
Efficacy of ultrasound-guided erector spinae plane block versus paravertebral block for postoperative analgesia in single-port video-assisted thoracoscopic surgery: a retrospective study
Introduction
Most of the surgical procedures requiring thoracotomy can be performed with video-assisted thoracoscopic surgery (VATS). A thoracoscopic method is frequently used in the surgical treatment of pneumothorax for prolonged air leak and recurrence. Compared with conventional thoracoscopic surgery, single-port VATS uses a single incision. Therefore, patients may have less pain and better respiratory function after surgery. Studies have shown that, uniportal VATS has advantages in terms of less pain, complication rate and length of hospital stay (LOS) compared to open surgery and multiport thoracoscopic techniques (1,2).
After the widespread use of ultrasound (US), new regional anesthesia techniques on the trunk are used as an analgesic method in thoracic surgery and are called truncal blocks (3). In VATS, thoracic paravertebral block (TPVB) is a successful method of providing postoperative analgesia and is recommended by the enhanced recovery after surgery (ERAS) protocol (4). Although the risk of complications is minimized with the use of US, it requires advanced experience owing to its proximity to the pleura, epidural, and subarachnoid distance (5,6). Considering its advantages in the postoperative period, less invasive, easier and safer applicable plane blocks may be sufficient for analgesia after uniportal VATS. The erector spinae plane block (ESPB) is a new technique that is easier to visualize and perform because it is more superficial. Owing to these advantages, it has been preferred frequently for postoperative analgesia in different types of operations such as thorax, abdomen, hip, and lumbar surgeries in recent years (7-10).
To the best of our knowledge, there is no study in the literature where a single-injection of ESPB and TPVB has been performed for postoperative analgesia in uniportal VATS. In this study, it was aimed to compare the analgesic effects of ESPB and TPVB, which were performed as a single injection in uniportal VATS. We present the following article in accordance with the STROBE reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-22-75/rc).
Methods
Study design and patient selection
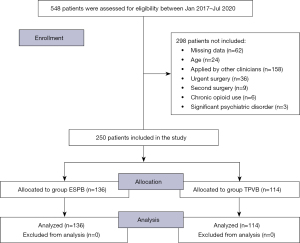
A total of 548 patients who underwent wedge resection by uniportal VATS technique under general anesthesia with a diagnosis of prolonged pneumothorax between Jan 2017 and Jul 2021 were retrospectively analyzed. TPVB was performed to all patients until Dec 2018 who underwent VATS, and then ESPB was applied for the purpose of clinical experience, although different opinions were presented about its effectiveness. In the retrospective review, patients who were made performed block by a single clinician to provide a standard and homogeneous group comparison were included in the study. The selection included the patients who met the criteria and applied consecutively. In this study, the authors included 114 patients who had TPVB application between Jan 2017 and Dec 2018 and 136 patients who had ESPB application between Jan 2019 and Jul 2021. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of the Bakırköy Dr. Sadi Konuk Training and Research Hospital (No. 2021-20-27/2019-250) and individual consent for this retrospective analysis was waived.
The demographic and clinical data of patients were obtained from the corporate computer-based documentation system. Patients aged between 18–70 years, having body mass index (BMI) <35 kg/m2, being in the American Society of Anesthesiologist (ASA) physical status classification of I–III, and underwent uniportal VATS were evaluated within the scope of this study. Patients first having uniportal VATS and later undergoing thoracotomy during the operation, with a serious psychiatric history, chronic pain or chronic opioid use (at least 3 months) and who underwent second surgery or emergency surgery were excluded from the study. A total of 250 patients were included in the study (Figure 1).
The patients were known to the anesthesiologist since all the applied blocks were performed by a single clinician. However, the practitioners on duty at the statistical and writing stage did not know which patients belonged to which group. Likewise, anesthesia nurses who were tasked with evaluating the results such as postoperative pain severity were independent from the study and were blinded by the block type which was performed. In addition, independent from the study, each patient was informed about the procedure to be done and their consent was obtained.
