
Percutaneous minimally invasive treatment of transverse patellar fracture using cannulated screws combined with high-strength sutures and Nice knots: a retrospective study
Introduction
The patella is the largest sesamoid bone in the human body. As an important component of the knee extensor mechanism, the patella plays a key role in increasing the moment arm of the quadriceps tendon, protecting the articular surface, and maintaining the appearance of the knee joint (1). Patellar fracture is an intra-articular fracture, accounts for about 1% of all fractures in adults, and is most commonly caused by direct, indirect, or mixed forces (2). At present, it is widely accepted that the surgical indications for patellar fracture include a fracture displacement >3 mm, combined ligament injury, an articular step-off >2 mm, and an open fracture (3). The goal of surgical treatment of the patellar fracture is to restore the smoothness of the articular surface, and the integrity of the knee extension mechanism to enable knee joint function to recover sufficiently to satisfy the patients’ needs in life and work.
The Kirschner wire combined with tension band wiring is a classic method for the treatment of patellar fractures in clinical settings, and this approach can be applied to almost all types of patellar fractures (4). After fixing the patella using this method, the knee extensor muscles convert the tension on the patella surface into axial pressure on the fractured end to promote fracture healing when the patient flexes and extends the knee joint. Currently, a modified treatment method for patellar fracture that combines cannulated screws with tension band wiring is widely used around the world (5). Compared to Kirschner wire, cannulated screws show better stability in the fixation of a patellar fracture, and have lower incidences of needle withdrawal and deformation (6). However, the steel wire used in these two techniques can easily cause a stimulation reaction in soft tissues, which seriously affects the function of the knee joint and patients’ quality of life. Additionally, due to soft-tissue stimulation complications and the future need for clinical examinations [such as magnetic resonance imaging (MRI)], the internal fixation is often removed in a 2nd operation after fracture healing, which increases patients’ medical costs.
To address these disadvantages, we utilized a minimally invasive technique for the treatment of transverse patellar fractures by using cannulated screws combined with high-strength sutures and Nice knots to replace the Kirschner wire and tension band wiring. In theory, this allows for less soft tissue complications associated with open approach and steel wire. The modified method not only reduced patients’ postoperative pain and soft-tissue stimulating symptoms, but also met the needs of stable fixation and postoperative rehabilitation. In this study, we retrospectively reviewed 48 cases of unilateral closed transverse patellar fracture that had been treated by either closed reduction and internal fixation using cannulated screws combined with high-strength sutures and Nice knots (the CRIF-NK group, n=24 patients), or traditional open reduction and internal fixation using cannulated screws combined with tension band wiring (the ORIF-TBW group, n=24 patients), and compared the intraoperative and early postoperative clinical results of both groups.
We present the following article in accordance with the STROBE reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-22-208/rc).
Methods
Patient enrollment
We enrolled 48 patients with unilateral closed transverse patellar fractures who had been treated by either closed reduction and internal fixation using cannulated screws combined with high-strength sutures and Nice knots (the CRIF-NK group, n=24 patients), or traditional open reduction and internal fixation using cannulated screws combined with tension band wiring (the ORIF-TBW group, n=24 patients) between June 2018 to June 2020 in this study. Patients with unilateral closed transverse patellar fractures were enrolled based on fracture morphology, and only if the following criteria were met: (I) the fracture displacement was >3 mm; (II) the articular step-off was >2 mm; and (III) the fracture morphology was evaluated by X-ray and computed tomography (CT), and confirmed intraoperatively.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Wuxi 9th People’s Hospital (No. LW 2021030). Individual consent for this retrospective analysis was waived. This trial was registered on https://www.chictr.org.cn (registration No. ChiCTR2100054360).
