Analysis of daily goal sheets on physician-nurse collaboration attitude
Introduction
Inter-professional collaboration is critical to optimize patient care and outcomes. Teamwork and collaboration between physicians and nurses are foundational components of professionalism, as they have been closely linked to improvements of health outcomes and quality of patient care (1,2). Benefits of positive inter-professional collaboration include reduction of the mortality rate in in-patient settings (3), increase of job satisfaction (4), improved maintenance of patient safety (5), and lowered health care costs (6).
Inter-professional collaboration is defined as “when multiple health workers from different professional backgrounds work together with patients, families, carers (caregivers), and communities to deliver the highest quality of care” (7). It is based on the concept that when providers consider each other’s perspective, in addition to that of the patient, they can deliver better care.
Modern intensive care requires a sophisticated, well-coordinated delivery system consisting of both advanced technology and a well-integrated, and highly skilled team. Although significant advances have improved the care and outcomes of many critically ill patients, the complexity and stress of the intensive care unit (ICU) setting nonetheless predispose these units to considerable medical error, which can be of grave consequence. In fact, failure to implement the best evidence-based interventions in the ICU has been estimated to cause 160,000 avoidable deaths each year in the United States (8). Research has found that the implementation of interventions, including the use of checklists during daily multidisciplinary rounds and clinician prompting, is able to reduce mortality and improve other relevant outcomes for patients (9).
Checklists have been successfully employed in aviation and the manufacturing industry to avoid critical omissions during complex procedures (10), and they have also been successfully used in health care. Notable examples are the World Health Organization Checklist for Safe Surgery (11) and the Keystone ICU Project checklist to prevent central line-associated bloodstream infections (12). In select centers, checklists have also been used during daily multidisciplinary ICU rounds to avoid errors of omission (13) and, together with daily goals assessment, may improve the effectiveness of inter-professional communication (14). In addition, the effectiveness of the checklists themselves can be leveraged by systematically prompting physicians and other providers to address omitted items (15).
In the healthcare field, poor communication is often cited as a root cause of medical errors. Effective teamwork and good working relationships can reduce errors and improve outcomes. This relationship between inter-professional communication, quality of care, and patient safety is highlighted in several Institute of Medicine (IOM) reports (16-18).
Prior reports have demonstrated that using a daily goal checklist improves physician-nurse communication and leads to better patient outcomes in the surgical ICU (19), while also facilitating the understanding of work flow and daily goals by residents and nurses, furthermore mutually enhancing communication.
When a campaign of quality improvement was launched on December 15th, 2016, we designed and initiated a daily goal sheet (DGS) as a tool to enhance departmental safety culture in the emergency intensive care unit (EICU), while facilitating team collaboration and communication. The DGS is a one-page checklist with a fixed structure for each day of the week that includes the patient name and diagnosis and the assigned attending physician and nurse. It directs team members to set, for each patient, a clear daily goal concerning care and treatment (20). The DGS assesses patient organ systems, collects interventions, and additionally reminds team members to be attentive to the mutual understanding and communication with patients and family members.
This study was designed to evaluate both the effectiveness of implementing the DGS, and any attitude change concerning physician-nurse collaboration from the April 15th, 2017 to October 15th, 2017.
Methods
Setting
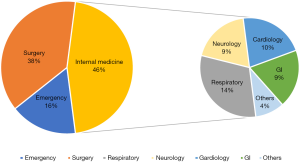
The study was performed in an EICU of 10 beds. The annual population of the patients in the EICU is shown in Figure 1. Our emergency setting averages 498 admissions per year and the majority of patients (73.5%) require mechanical ventilation. The mortality of patients is 2.2% with the average length of stay (LOS) of 4.97 days. All physicians and nurses were informed of the purposes of this study. Questionnaires were administered to 65 regular staff physicians, excluding advanced training physicians and rotating physicians. Fifty-seven valid questionnaires returned completed, with a physician response rate of 87.7%. Similarly, 172 questionnaires were administered to nurses, and 154 valid responses were collected, with a nursing response rate of 89.5%.