General anesthesia and truncal blocks technique
In our clinic, a standard anesthesia protocol is applied in all patients. Electrocardiography, non-invasive blood pressure and peripheral oxygen saturation monitorizations were performed as a standard. Midazolam (0.03–0.05 mg/kg) was administered intravenously (IV) as premedication, and isotonic saline infusion (8 mL/kg/h) was initiated by inserting a 22-gauge venous line. After the required asepsis conditions in the block area were met, while the patient was in the sitting position, by using US (Esaote MyLabSeven/Esaote S.p.A, Genoa, Italy) a linear multifrequency 12 L probe and a 20-gauge 100 mm peripheral nerve block needle (Stimupleks Ultra 360 30°—BRA-04892510-01/B. Braun Melsungen AG, Hessen, Germany), the one-sided truncal block was performed.
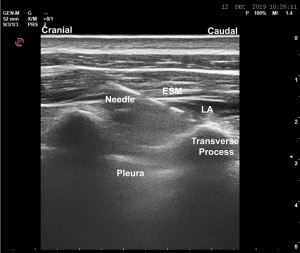
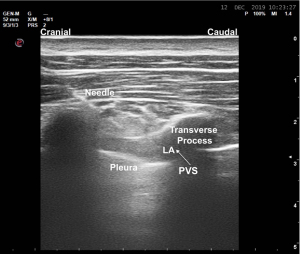
The transverse process was visualized by placing the probe approximately 3 cm lateral to the spinous process of the T5 vertebrae for ESPB. When the needle was advanced in the cranio-caudal direction with an angle of 30–40° and touched the transverse process, the presence of blood and/or air was checked by aspiration. Hydro-dissection was performed with 2–3 mL isotonic saline and 20 mL 0.25% bupivacaine (Marcaine 0.5%, 5 mg/mL) was injected by observing that the erector spinae muscle (ESM) was separated from the transverse process (Figure 2). In the TPVB procedure, the probe was placed in the paramedian sagittal plane immediately lateral to the T5 vertebra spinous process, and the needle was advanced in-plane in the cranio-caudal direction at an angle of 30–40°. After passing the existing muscle groups on this plane, it was entered under the superior costotransverse ligament. Hydro dissection was performed with 2–3 mL of isotonic saline, and the pleura were pushed down, then 20 mL of 0.25% bupivacaine was injected (Figure 3).
Standard anesthesia induction after truncal block was performed with propofol (2–3 mg/kg), fentanyl (1–2 µg/kg) and rocuronium (0.6–0.8 mg/kg). Anesthesia was maintained with sevoflurane (0.7 MAC) and IV remifentanil infusion (0.05–0.1 µg/kg/min). At the end of the surgery, 8 mg ondansetron as prophylactic antiemetic and 1 g paracetamol and 100 mg tramadol hydrochloride IV were given. After the operation, the patients were transferred to post-anesthesia care unit (PACU) for close hemodynamic follow-up for the first 24 hours. The evaluation of postoperative pain and opioid consumption was performed by an anesthesiologist independent of the work in the PACU team.
Surgical procedures
In our bullectomy operations with single-port VATS, a 2.5 cm incision was made at the level of the 5th intercostal space in the median axillary line, after entering the thorax with a 10 mm 30° video thoracoscope, the thoracoport was retracted and two rotary instruments (Roticulator Endograsp and EndoGIA Universal, Covidien Ilc, Mansfield, MA, USA) was placed. Tube thoracostomy incisions made from the 5th intercostal space were used in the emergency department, which was enlarged for the uniportal incision, and the thorax was entered with finger dissection, taking into account the lung adhesions that may occur in these incisions. By removing the thoracoport, excessive pressure on the intercostal neurovascular bundle that could cause chronic pain was avoided. Usually two endostapes were placed and wedge resection was performed. A standard pleurectomy was performed using endoscopic kitner dissectors and a curved ovarian clamp. A 32 Fr thorax drain was placed through the same incision and underwater drainage was taken.
Pain management
Standard postoperative analgesia was performed using a patient-controlled analgesia (PCA) device (CADD-Legacy PCA Ambulatory Infusion Pump, Model 6300/Smiths Medical, Dublin, OH, USA) using IV morphine infusion. Morphine solution (0.5 mg/mL) prepared in 100 mL isotonic saline; and the PCA was adjusted as 1 mg bolus, lockout interval of 10 minutes, 1-hour limit dose 4 mg, and no basal infusion. All patients’ 1st-6th-12th-24th hour numerical rating scale (NRS) scores were examined in the pain follow-up form. For rescue analgesia, patients received a non-steroidal anti-inflammatory agent in two doses of IV ibuprofen 800 mg per day for a total of 1,600 mg. Morphine consumption was evaluated in terms of bolus number and converted as milligrams.
