RBBB, right bundle branch block; ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin receptor blocker; CCB, calcium channel blocker; ICD, implantable cardioverter defibrillator; NA, data not available.
The ELV group had significantly larger EDV, ESV, LVEDd, and LVESd (P=0.000, 0.001, 0.000, 0.000, respectively), and considerably smaller LVEF (56.93%±13.21% vs. 66.85%±8.55%, P=0.002) than the NLV group. Moreover, there were no statistically significant differences between the two groups in AoVmax, AomaxPG, ascending aorta diameter, LVOTV, LVOT PG, IVST, LAd, LVPWT, main pulmonary artery diameter (MPAd), VE, and VA (Table 4).
Table 4
| Echo | ASHCM | ApHCM | |||||
|---|---|---|---|---|---|---|---|
| ELV (n=10) | NLV (n=78) | P | ELV (n=5) | NLV (n=37) | P | ||
| AOVmax, cm/s | 122.39±26.61 | 137.86±32.49 | 0.154 | 115.40±67.89 | 132.49±32.20 | 0.607 | |
| AOmaxPG, mmHg | 6.25±2.65 | 8.024±4.35 | 0.213 | 8.40±2.54 | 7.5757±3.82 | 0.644 | |
| ascAorta, mm | 30.31±4.13 | 29.55±7.37 | 0.750 | 32.10±4.21 | 31.81±4.86 | 0.899 | |
| LVOTV, cm/s | 120.33±60.00 | 116.96±39.32 | 0.892 | NA | 153.00±38.18 | NA | |
| LVOT PG, mmHg | 6.94±6.085 | 5.90±4.0 | 0.677 | NA | 9.50±4.95 | NA | |
| EDV, mL | 173.44±18.74 | 96.08±25.93 | 0.000 | 178.27±33.20 | 109.80±21.42 | 0.000 | |
| ESV, mL | 75.52±27.26 | 32.51±12.96 | 0.001 | 56.94±9.27 | 31.77±10.32 | 0.000 | |
| LVEF, % | 56.93±13.21 | 66.85±8.55 | 0.002 | 66.00±7.72 | 70.27±6.23 | 0.169 | |
| IVST, mm | 15.74±3.40 | 18.08±5.26 | 0.176 | 20.94±19.82 | 10.98±2.38 | 0.324 | |
| LAd, mm | 43.10±7.90 | 39.72±6.27 | 0.123 | 44.30±5.61 | 37.86±5.46 | 0.018 | |
| LVEDd, mm | 58.94±2.73 | 45.30±5.70 | 0.000 | 59.20±4.15 | 48.04±4.26 | 0.000 | |
| LVESd, mm | 40.79±6.10 | 28.79±4.77 | 0.000 | 37.14±2.40 | 28.79±3.27 | 0.000 | |
| LVPWT, mm | 10.63±2.20 | 10.81±2.66 | 0.835 | 10.13±1.46 | 9.77±2.088 | 0.707 | |
| MPAd, mm | 19.79±10.68 | 21.68±6.46 | 0.596 | 23.00±3.37 | 23.22±2.81 | 0.884 | |
| VE, cm/s | 71.45±33.98 | 74.54±25.63 | 0.731 | 65.330±16.36 | 73.61±17.61 | 0.327 | |
| VA, cm/s | 61.01±20.070 | 76.11±32.73 | 0.182 | 58.81±26.49 | 82.93±26.25 | 0.065 | |
| LVAT, mm | NA | NA | NA | 18.50±6.61 | 17.98±3.27 | 0.795 | |
ASHCM, asymmetric septal HCM; ApHCM, apical HCM; HCM, hypertrophic cardiomyopathy; ELV, enlarged left ventricle; NLV, normal left ventricle; AOVmax, aortic max velocity; AOmaxPG, aortic max pressure gradient; ascAorta, ascending aorta; LVOTV, left ventricular outflow tract velocity; LVOT PG, left ventricular outflow tract pressure gradient; EDV, end-diastolic volume; ESV, end-systolic volume; LVEF, left ventricular ejection fraction; IVST, interventricular septum thickness; LAd, left atrial diameter; LVEDd, left ventricular end-diastolic diameter; LVESd, left ventricular end-systolic diameter; LVPWT, left ventricular posterior wall thickness; MPAd, main pulmonary artery diameter; VE, peak early-diastolic mitral flow velocity; VA, peak end-diastolic mitral flow velocity; LVAT, left ventricular apical thickness; NA, data not available.