Intervention tool
The DGS was designed according to the specific departmental concerns for patients and highlighted each system feature that is habitually and has historically been easy to overlook, which contains 17 categories, includes patient status (sepsis/shock/MODS, CVS, Resp sys, Neuro sys, GI sys, Uro sys, Coagulation/Blood sys, nutrition, infection, tubes in situ and extubation indicators, deep-vein thrombosis (DVT) prophylaxis, sedatives and analgesia, delirium, sleep, rehabilitation, and specific requests from family members. During each day’s morning round, the most senior physician of every medical team was requested to set a daily goal, treatment plan and evaluation parameters, aiming to explore and find the most important clinical needs. The DGS was applied to every consecutive patient within the EICU during morning rounds from December 15th, 2016 to April 15th, 2017.
Survey tool and details
Control studies were conducted before and after the implementation of the DGS. The details were as follows: (I) general information, which included gender, age, educational background, professional rank and title, and number of years of working experience; and (II) Attitudes Toward Physician-Nurse Collaboration to evaluate the attitude to PNC.
These items addressed areas of physician-nurse interaction including authority, autonomy, responsibility for patient monitoring, collaborative decision-making, and role expectations. The scale comprises four dimensions: dimension 1, shared educational and collaborative relationships (items 1–7); dimension 2, caring as opposed to curing (items 8–10); dimension 3, nurse’s autonomy (items 11–13); and dimension 4, physician’s authority (items 14–15). These were answered on a 4-point Likert-type scale (4= strongly agree, 3= agree, 2= disagree, 1= strongly disagree) (21). A higher score meant a reflection of a more positive attitude toward PNC.
Statistical analysis
The raw data were recorded in Microsoft Excel and analyzed by Student’s t-test and Pearson’s correlation coefficient on SPSS 22.0. A P value <0.05 was defined to represent a statistically significant difference.
Results
Item comparison towards PNC before and after DGS
There was considerable statistically significant difference before and after DGS concerning physician and nurse responsibility in item 3 (Table 1).

Full table
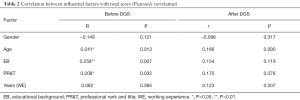
Influential factor comparison before and after DGS regarding PNC
Before the DGS, there was a positive relationship with age, educational background, and professional rank and title towards physician-nurse collaboration attitude. Following the DGS, however, there was no observed significant relationship with gender, age, educational background, professional rank and title, or years of working experience (Table 2).
Full table
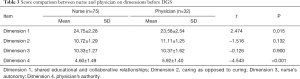
Attitude comparison on each dimension before and after the DGS towards PNC
Statistically significant differences were identified between physicians and nurses on dimension 1 and dimension 4 before DGS, whereas the difference was no longer observed on dimension 1 after DGS (Tables 3,4).
Full table

Full table
Discussion
This analysis demonstrates that the DGS boosts the understanding by physicians and nurses of their responsibilities in teamwork. The recognition degree increased after the DGS in our study on dimension 3, with physician and nurse responsibility being greatly overlapped (Table 1). This is an important finding given that nurses and physicians must be able to rely on each other for optimal patient outcomes. Mutual respect is vital (22), yet physician-nurse disagreements can occur during clinical collaboration due to the differences of s educational backgrounds and work responsibilities, and importantly lack of or suboptimal communication (23). The implementation of DGS in ICU, are extremely important for the whole care team, which can help physicians and nurses focus on important goals and improve documentation of care (24).
A critical patient in an intensive care setting especially requires a clear goal for diagnostic and treatment plans in order to cope with the emergency situation. Since the implementation of the DGS in our emergency setting, the physician-nurse team has been able to convene daily during morning rounds to discuss and set the goal and evaluation target of the working day for each patient. In this way, a centralized and effective care and treatment can begin.
Although the physician and nurse independently work on tasks related to their own duty, the share goal of optimizing treatment effectiveness necessitates close communication concerning patient condition changes, plan or intervention effectiveness, and revision of physician orders. The target set, trace, revision and completion of the DGS facilitates this communication and supervision between the day and night shifts and between the physician and nurse.