Outcome measurements
The primary outcome measure was postoperative cumulative morphine consumption in the first 24 hours. The secondary outcome measures were the NRS scores at rest (static) and while coughing (dynamic) examined at four different time periods (1st, 6th, 12th, and 24th hours). Furthermore, these measures, intraoperative opioid requirement, postoperative rescue analgesic requirement, perioperative complications including bradycardia, nausea and vomiting, postoperative pulmonary complications as atelectasis, effusion and pneumonia were also evaluated.
Statistical analysis
The G*Power 3.1.9.2 programme was used to calculate the sample size of the study. A pilot retrospective study was conducted with twenty patients from each group to determine the minimal sample size for the primary outcome. The mean morphine consumption was 19.25±8.75 in the group ESPB and 14.47±6.22 in the group TPVB. An effect size 0.546 and α error =0.05 with a power of 95% was assumed so that each group had at least 93 participants. We included 136 patients in group ESPB and 114 patients in group TPVB due to the possibility of dropouts. Patient data from the pilot study were not included in the main study.
The data obtained from the research were analyzed with SPSS 22.00 program. Mean, standard deviation (SD), median, lowest highest, frequency, and ratio values were used in descriptive statistics of the data. The distribution of variables was measured by the Kolmogorov Simonov test. Independent sample t-test and Mann-Whitney U test were used for the analysis of quantitative independent data. The chi-square test was used for the analysis of qualitative independent data, and the Fischer test was used when the chi-square test conditions were not met. P<0.05 was accepted for the significance level.
Results
Among participants, 84.8% were male and the mean age was 32.4 years. The ASA score and the other descriptive variables of the patients in the two groups were not different (Table 1). There was no significant difference between the groups in the intraoperative remifentanil consumption (P=0.251). There was no statistically significant difference in terms of hemodynamic parameters in the intraoperative period of the patients (Table 2). Although the incidence of opioid-related side effects in the postoperative period was higher in the ESPB group with a significantly higher morphine consumption, no statistically significant difference was found between the groups. The number of PCA button presses (demand dose) was significantly higher in the ESPB group, regardless of the lockout interval (P<0.001) (Table 3).
Table 1
| Characteristics | ESPB group (n=136) | TPVB group (n=114) | P value |
|---|---|---|---|
| Age | 33.93±11.51 | 30.14±8.1 | 0.151 |
| Gender | 0.740 | ||
| Female | 22 (16.2%) | 16 (14.03%) | |
| Male | 114 (83.8%) | 98 (86.9%) | |
| Height | 175.04±7.65 | 174.54±6.81 | 0.718 |
| Weight | 65.17±6.11 | 64.85±9.77 | 0.832 |
| BMI | 21.39±2.24 | 20.99±2.73 | 0.379 |
| ASA | 0.965 | ||
| I | 24 (17.6%) | 22 (19.3%) | |
| II | 104 (76.5%) | 86 (75.4%) | |
| III | 8 (5.9%) | 6 (5.3%) |
Data are presented as mean ± SD or number (%). ESPB, erector spinae plane block; TPVB, thoracic paravertebral block; BMI, body mass index; ASA, American Society of Anesthesiologists; SD, standard deviation.