Clinical features and echocardiographic parameters of ELV and NLV in ApHCM patients
Of the patients with ApHCM, five had ELV and 37 had NLV. There were no notable differences between the ELV and NLV groups in terms of the proportion of male patients (80% vs. 59.46%, P=0.633). Also, no significant differences were observed between the two groups with respect to clinical symptoms, age at disease diagnosis, hospitalization rate, and complications. ECG changes mainly included atrial fibrillation (Af) and ST-T changes. The ELV group had a markedly higher incidence rate of Af than the NLV group (60% vs. 13.51%, P=0.04). There was a significant difference in the incidence rate of ST-T changes between the ELV and NLV groups (100% vs. 13.51%, P=0.014).
In terms of drug treatment, the ELV group had a considerably higher rate of ACEI/ARB use than the NLV group (100% vs. 40.54%, P=0.018). There was no statistically significant difference between the two groups in terms of the percentage of subjects receiving pacemaker placement (Table 3).
For patients with ApHCM, the ELV group had significantly larger EDV, ESV, LVEDd, and LVESd (all P=0.000) compared to the NLV group. The ELV group also had a markedly larger LAd than the NLV group (44.30±5.61 vs. 37.86±5.46 mm, P=0.018). Furthermore, the ELV group had a lower LVEF than the NLV group, but the difference between the groups was not statistically significant (66.00%±7.72% vs. 70.27%±6.23%, P=0.169). There were no significant differences between the two groups in terms of AoVmax, AomaxPG, ascending aortic diameter, IVST, LVPWT, MPAd, VE, and VA (Table 4).
Discussion
As is shown in previous studies, the morbidity rate of HCM in the general population is 1:500; however, thus far, there have been no reports regarding the morbidity rate of ES-HCM in the general population. According to previous reports, the morbidity rate of ES-HCM among patients with HCM patients is 2.4–15.7% (5,7,15-17). The evolution from HCM to ES-HCM is gradual. Approximately 75% of patients with HCM maintain a LVEF of >65% for a longer period of time, with (mild) or without myocardial fibrosis. The progression of disease is synchronized with the gradual occurrence of myocardial remodeling, with LVEF ranging from 50% to 65% and increased myocardial fibrosis. At this stage, the left ventricular wall gradually becomes thinner (at a rate of approximately 1–2 mm/year), the left internal diameter gradually increases (at approximately 1–4 mm/year), and the LVEF decreases (18). Studies have reported that the lag time between the onset of clinical symptoms and confirming diagnosis of HCM for the first time lasts several years, usually 5–6 years, and 5–10% of patients with HCM will go on to develop ES-HCM (5,7,19).
The morbidity rate of ES-HCM among patients with HCM in this study was 5.29%, which is similar to that described in previous studies (20). The morbidity rates of ES-HCM among patients with HOCM, non-obstructive ASHCM, and ApHCM were 2.5%, 2.27%, and 0, respectively. This result indicated that patients with ApHCM had relatively mild symptoms and were less likely to evolve to the ES-HCM stage than those with HOCM and non-obstructive ASHCM. The morbidity rate of ES-HCM among ELV patients (17.65%) was significantly higher than that in the overall HCM population, indicating that the ELV patients had a higher risk of evolving to ES-HCM. Tunca Sahin et al. investigated the morbidity rate in 152 children patients with HCM, and they found that three cases (2%) of HCM showed similar manifestations of dilated heart disease during the course of the disease (21). It suggested that there are some differences in the prevalence of ES-HCM between adults and children.
Age and sex affected the left ventricular dimension and LVOT PG of patients with HCM, while ELV had a certain effect on LVEF. Previous studies have shown that patients with HCM aged ≤50 years had no significant gender-related differences in LVOT PG (22). For patients with HOCM aged >50 years, males had a significantly lower LVOT PG as well as markedly larger LVEDd and LVESd than females, but there were no significant differences between male and female patients with respect to LVEDd/body surface area (BSA) and LVESd/BSA (19,23).
The results of this study showed that the proportion of male patients with ELV was notably higher among the overall HCM population and in those with non-obstructive ASHCM; however, this could not completely rule out the effect of sex-related BSA differences on the results. This result provided indirect evidence that male patients with HCM were more prone to ELV; moreover, whether male patients with HCM are more likely to evolve to ES-HCM remains to be further studied.
Of the enrolled patients with HCM, the ELV group had a significantly higher proportion of male patients and a markedly lower LVOT PG compared to the NLV group, which was somewhat similar to previous studies (23,24). Furthermore, Mitra et al. conducted a similar study to determine the prevalence and outcomes in HCM patients with pulmonary hypertension (PH), and they found that the prevalence of PH increased progressively in HCM patients without LVOT obstruction, HCM patients with LVOT obstruction, HCM patients diagnosed at age ≥65 years and ES-HCM patients (25). However, in this study we didn’t make further comparative analysis due to the limited samples of different types of HCM combined with PH.