Furthermore, the DGS helps lower the interference in physician and nurse interaction due to factors such as age, knowledge base and professional level. Objective bias or disagreement were obviated after the initiation of the DGS, regardless of the age, knowledge and professional factors involved. The collaboration showed a homogeneous attitude between every level of physician and nurse (Table 2); the physician-nurse teams were indeed “on the same page!”
Our tabular daily goal promotes physician and nurse awareness of patient diagnosis and treatment. Being located at bedside, the DGS is highly accessible, which simplifies the interaction of team members. The target goal being clearly expressed during physician or nurse shift changes facilitates the uniformity of patient management between the day and night teams. The DGS also standardizes the workflow of critical care conditions, enabling this by its clear goal and evidence-based improvement records, and by mitigating the effects of opinion bias and communication conflicts.
The DGS also helps enable team members to grow and cooperate. The difference seen on dimension 1 was not noted after DGS implementation, which implies that the shared educational and collaborative relationships between physicians and nurses improved. As such, the DGS promotes sharing of knowledge and working toward a common goal where each professional learns about each other’s roles and responsibilities from each other and helps ensure better communication with fewer chances of error.
The DGS framed a model workflow of the morning rounds, directing physicians and nurses to review every system and highlight those important concerns via the tabular checklist, which included items such as tubes in situ, indicator of extubation, rehab, pressure ulcer, DVT, hospital infection control and prevention, delirium, sedation, analgesia and family members’ special needs or requirements. The targeted goal also guided junior residents and nurses towards conceiving critical patient management as a systematic enterprise.
Practical advice, suggestions for improvement, and constructive criticism for increasing the effective implementation of the goal through team interactions are fully affirmed and encouraged. This attitude facilitates the building of a positive dynamic between physicians and nurses. In the earlier weeks of the DGS in our emergency settings, some physicians in charge first refused to complete the DGS, citing concerns of a greater workload. Soon after the initiation, those physicians reporting being happy to utilize the DGS, as it made them fully aware of patient conditions, while incorporating into their mind a systemic overview of patient-care, which can improve work efficiency and reduce their overall workload. Overall, these benefits helped achieve the realization that while the DGS was compulsory work, it was compatible and contributed to hospital-wide safety culture. Upon being surveyed, all the nurses were satisfied with the implementation of the DGS when the questionnaire was distributed in April 2017. In fact, the nursing team developed a “your favorite physician” award following the DGS implementation for the physicians whose target goals were most clear and cooperation-oriented.
While this novel study prospectively quantified physician-nurse collaboration, our study only focused on the attitude change with the DGS application concerning the physician-nurse collaboration, and it did not closely examine patient quality indicators or outcomes in emergency care settings. The attitude of PNC is crucial in an EICU department that frequent turnover between intensive care and regular care were observed. We standardized the workflow of critical patients through the implementation of the DGS along with multiple policies have been documented since its initiation, including fluid management of patients after emergency surgery, heart rate and blood pressure management of patients with dissecting aneurysm, and blood sugar control orders in insulin pump patients. Further investigation assessing how such changes in physician-nurse collaborations impact patient outcomes is warranted.
In conclusion, this study shows the use of a standardized and individualized checklist of the DGS in an emergency intensive care setting can improve cooperation between physicians and nurses along with building rational consideration and positive collaboration in clinical practice.
Acknowledgments
We would like to thank Xiao Li Yang for authorizing the use of her Chinese Attitudes Toward Physician-Nurse Collaboration.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The name of the ethics committee is Zhejiang Medical University, Sir Run Run Shaw Hospital. The number/ID of the approval is 2015KYB209.
References
- Nkansah NT, Brewer JM, Connors R, et al. Clinical outcomes of patients with diabetes mellitus receiving medication management by pharmacists in an urban private physician practice. Am J Health Syst Pharm 2008;65:145-9. [Crossref] [PubMed]
- Chiarici A, Andrenelli E, Serpilli O, et al. An Early Tailored Approach Is the Key to Effective Rehabilitation in the Intensive Care Unit. Arch Phys Med Rehabil 2019;100:1506-14. [Crossref] [PubMed]
- Schraeder C, Shelton P, Sager M. The effects of a collaborative model of primary care on the mortality and hospital use of community-dwelling older adults. J Gerontol A Biol Sci Med Sci 2001;56:M106-12. [Crossref] [PubMed]
- Ajeigbe DO, McNeese-Smith D, Phillips LR, et al. Effect of Nurse-physician teamwork in the emergency department nurse and physician perception of job satisfaction. J Nurs Care 2014;3:141-8.