Surgical technique
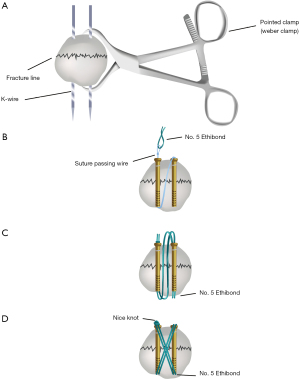
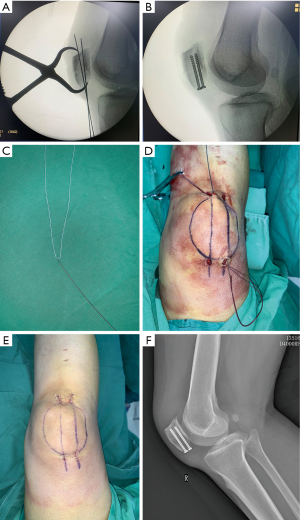
After administering appropriate anesthesia to the patient, a pneumatic tourniquet was used on the lower limb, and routine surgical disinfection and draping were performed. The swelling degree of the knee joint was assessed. If significant swelling was present along with many ecchymoses, or obvious fluctuation in the knee joint, a syringe was used to draw out the fluid. With the knee joint in the extended position, point-reduction forceps were used to reduce the patella, and C-arm fluoroscopy was used to confirm good fracture reduction. With the knee joint in the flexed position, 2 1.2-mm guide pins were drilled parallelly from the distal end to the proximal end close to the articular surface. Fluoroscopy was then used to ensure that the guide pins were located about 5 mm below the patella cartilage and parallel to the articular surface. Next, 4 skin incisions of about 0.5 mm were made at the entrances and exits of the guide pins, and the tissues were separated to expose the surface of the patella. A hollow drill was then used to expand the tunnels along the guide pins. After measuring the length of each tunnel, a cannulated screw of a suitable length of 4.0 mm was selected for insertion in the patella, and the position and length of the cannulated screw were examined under fluoroscopy. In the CRIF-NK group, high-strength sutures composed of No. 5 Ethibond (Ethicon, Somerville, NJ, USA) were passed through the 2 cannulated screws, creating a figure “8” shape via a suture passing wire (Arthrex, Naples, FL, USA). After cutting the loop guide wire at the end of the thread guide, double-stranded Nice knots were used to gradually tighten the high-strength sutures. Due to the loop security provided by the Nice knots, knot slippage was prevented. When the Nice knots were finally tightened, a figure “8” was created (see Figures 1,2). In the ORIF-TBW group, the traditional surgical procedures were performed as described previously (7).
Pre-operative and postoperative management
The operative time from the 1st skin incision to the closure of the wound for each patient was recorded routinely, as was the intraoperative blood loss (mL). X-ray radiographs (anteroposterior and lateral view) at 2 days, 6 weeks, and 3, 6, and 12 months after surgery were obtained. The criteria for fracture healing were an absence of local pain and tenderness, normal walking without help, and evidence of trabecular bone on the fracture line. Both groups started knee functional exercises, including static quadriceps training and straight leg elevation, 1 day after surgery. Active or passive knee joint functional exercises and tolerable partial-weight training with support from an adjustable brace were started 2 days after surgery and continued under the guidance of a physiotherapist for 3 weeks. The knee flexion and extension range reached or exceeded 90° within 2–3 weeks of the operation, and all patients were able to walk at the 6-week follow-up. The knee function was assessed using Böstman scale (8), and the degree of pain was quantified by the Visual Analogue Scale (VAS) (9). As described previously (10), the clinical grading scale of Böstman includes a range of movement (3–6 points), pain (0–6 points), work (0–4 points), atrophy (0–4 points), assistance in walking (0–4 points), effusion (0–2 points), giving way (0–2 points), and stair-climbing (0–2 points).
Statistical analysis
SPSS version 24.0 (SPSS, Inc., Chicago, IL, USA) was used to analyze the data. The results are expressed as the mean ± standard deviation. The repeated measurement ANOVA was used for comparisons between two groups, and a two-sided P value <0.05 was considered statistically significant.
Results
All patients underwent surgical treatment within 48 hours of admission, and were discharged within 3–5 days of surgery. For both groups, the fracture union rate was 100%, and the functional recovery of the limb was satisfactory at the last follow-up.