In addition, this study revealed that patients with non-obstructive ASHCM with ELV had a significantly decreased LVEF compared to those with NLV, and the use of symptom-improving diuretics was significantly increased. Also, the LVEF decrease in ApHCM patients with ELV was not notably different to those with NLV, and there was no significant increase in the use of diuretics. Studies have demonstrated that ELV has a certain effect on LVEF, but this effect varies among different variants of HCM (26).
Data has shown that 75–95% of patients with HCM experience ECG abnormalities, mainly characterized by ST-segment changes [inverted T wave and abnormal Q waves (27)] as well as complex arrhythmias such as ventricular tachycardia, multifocal ventricular premature beats, and Af (28). The present study revealed that major ECG changes in HCM patients included Af and ST-T changes. Of the patients with AHCM, those with ELV had significant enlargement in the left atrium, as well as markedly higher incidence rates of Af and ST-T changes, and rate of ACEI/ARB use, compared to those with NLV. Among patients with non-obstructive ASHCM, there were no notably differences between the ELV and NLV groups in terms of left atrial size, incidence rates of Af, ST-T change, and rate of ACEI/ARB use. Studies have shown that ELV could affect the myocardial electrophysiology of patients with ApHCM. Since ApHCM patients have relatively mild clinical symptoms, the main therapeutic measure for improving myocardial remodeling is ACEI/ARB.
Limitations of the study
HCM diagnosis was only based on clinical phenotypes and no genetic evidence could be provided. Also, this study was a single-center retrospective study with a limited sample size.
Conclusions
The incidence rate of ES-HCM among patients with ApHCM was lower than that of patients with HOCM and non-obstructive ASHCM. The prevalence of ES-HCM in HCM patients with ELV was higher than those with NLV, and there was a higher proportion of male than female patients. Therefore, patients with different HCM variants have different clinical features.
Acknowledgments
Funding: This study was supported by a grant from the Hunan Provincial Special Fund for Health Care (B201603).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://dx.doi.org/10.21037/apm-21-2304
Data Sharing Statement: Available at https://dx.doi.org/10.21037/apm-21-2304
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/apm-21-2304). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee, and with the Helsinki Declaration (as revised in 2013). The authors confirm that the procedures followed were assessed by the Ethics Committee of the First Affiliated Hospital of Hunan Normal University (approval No. 20160528-1), and informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Maron BJ, Maron MS. Hypertrophic cardiomyopathy. Lancet 2013;381:242-55. [Crossref] [PubMed]
- Lee HJ, Kim HK, Kim M, et al. Clinical impact of atrial fibrillation in a nationwide cohort of hypertrophic cardiomyopathy patients. Ann Transl Med 2020;8:1386. [Crossref] [PubMed]
- Spoladore R, Maron MS, D'Amato R, et al. Pharmacological treatment options for hypertrophic cardiomyopathy: high time for evidence. Eur Heart J 2012;33:1724-33. [Crossref] [PubMed]
- Solomon T, Filipovska A, Hool L, et al. Preventative therapeutic approaches for hypertrophic cardiomyopathy. J Physiol 2021;599:3495-512. [Crossref] [PubMed]
- Harris KM, Spirito P, Maron MS, et al. Prevalence, clinical profile, and significance of left ventricular remodeling in the end-stage phase of hypertrophic cardiomyopathy. Circulation 2006;114:216-25. [Crossref] [PubMed]
- Olivotto I, Cecchi F, Poggesi C, et al. Patterns of disease progression in hypertrophic cardiomyopathy: an individualized approach to clinical staging. Circ Heart Fail 2012;5:535-46. [Crossref] [PubMed]
- Thaman R, Gimeno JR, Murphy RT, et al. Prevalence and clinical significance of systolic impairment in hypertrophic cardiomyopathy. Heart 2005;91:920-5. [Crossref] [PubMed]
- Maron BJ. Hypertrophic cardiomyopathy: a systematic review. JAMA 2002;287:1308-20. [Crossref] [PubMed]
- Ramineni R, Merla R, Chernobelsky A. Noncompaction of ventricular myocardium associated with hypertrophic cardiomyopathy and polycystic kidney disease. Am J Med Sci 2010;339:383-6. [Crossref] [PubMed]