Table 2
| Item | ESPB group (n=136) | TPVB group (n=114) | P value |
|---|---|---|---|
| Duration of anesthesia (min) | 127.94±46.14 | 117.94±35.39 | 0.169 |
| Duration of surgery (min) | 96.89±45.76 | 94.28±33.18 | 0.927 |
| Mean remifentanil use (μg/kg/min) | 0.044±0.276 | 0.041±0.030 | 0.251 |
| Intraoperative complications | |||
| Bradycardia | 8 (5.9%) | 8 (7.0%) | 0.796 |
| Tachycardia | 18 (13.2%) | 22 (19.3%) | 0.357 |
| Hypotension | 68 (50.0%) | 74 (64.9%) | 0.094 |
| Hypertension | 14 (10.3%) | 18 (15.8%) | 0.360 |
| Postoperative complications | |||
| Hematoma | 4 (2.9%) | 4 (3.5%) | 0.857 |
| PONV | 24 (17.6%) | 16 (14.0%) | 0.583 |
| Pruritus | 4 (2.9%) | 2 (1.8%) | 0.666 |
| PPC | 18 (13.2%) | 12 (10.5%) | 0.643 |
| Chest tube removal (day) | 4.31±2.77 | 4.42±2.16 | 0.649 |
| LOS (day) | |||
| PACU | 1 (100.0%) | 1 (100.0%) | 1.000 |
| Ward | 5.44±2.26 | 5.38±2.02 | 0.867 |
Data are presented as mean ± SD or number (%). ESPB, erector spinae plane block; TPVB, thoracic paravertebral block; PONV, postoperative nausea and vomiting; PPC, postoperative pulmonary complication; LOS, length of hospital stay; PACU, post-anesthesia care unit; SD, standard deviation.
Table 3
| Item | ESPB group (n=136) | TPVB group (n=114) | P value |
|---|---|---|---|
| PCA demand dose | 36.64±26.9 | 18.82±13.67 | <0.001* |
| PCA delivered dose | |||
| PO 0–1st h | 3.17±1.34 | 2.01±1.12 | 0.863 |
| PO 0–6th h | 8.76±4.92 | 4.02±1.78 | 0.006* |
| PO 0–12th h | 16.69±8.56 | 9.65±5.49 | <0.001* |
| PO 0–24th h | 20.06±9.98 | 11.35±7.08 | <0.001* |
| Rescue analgesia requirement | 24 (17.6%) | 22 (19.3%) | 0.812 |
| S-NRS | |||
| PO 1st h | 3 [0–7] | 3 [0–7] | 0.783 |
| PO 6th h | 2 [0–5] | 2 [0–5] | 0.059 |
| PO 12th h | 2 [0–6] | 3 [0–6] | 0.350 |
| PO 24th h | 3 [0–5] | 2 [0–4] | 0.008* |
| D-NRS | |||
| PO 1st h | 3 [1–5] | 3 [0–8] | 0.346 |
| PO 6th h | 4 [1–7] | 3 [1–7] | 0.003* |
| PO 12th h | 4 [1–7] | 3 [0–7] | 0.514 |
| PO 24th h | 4 [1–8] | 3 [0–7] | 0.034* |
Data are presented as mean ± SD, median (IQR) or number (%). *, P<0.05. ESPB, erector spinae plane block; TPVB, thoracic paravertebral block; PCA, patient-controlled analgesia; PO, postoperative; h, hour; S-NRS, static numerical rating scale; D-NRS, dynamic numerical rating scale; SD, standard deviation.
Similarly, cumulative morphine consumption in the postoperative 12th and 24th hours was significantly higher in the ESPB group (P<0.001 and P<0.001, respectively). Static NRS scores were lower in the TPVB group at 24th hour (P=0.008). In addition, NRS scores at rest were lower than four in both block groups (Table 3). Dynamic NRS scores were significantly lower in the TPVB group at postoperative 6th and 24th hours (P=0.003 and P=0.034, respectively).
When the intragroup values were compared using the repeated measurement test, there was no significant difference in dynamic NRS scores in the TPVB group as time from the 1st hour to the 24th hour (Table 3). Both groups were found to be similar to each other in terms of the LOS (PACU and ward) of the patients (P=1.000 and P=0.867, respectively).
Discussion
For VATS, which is considered a minimally invasive surgical approach, TPVB is now accepted as a first-line local site technique rather than thoracic epidural analgesia (TEA) (4). Although other truncal blocks have become widespread as postoperative analgesia techniques, less invasive methods alternative to TPVB have been reported in VATS (5,11,12). ESPB is a new and up-to-date method, and when compared with TPVB, there are not enough studies in the literature in VATS (5,12).