As Table 1 shows, the operative time did not differ significantly between the CRIF-NK group (48.75±2.38 min) and the ORIF-TBW group (48.46±1.86 min; P>0.05), but the intraoperative blood loss of the CRIF-NK group (35.21±6.16 mL) was significantly less than that of the ORIF-TBW group (75.42±7.92 mL; P<0.001). The results above indicate that the CRIF-NK technique caused less operative trauma than the ORIF-TBW technique, which could be beneficial to the early recovery of patients.
Table 1
| Variables | CRIF-NK group (n=24) | ORIF-TBW group (n=24) | P |
|---|---|---|---|
| Operative time (min) | 48.75±2.38 | 48.46±1.86 | 0.639 |
| Intraoperative blood loss (mL) | 35.21±6.16 | 75.42±7.92 | <0.001 |
| VAS (4 weeks) | 3.52±0.42 | 5.16±0.68 | <0.001 |
| VAS (8 weeks) | 1.47±0.40 | 3.14±0.72 | <0.001 |
| Böstman scale (8 weeks) | 28.13±0.94 | 26.33±1.00 | <0.001 |
| Böstman scale (1 year) | 29.00±0.88 | 29.17±0.96 | 0.535 |
| Fracture healing time (weeks) | 11.92±0.83 | 12.04±0.69 | 0.573 |
CRIF-NK, cannulated screws combined with high-strength sutures and Nice knots; ORIF-TBW, open reduction and internal fixation using cannulated screws and tension band wiring; VAS, Visual Analog Scale.
The average follow up was 21.9 months (range, 16–29 months) with all patients followed to clinical and radiographic union. The mean VAS scores at 4 and 8 weeks and the mean Böstman scale score at 8 weeks after surgery were significantly better in the CRIF-NK group (3.52±0.42, 1.47±0.40 and 28.13±0.94, respectively) than the ORIF-TBW group (5.16±0.68, 3.14±0.72 and 26.33±1.00, respectively; all P<0.001). No significant differences were observed in the mean Böstman scale scores at the 1-year follow-up, or the fracture healing time between the CRIF-NK group (29.00±0.88 and 11.92±0.83 weeks, respectively) and the ORIF-TBW group (29.17±0.96 and 12.04±0.69 weeks, respectively; P>0.05). Additionally, only 1 patient (1/24) in the CRIF-NK group required internal fixation removal, but all patients (24/24) in the ORIF-TBW group required internal fixation removal.
Discussion
The Kirschner wire combined with tension band wiring is a widely used surgical method for the treatment of patellar fractures in clinical settings (11). In the surgical treatment of patella fractures, many orthopedists have reported that internal fixation, especially with a Kirschner wire and steel wire, stimulates the thin prepatellar soft tissue, resulting in varying degrees of pain or joint discomfort, and thereby affecting knee function (12). Additionally, many patients must undergo a 2nd operation due to soft-tissue stimulating symptoms, which further increases the suffering and treatment costs of patients (13,14). Further, the implantation of the steel wire makes it impossible for patients to undergo MRI examinations, which can affect the diagnosis and treatment of other diseases. To address these disadvantages, many improvements have been made. For example, Liu et al. (7) used cannulated screws to replace the Kirschner wire in the treatment of patellar fracture and achieved good clinical outcomes. Cannulated screws effectively avoid the disadvantages of the Kirschner wire, including needle withdrawal and deformation, but cannot prevent the soft-tissue stimulating symptoms caused by a steel wire. Thus, metal-free techniques have been applied in the surgical treatment of patella fractures.
McGreal et al. (15) demonstrated that the mechanical properties of a braided polyester suture (No. 5, Ticron) are equivalent to those of steel wire when applied as a tension band for the internal fixation of the fractured patella. Additionally, Chen et al. (16) found that No. 5 Ticron sutures were effective and safe in the fixation of a fractured patella, and had a lower complication rate than that of steel wire. On the basis of these studies, we improved the surgical treatment by using cannulated screws and high-strength sutures to replace the Kirschner wire and tension band wiring in the CRIF-NK group. The modified method not only reduced patients’ postoperative pain and soft-tissue stimulating symptoms, but also met the needs of stable fixation and postoperative rehabilitation. Additionally, the improved method greatly decreased the 2nd operation rate. Indeed, in the CRIF-NK group, only 1 patient (1/24) requested the removal of the cannulated screws for reasons related to personal faith. Conversely, in the CRIF-NK group, all patients (24/24) requested the removal of the tension band wiring due to a dull pain in the knee joint with significant weather changes, and the possibility that MRI examinations may need to be performed in the future.