- An S, Fan C, Yan L, et al. Comparison of long-term outcome between apical and asymmetric septal hypertrophic cardiomyopathy. Cardiology 2017;136:108-14. [Crossref] [PubMed]
- Özdemir MEuropean Society of Cardiology. 2014 European Society of Cardiology guidelines on hypertrophic cardiomyopathy. Turk Kardiyol Dern Ars 2014;42:693-7. [Crossref] [PubMed]
- Gersh BJ, Maron BJ, Bonow RO, et al. 2011 ACCF/AHA Guideline for the Diagnosis and Treatment of Hypertrophic Cardiomyopathy: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Developed in collaboration with the American Association for Thoracic Surgery, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol 2011;58:e212-60. [Crossref] [PubMed]
- Efthimiadis GK, Parcharidou D, Pagourelias ED, et al. Prevalence and clinical outcomes of incidentally diagnosed hypertrophic cardiomyopathy. Am J Cardiol 2010;105:1445-50. [Crossref] [PubMed]
- Wiegers SE, Ryan T, Arrighi JA, et al. 2019 ACC/AHA/ASE advanced training statement on echocardiography (revision of the 2003 ACC/AHA clinical competence statement on echocardiography): A Report of the ACC Competency Management Committee. Catheter Cardiovasc Interv 2019;94:481-505. [Crossref] [PubMed]
- Biagini E, Coccolo F, Ferlito M, et al. Dilated-hypokinetic evolution of hypertrophic cardiomyopathy: prevalence, incidence, risk factors, and prognostic implications in pediatric and adult patients. J Am Coll Cardiol 2005;46:1543-50. [Crossref] [PubMed]
- Spirito P, Maron BJ, Bonow RO, et al. Occurrence and significance of progressive left ventricular wall thinning and relative cavity dilatation in hypertrophic cardiomyopathy. Am J Cardiol 1987;60:123-9. [Crossref] [PubMed]
- Hina K, Kusachi S, Iwasaki K, et al. Progression of left ventricular enlargement in patients with hypertrophic cardiomyopathy: incidence and prognostic value. Clin Cardiol 1993;16:403-7. [Crossref] [PubMed]
- Maron BJ, Spirito P. Implications of left ventricular remodeling in hypertrophic cardiomyopathy. Am J Cardiol 1998;81:1339-44. [PubMed]
- Rogers DP, Marazia S, Chow AW, et al. Effect of biventricular pacing on symptoms and cardiac remodelling in patients with end-stage hypertrophic cardiomyopathy. Eur J Heart Fail 2008;10:507-13. [Crossref] [PubMed]
- Marian AJ, Tan Y, Li L, et al. Hypertrophy regression with n-acetylcysteine in hypertrophic cardiomyopathy (HALT-HCM): a randomized, placebo-controlled, double-blind pilot study. Circ Res 2018;122:1109-18. [Crossref] [PubMed]
- Tunca Sahin G, Ozgur S, Kafali HC, et al. Clinical characteristics of hypertrophic cardiomyopathy in children: an 8-year single center experience. Pediatr Int 2021;63:37-45. [Crossref] [PubMed]
- Zhang C, Liu R, Yuan J, et al. Gender-related differences in the association between serum uric acid and left ventricular mass index in patients with obstructive hypertrophic cardiomyopathy. Biol Sex Differ 2016;7:22. [Crossref] [PubMed]
- Dimitrow PP, Czarnecka D, Kawecka-Jaszcz K, et al. The influence of age on gender-specific differences in the left ventricular cavity size and contractility in patients with hypertrophic cardiomyopathy. Int J Cardiol 2003;88:11-6; discussion 16-7. [Crossref] [PubMed]
- Maron BJ, McKenna WJ, Danielson GK, et al. American College of Cardiology/European Society of Cardiology clinical expert consensus document on hypertrophic cardiomyopathy. A report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents and the European Society of Cardiology Committee for Practice Guidelines. J Am Coll Cardiol 2003;42:1687-713. [Crossref] [PubMed]
- Mitra A, Ghosh RK, Bandyopadhyay D, et al. Significance of pulmonary hypertension in hypertrophic cardiomyopathy. Curr Probl Cardiol 2020;45:100398 [Crossref] [PubMed]
- Zamani P, Akers S, Soto-Calderon H, et al. Isosorbide dinitrate, with or without hydralazine, does not reduce wave reflections, left ventricular hypertrophy, or myocardial fibrosis in patients with heart failure with preserved ejection fraction. J Am Heart Assoc 2017;6:004262 [Crossref] [PubMed]
- Patel SI, Ackerman MJ, Shamoun FE, et al. QT prolongation and sudden cardiac death risk in hypertrophic cardiomyopathy. Acta Cardiol 2019;74:53-8. [Crossref] [PubMed]
- Lyon A, Bueno-Orovio A, Zacur E, et al. Electrocardiogram phenotypes in hypertrophic cardiomyopathy caused by distinct mechanisms: apico-basal repolarization gradients vs. Purkinje-myocardial coupling abnormalities. Europace 2018;20:iii102-12. [Crossref] [PubMed]
(English Language Editor: A. Kassem)