Unlike in uniportal VATS, the incision is limited to an intercostal space. The length and number of incisions are less than that of the conventional approach of VATS. Therefore, anatomical structures such as muscles, nerves, and blood vessels are exposed to less trauma and clinically less postoperative pain is provided (13-15). This study was conducted to compare the postoperative analgesic efficacy of single-injection TPVB and ESPB in uniportal VATS. The most important finding of the present study is that TPVB provides superior postoperative analgesia and less opioid consumption than ESPB with a single level and single-injection in uniportal thoracoscopic surgery. Since morphine consumption is considered as an indicator in the evaluation of analgesic efficacy, morphine consumption was evaluated in our study. It was noted that morphine consumption was significantly lower in the TPVB group in the first 24 hours postoperatively. Morphine consumption in the first hour was similar between the two groups. It may depend on the analgesia which was applied at the end of surgery. Morphine consumption was higher in the ESPB group in all periods after 1st hour; however static NRS values did not show any statistically significant difference between the two groups except for the 24th hour. These results may be related to two reasons. Firstly, it was probable that intense morphine consumption used in the ESPB group could be effective when NRS scores were examined. Secondly, ESPB has a better effect on moderate pain during resting but is insufficient in severe pain caused by physical activity such as coughing. Because, when the dynamic NRS values were examined, it was found to be significantly higher in the ESPB group at 6th and 24th hours.
Similarly, another study found that morphine consumption and VAS scores were lower in the TPVB group (5). However, in the presented study, it is important to obtain similar results with the single-level application of TPVB. The objectivity and consistency of the results of this study are higher since both blocks were performed from a single level and a more homogenous group was evaluated. In uniportal thoracoscopy, the authors determined the effective level and obtained similar results with single point TPVB, so the authors do not recommend multiple injections at least in single-port VATS.
In the cadaver study comparing the TPVB and ESPB spread, it was reported that the spread in the ESPB to the thoracic paravertebral area was inconsistent and that there was no spread to the epidural area, therefore ESPB could not be equivalent to single and multiple injections of TPVB (16). Recently, Lonnqvist et al. (17) reported that there was insufficient evidence for the spread of local anesthesia in ESPB and that the anterior part of the intercostal nerve was not reliably affected, so it could not create analgesia in the anterior part of the trunk. In the presented study, it was found that ESPB could not provide as analgesic efficacy as TPVB even in this type of surgery associated with less surgical trauma.
In previous studies, it is noteworthy that different results have appeared due to the differences in the positions of the patients during the block technique (6,12). In a recent review, it has been reported that when performing ESPB, the patient’s position may affect the spread of local anesthesia and therefore the effect and quality of the block. Still, no studies are investigating this effect (18). The primary purpose of the study is not to investigate the relationship between the position of the patient and the analgesic effect of the block, but there are different application techniques in the literature. In this study, both blocks were applied in the sitting position. Therefore, since the conditions valid for the distribution of local anesthetic (LA) are the same for TPVB, it cannot be considered to affect the study results.
The authors have some limitations in the present study. Firstly, it was retrospective, based on a single center’s experience. Secondly, it had not a control group where both blocks were not applied. Moreover, after additional procedures, the authors could not evaluate the dermatome area affected by the block in every patient owing to temporal limitations. However, this study will contribute significantly to the literature since there are a limited number of studies in thoracoscopic surgery.