- Nadzam DM. Nurses' role in communication and patient safety. J Nurs Care Qual 2009;24:184-8. [Crossref] [PubMed]
- Friese CR, Manojlovich M. Nurse physician relationships in ambulatory oncology settings. J Nurs Scholarsh 2012;44:258-65. [Crossref] [PubMed]
- World Health Organization. Framework for action on interprofessional education & collaborative practice. Geneva: World Health Organization. Available online: Published 2010. Accessed September 20, 2015.http://apps.who.int/iris/bitstream/10665/70185/1/WHO_HRH_HPN_10.3_eng.pdf
- Pronovost PJ, Rinke ML, Emery K, et al. Interventions to reduce mortality among patients treated in intensive care units. J Crit Care 2004;19:158-64. [Crossref] [PubMed]
- Damiani LP, Cavalcanti AB, Moreira FR, et al. A cluster randomized trial of a multifaceted quality improvement intervention in Brazilian intensive care units: study protocol Implementation Science. Crit Care Resusc 2015;17:113-21. [PubMed]
- Hales BM, Pronovost PJ. The checklist–a tool for error management and performance improvement. J Crit Care 2006;21:231-5. [Crossref] [PubMed]
- Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med 2009;360:491-9. [Crossref] [PubMed]
- Pronovost P, Needham D, Berenholtz S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med 2006;355:2725-32. [Crossref] [PubMed]
- Vincent JL. Give your patient a fast hug (at least) once a day. Crit Care Med 2005;33:1225-9. [Crossref] [PubMed]
- Pronovost P, Berenholtz S, Dorman T, et al. Improving communication in the ICU using daily goals. J Crit Care 2003;18:71-5. [Crossref] [PubMed]
- Weiss CH, Moazed F, McEvoy CA, et al. Prompting physicians to address a daily checklist and process of care and clinical outcomes: a single-site study. Am J Respir Crit Care Med 2011;184:680-6. [Crossref] [PubMed]
- Committee on Quality of Health Care in America, Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press, 2001.
- Kohn LT, Corrigan JM, Donaldson MS. To Err is Human: Building a Safer Health System. Washington, DC: National Academies Press, 2000.
- Greiner AC, Knebel E. Health Professions Education: A Bridge to Quality. Washington, DC: National Academies Press; 2003. Available online: Accessed January 14, 2018.http://www.nap.edu/catalog/10681/health-professions-education-a-bridge-to-quality
- Siegele P. Enhancing outcomes in a surgical intensive care unit by implementing daily goals tools. Crit Care Nurse 2009;29:58-69. [Crossref] [PubMed]
- Schwartz JM, Nelson KL, Saliski M, et al. The Daily Goals Communication Sheet: A Simple and Novel Tool for Improved Communication and Care. Jt Comm J Qual Patient Saf 2008;34:608-13. [Crossref] [PubMed]
- Yang XL, Lv HY, Li SG. Comparison of attitudes of physicians and nurses toward physician-nurse collaboration. Chinese Journal of Nursing 2006;466-9. Available online: http://www.cnki.com.cn/Article/CJFDTotal-ZHHL200605043.htm
- Searle C. Professional practice: a South African nursing perspective. Durban: Butterworth, 1987.
- Qolohle MD, Conradie HH, Ogunbanjo GA, et al. A qualitative study on the relationship between physicianss and nurses offering primary health at KwaNobuhle (Uitenhage). SA Fam Pract 2006;48:17. [Crossref]
- Binnekade JM, Brunsveld-Reinders AH, Arbous MS, et al. Incorporation of Daily Goals in Daily Care Planning Does Not Shorten Length of Stay in the Intensive Care Unit. Crit Care Nurs Q 2018;41:178-85. [Crossref] [PubMed]