The Nice knot is a novel type of double-stranded knot that has many advantages, including those related to its adjustability, strength, versatility, and simplicity (17). The Nice knot exerts little shear force on the patella, and the characteristic of loop security prevents knot slippage, allowing surgeons to stop and resume the tightening process at any stage (18). Finally, the Nice knot achieves the best positioning and reduction (18). Chen et al. (10) applied the Nice knot as an auxiliary reduction technique in the treatment of patellar fractures, and found that the sliding and self-stabilizing Nice knot reduced operative time and intraoperative blood loss, stabilized the fixation, and achieved satisfactory postoperative outcomes. In the present study, we used high-strength sutures with Nice knots to achieve auxiliary reduction and fix the transverse patella fractures in the CRIF-NK group, which significantly reduced the reduction time, and did not extend the operative time for the minimally invasive fixation of the patella. Further, the modified method created a stable, non-stimulating, and safe knot.
Minimally invasive closed reduction and internal fixation are development trends in modern surgery, and have been proven to be associated with earlier exercise and rehabilitation, higher knee function scores, fewer joint adhesions or stiffness, and a lower incidence of wound complications in the management of fractures around the knee joint (19,20). Chiang et al. (21) compared the minimally invasive technique with traditional open tension band wiring in the treatment of displaced transverse patellar fractures, and found that the minimally invasive technique was a reproducibly reliable method that offered better clinical outcomes, and had lower incidence rates of reoperation and complications. In the present study, the minimally invasive closed reduction and internal fixation technique was used in the CRIF-NK group, and did not require extensive incisions of the soft tissues or the splitting of ligaments, which in turn led to less tissue damage and intraoperative blood loss. Additionally, the minimally invasive treatment method resulted in no soft-tissue stimulating complications postoperatively, and did not require internal fixation removal. Thus, we are of the view that the improvements described above contributed to the better clinical outcomes in the CRIF-NK group compared to the ORIF-TBW group.
In conclusion, this study reported the intraoperative and early postoperative clinical results of the closed reduction and internal fixation of transverse patellar fractures using cannulated screws combined with high-strength sutures and Nice knots. Compared to the method of traditional open reduction and internal fixation of transverse patellar fractures using cannulated screws combined with tension band wiring, our improved treatment method reduced intraoperative blood loss, tissue damage, and soft-tissue stimulating complications, which are beneficial to the early functional recovery of the knee joint postoperatively. Additionally, the method eliminates the need to remove the tension band wiring and internal fixation, and thus greatly decreases the medical burden placed on patients. Thus, we conclude that the percutaneous minimally invasive treatment of a transverse patellar fracture using cannulated screws combined with high-strength sutures and Nice knots produces good clinical outcomes and is worthy of clinical application.
There were several limitations in the present study. First, this was a retrospective study of a novel technique, and biases from authors may have affected the results. Next, the average follow-up period of 21.9 months may be not long enough to supporting definitive conclusions. Furthermore, only 24 patients for each group were included into this retrospective clinical study with limited statistical value due to the small patient population.