Conclusions
The present study shows that TPVB is still a superior analgesic method in thoracoscopic surgery. ESPB could not provide as adequate analgesia as TPVB in this type of surgery, associated with less surgical trauma. However, our data should be confirmed by prospective and larger sampled, multi-centric randomized controlled trials.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-75/rc
Data Sharing Statement: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-75/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-75/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of the Bakırköy Dr. Sadi Konuk Training and Research Hospital (No. 2021-20-27/2019-250) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Soultanis KM, Gonzalez-Rivas D. Devising the guidelines: the concept of uniportal video-assisted thoracoscopic surgery-incisions and anesthetic management. J Thorac Dis 2019;11:S2053-61. [Crossref] [PubMed]
- Hirai K, Usuda J. Uniportal video-assisted thoracic surgery reduced the occurrence of post-thoracotomy pain syndrome after lobectomy for lung cancer. J Thorac Dis 2019;11:3896-902. [Crossref] [PubMed]
- Sari S, Kumar J, Turan A. New peripheral nerve blocks and local anesthetics. Curr Opin Crit Care 2021;27:733-42. [Crossref] [PubMed]
- Piccioni F, Ragazzi R. Anesthesia and analgesia: how does the role of anesthetists changes in the ERAS program for VATS lobectomy. J Vis Surg 2018;4:9. [Crossref] [PubMed]
- Chen N, Qiao Q, Chen R, et al. The effect of ultrasound-guided intercostal nerve block, single-injection erector spinae plane block and multiple-injection paravertebral block on postoperative analgesia in thoracoscopic surgery: A randomized, double-blinded, clinical trial. J Clin Anesth 2020;59:106-11. [Crossref] [PubMed]
- Gürkan Y, Aksu C, Kuş A, et al. Erector spinae plane block and thoracic paravertebral block for breast surgery compared to IV-morphine: A randomized controlled trial. J Clin Anesth 2020;59:84-8. [Crossref] [PubMed]
- Hacıbeyoğlu G, Topal A, Küçükkartallar T, et al. Investigation of the effect of ultrasonography-guided bilateral erector spinae plane block on postoperative opioid consumption and pain scores in patients undergoing hepatectomy: a prospective, randomized, controlled study. Sao Paulo Med J 2022;140:144-52. [Crossref] [PubMed]
- Tulgar S, Kapakli MS, Senturk O, et al. Evaluation of ultrasound-guided erector spinae plane block for postoperative analgesia in laparoscopic cholecystectomy: A prospective, randomized, controlled clinical trial. J Clin Anesth 2018;49:101-6. [Crossref] [PubMed]
- Pişkin Ö, Gökçe M, Altınsoy B, et al. Effects of continuous erector spinae plane block on postoperative pain in video-assisted thoracoscopic surgery: a randomized controlled study. Gen Thorac Cardiovasc Surg 2022;70:64-71. [Crossref] [PubMed]
- Ahiskalioglu A, Tulgar S, Celik M, et al. Lumbar Erector Spinae Plane Block as a Main Anesthetic Method for Hip Surgery in High Risk Elderly Patients: Initial Experience with a Magnetic Resonance Imaging. Eurasian J Med 2020;52:16-20. [Crossref] [PubMed]
- Zhao H, Xin L, Feng Y. The effect of preoperative erector spinae plane vs. paravertebral blocks on patient-controlled oxycodone consumption after video-assisted thoracic surgery: A prospective randomized, blinded, non-inferiority study. J Clin Anesth 2020;62:109737. [Crossref] [PubMed]
- Taketa Y, Irisawa Y, Fujitani T. Comparison of ultrasound-guided erector spinae plane block and thoracic paravertebral block for postoperative analgesia after video-assisted thoracic surgery: a randomized controlled non-inferiority clinical trial. Reg Anesth Pain Med 2019; Epub ahead of print. [Crossref] [PubMed]
- Wang Q, Wei S, Li S, et al. Comparison of the analgesic effect of ultrasound-guided paravertebral block and ultrasound-guided retrolaminar block in Uniportal video-assisted Thoracoscopic surgery: a prospective, randomized study. BMC Cancer 2021;21:1229. [Crossref] [PubMed]
- Ojanguren A, Gonzalez M. What is the optimal way to succeed in uniportal VATS? J Thorac Dis 2020;12:3018-21. [Crossref] [PubMed]
- Matsuura N, Igai H, Ohsawa F, et al. Uniport vs. multiport video-assisted thoracoscopic surgery for anatomical lung resection-which is less invasive? J Thorac Dis 2021;13:244-51. [Crossref] [PubMed]
- Nielsen MV, Moriggl B, Hoermann R, et al. Are single-injection erector spinae plane block and multiple-injection costotransverse block equivalent to thoracic paravertebral block? Acta Anaesthesiol Scand 2019;63:1231-8. [Crossref] [PubMed]
- Lonnqvist PA, Karmakar MK, Richardson J, et al. Daring discourse: should the ESP block be renamed RIP II block? Reg Anesth Pain Med 2021;46:57-60. [Crossref] [PubMed]
- Tulgar S, Ahiskalioglu A, De Cassai A, et al. Efficacy of bilateral erector spinae plane block in the management of pain: current insights. J Pain Res 2019;12:2597-613. [Crossref] [PubMed]
(English Language Editor: D. Chapman)