Acknowledgments
Funding: This study was funded by the Wuxi Top Medical Expert Team of “Taihu Talent Program” (No. TTPJY202101).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-208/rc
Data Sharing Statement: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-208/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-208/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Wuxi 9th People’s Hospital (No. LW 2021030). Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sayum Filho J, Lenza M, Tamaoki MJ, et al. Interventions for treating fractures of the patella in adults. Cochrane Database Syst Rev 2021;2:CD009651. [PubMed]
- Henrichsen JL, Wilhem SK, Siljander MP, et al. Treatment of Patella Fractures. Orthopedics 2018;41:e747-55. [Crossref] [PubMed]
- Steinmetz S, Brügger A, Chauveau J, et al. Practical guidelines for the treatment of patellar fractures in adults. Swiss Med Wkly 2020;150:w20165. [Crossref] [PubMed]
- Kakazu R, Archdeacon MT. Surgical Management of Patellar Fractures. Orthop Clin North Am 2016;47:77-83. [Crossref] [PubMed]
- Malik M, Halwai MA. Open reduction and internal fixation of patellar fractures with tension band wiring through cannulated screws. J Knee Surg 2014;27:377-82. [Crossref] [PubMed]
- Hoshino CM, Tran W, Tiberi JV, et al. Complications following tension-band fixation of patellar fractures with cannulated screws compared with Kirschner wires. J Bone Joint Surg Am 2013;95:653-9. [Crossref] [PubMed]
- Liu C, Ren H, Wan C, et al. Comparison of the Therapeutic Effects of Tension Band with Cannulated Screw and Tension Band with Kirschner Wire on Patella Fracture. Comput Math Methods Med 2020;2020:4065978. [Crossref] [PubMed]
- Böstman O, Kiviluoto O, Nirhamo J. Comminuted displaced fractures of the patella. Injury 1981;13:196-202. [Crossref] [PubMed]
- Hayes MHS, Paterson DG. Experimental development of the graphic rating method. Psychol Bull 1921;18:98-9.
- Chen M, Jin X, Fryhofer GW, et al. The application of the Nice knots as an auxiliary reduction technique in displaced comminuted patellar fractures. Injury 2020;51:466-72. [Crossref] [PubMed]
- Tian Y, Zhou F, Ji H, et al. Cannulated screw and cable are superior to modified tension band in the treatment of transverse patella fractures. Clin Orthop Relat Res 2011;469:3429-35. [Crossref] [PubMed]
- Wang Y, Xia D, Luo X, et al. Comparison of the Kirschner Wire Tension Band with a Novel Nickel-Titanium Arched Shape-Memory Alloy Connector in Transverse Patellar Fractures: A Retrospective Study. J Knee Surg 2021;34:987-96. [Crossref] [PubMed]
- Zhu XZ, Huang TL, Zhu HY, et al. A retrospective cohort study on prevalence of postoperative complications in comminuted patellar fractures: comparisons among stabilized with Cannulated-Screw, Kirschner-Wire, or Ring-Pin Tension Bands. BMC Musculoskelet Disord 2021;22:60. [Crossref] [PubMed]
- Lin T, Liu J, Xiao B, et al. Comparison of the outcomes of cannulated screws vs. modified tension band wiring fixation techniques in the management of mildly displaced patellar fractures. BMC Musculoskelet Disord 2015;16:282. [Crossref] [PubMed]
- McGreal G, Reidy D, Joy A, et al. The biomechanical evaluation of polyester as a tension band for the internal fixation of patellar fractures. J Med Eng Technol 1999;23:53-6. [Crossref] [PubMed]
- Chen CH, Huang HY, Wu T, et al. Transosseous suturing of patellar fractures with braided polyester - a prospective cohort with a matched historical control study. Injury 2013;44:1309-13. [Crossref] [PubMed]
- Boileau P, Alami G, Rumian A, et al. The Doubled-Suture Nice Knot. Orthopedics 2017;40:e382-6. [Crossref] [PubMed]
- Lee HJ, Kim BK, Ryu HS, et al. Vertical Interfragmentary Doubled Suture for Displaced Patella Fractures: Sequential Compressive Tightening with Nice Knot. Clin Orthop Surg 2020;12:413-6. [Crossref] [PubMed]
- Vicenti G, Bizzoca D, Nappi VM, et al. Minimally invasive osteosynthesis technique in the treatment of transverse patellar fractures in the elderly. Injury 2020;51:S50-5. [Crossref] [PubMed]
- Shao J, Wang J, Chen Y, et al. Comparison of a minimally invasive surgical technique with open surgery for transverse patella fractures. Exp Ther Med 2019;18:4203-8. [Crossref] [PubMed]
- Chiang CC, Chen WM, Jeff Lin CF, et al. Comparison of a minimally invasive technique with open tension band wiring for displaced transverse patellar fractures. J Chin Med Assoc 2011;74:316-21. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)


